Your Pharmacy Benefit
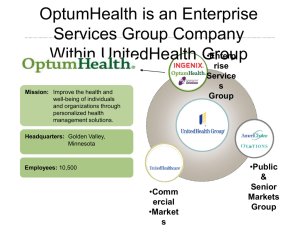
advertisement

•Welcome to Chapter 3C – Pharmacy Coverage •As a reminder, please remember: • All Chapters provided in the 2015 Benefits Guide are intended to be part of a module series •There are eight Chapters, several of which contain sub-chapters • Follow along with and compile these into your own presentation (see below) in the order they are presented • Text items in red are variables. Please modify them as necessary in order to fit your presentation’s and consumers’ needs • Please pick and choose from the slides provided to create a custom presentation that is right for you and your consumers. To do this, refer to the instructions listed on the end slide of each Chapter 1 Proprietary Information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. Pharmacy Coverage Your pharmacy benefit offers you access to: • Affordable medications • • Choice of Pharmacy: • • A number of affordable brand and generic medications Thousands of retail pharmacies, including national chains, many community pharmacies plus the OptumRx® Mail Service Pharmacy 24/7 Personal Support: • Benefit information, savings and lower cost alternatives online or by talking to a pharmacist or benefit specialist 24 hours a day, 7 days a week 2 Proprietary Information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. Looking for ways to lower the cost of your prescription drugs? AFFORDABLE MEDICATIONS Prescription Drug List (PDL) – A list of brand and generic medications approved by the U.S. Food and Drug Administration (FDA) $ Tier 1 $$ Tier 2 $$$ Prescription medications are placed into tiers based on their overall value. Tier 3 Tier levels determine the amount paid when a prescription is filled. Typically generics Exclusions • When lower-cost options are available, the higher-cost option from coverage under the pharmacy benefit may be excluded • If you are taking an excluded medication, check the “Drug Pricing” tool found under “Manage My Prescriptions” on myuhc.com® 3 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. CLINICAL PROGRAMS Promoting safety and appropriate use Notification or Prior Authorization • Requires your doctor to tell us why you are taking your medication in order to determine if you will receive benefit coverage • To start the process talk to your doctor. Once we review the information, we will send you and your doctor a letter to let you know if the medication is covered Supply Limits • A supply limit is the largest quantity of medication covered per copayment or in a time period • Based on FDA guidelines for medication dosage, clinical guidelines or usage patterns Step Therapy • With this program you need to try a lower-cost medication first, before a higher-cost medication may be covered 4 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. FINDING YOUR PHARMACY Access to pharmacy network and OptumRx Mail Service Pharmacy Retail Pharmacy Network • Thousands of retail pharmacies, including large national chains, many community pharmacies OptumRx Mail Service Pharmacy • Receive home delivery of your medication with free standard shipping • Speak to a pharmacist who can answer your questions anytime, any day • Set up text and email reminders to help you remember to take or refill a medication 5 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. OPTUMRx MAIL SERVICE PHARMACY How to Enroll in Home Delivery 6 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. PHARMACY COSTS Retail $ Tier 1 $__ Member Cost Mail Order $__ Member Cost 1-month supply $$ Tier 2 $$$ Tier 3 $__ Member Cost 3-month supply $__ Member Cost 1-month supply $__ Member Cost 3-month supply $__ Member Cost 1-month supply This is the current copayment/coinsurance structure of the plan in effect today. These amounts are subject to change. 7 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. 3-month supply YOUR PERSONAL RESOURCES We provide resources available to help you anywhere, anytime Visit www.myuhc.com to manage your prescriptions, look up nearby pharmacies, and access the PDL list Our mobile website provides text messages and medication reminders in addition to our web resources Call the number on the back of your ID card for 24/7 call support to answer pharmacy and medical questions 8 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. SPECIALTY PHARMACY We focus on you and the total condition, not just drug utilization Conditions Include: Cancer, Hemophilia, Hepatitis C, Multiple Sclerosis, Rheumatoid Arthritis, HIV and more Services: • 24/7 access to pharmacies, providing support focused on you • Adherence and clinical programs to help you better manage your condition • Proactive reminders and timely delivery • Online support and medication information for you Our Specialty Pharmacy Program provides the resources and the condition-specific support you need to help you manage your complex conditions and achieve your best health. 9 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. PHARMACY PAYMENT PROCESS 1 Present health plan ID card to pharmacy. 2 Pharmacy verifies eligibility and any amount you owe at the point of sale. 10 Confidential property of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. 3 You pay your member cost responsibility for medications covered under your pharmacy benefit. MAIL SERVICE MEMBER SELECT If you are currently taking medication on a regular basis – you have an important decision to make. • Effective 1/1/2015, you are already enrolled in Mail Service Member Select and can begin realizing the benefits of home delivery immediately. • You must choose to either fill your maintenance medication through the OptumRx Mail Service Pharmacy or through a retail pharmacy. • If you choose a retail pharmacy you must disenroll from Mail Service Member Select. • Mail Service Member Select allows you two retail pharmacy refills of your maintenance medication before you have to decide. • If you do not take action after the second retail fill you will pay 100% of the drug cost until you make a decision. • If you choose not to take advantage of the mail service pharmacy and disenroll, you may continue filling medications at a retail pharmacy for your standard copay or cost.. 11 Proprietary information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. SELECT DESIGNATED PHARMACY Participants choose one of three options to continue receiving network benefits A Move to a lower-cost medication and save up to $480 per year Saving you and your members money There are often many medications that treat the same condition. Members should consider a lower-cost option. Average employer savings Use mail service and save up to $90 per year B Members who want to keep taking their current medication can -- through the convenient mail service pharmacy. $0.63 PMPM Average member savings Do both and save up to $500 per year C For the most savings, use a lower-cost medication and mail service. $360 annually Members on affected drugs who have non-network benefit coverage and choose to make no change will pay the full cost of the drug, and can file a paper claim for reimbursement as an non-network benefit. Potential savings estimates are based on UnitedHealthcare typical benefit designs and are calculated based on an average 30-day supply for retail or a 90-day supply for mail service. Actual savings may vary. Average savings based on BoB plan results from Q1-Q3 2012. 12 Proprietary information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. SELECT DESIGNATED PHARMACY Member Engagement Helping members understand their choices Letters explaining the program (after grace fill #1) Automated phone call about the program (after grace fill #1) Point-of-sale message, delivered by the pharmacist (after grace fills #1 and #2) 13 Proprietary information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. SELECT DESIGNATED PHARMACY Advantage PDL Program Medications 14 Proprietary information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. SELECT DESIGNATED PHARMACY Traditional PDL Program Medications 15 Proprietary information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group. •This ends Chapter 3C – Pharmacy Coverage •Please open Chapter 4A – Choice Plus Plan •Copy and Paste slides from Chapter 4A to this Power Point (Chapter 1) 1. Click on the first slide and then press shift while you click on the last slide 2. Right click on the first slide and select copy 3. Go to the first section 4. Click below the thumbnail of the last slide in that section 5. Right click there and select Copy—Use Source Formatting •Whichever slides from Chapter 4A that do not apply to your customer, delete 16 Proprietary Information of UnitedHealth Group. Do not distribute or reproduce without express permission of UnitedHealth Group.