Chapter 18- The Heart
advertisement

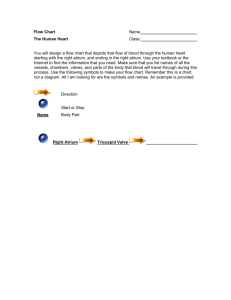
The Heart Chapter 18 Anatomy 32 Emotions do not come from the heart, it may feel as if they do because emotions affect heart rate. The purpose of the heart is to pump blood either to the lungs through the pulmonary circuit or through the body via the systemic circuit. I. Location and orientation within the thorax The heart is the size of your fist and weighs less than a pound. It began beating 22 days after conception and continues to rhythmically contract until the times dies. It is located in the thoracic cavity posterior to the ribs and just superior to the diaphragm. It is position so the apex points to the left and anterior to the rest of the heart. The base faces posteriorly. The perimeter of the heart lies within four points. As a clinician it is important to know these points in order to distinguished a normal size heart from an enlarge heart. See page 501 Fig 18.11 Superior left point- at costal cartilage of second rib about an inch lateral to the sternum Inferior left point- fifth intercostals space at midclavicar line Superior right point- costal cartilage of third rib connects to sternum Inferior right point- costal cartilage of sixth rib about an inch lateral to sternum II. Structure of the heart The description begins with the most superficial layers and works to the deepest layers. • A. Coverings- The heart is enclosed by a serous membrane that has three layers: • 1. Fibrous pericardium- outer layer, it adheres to the diaphragm and holds the heart in place. – Serous pericardium- layer below the fibrous pericardium composed of the parietal and visceral pericardium. – 2. Parietal pericardium- adheres to the inner surface of the fibrous pericardium and forms the parietal cavity that is filled with serous fluid. – 3. Visceral pericardium- also called the epicaridum, it lies just above epicardium (heart muscle) • B. Layers of the heart wall- cardiac muscle can be distinguished into three layers: – Epicardium- superficial, comes in contact with epicardium, holds fat – Myocardium- middle muscular layer, contracts to move blood – Endocardium-deepest layer, composed of endothelial cells it lines the chambers, and make the valves. C. Heart Chambers- Interiorly, the chambers are divided into left and right sides by the interatrial septum or inventricular septum. Exteriorly the separation of atria and ventricles is indicated by the coronary sulcus (crown) and ventricle separation is indicated by the anterior and posterior interventricular sulcus. Atria have thinner walls because the apply less force when contracting than ventricles which must work against gravity. Anterior Exterior View of The Heart Posterior Exterior Heart • 1. Right Atrium- a top chamber that receives blood low in oxygen coming from upper and lower body via the superior and inferior vena cava and coronary sinus. Superficially the atrium has the right auricle. The anterior wall has folded muscle ridges called pectinate muscles. The fossa ovalis indicates the area at which the fetal heart had an opening. The atria opens into the ventricle through the right atrioventricular valve (tricuspid). • 2. Right Ventricle- a lower chamber that receives blood from the right atrium. The interior had ridges called trabeculae carneae and extending muscles called papillary muscles which have the chordae tendineae. These are connective tissue bands that attach to the AV valve flaps (cusps) and help to keep it from folding into the atrium when the ventricle contracts. When the ventricle contracts it send blood out to the lungs, first trough the pulmonary semilunar valve then via the pulmonary artery • 3. Left Atrium- upper chamber that receives oxygenated blood coming from the lungs via the pulmonary vein. It also contains pectinate muscles. It opens into the ventricles through the left atrioventricular valve (mitral or bicuspid valve). 4. Left Ventricle- lower chamber that receives blood from the left atrium. It forms the apex of the heart and has the same characteristics as the right ventricle. When it contracts, blood flows through the aortic semilunar valve and then to system circulation via the aorta. It’s wall is three times thicker than right ventricles because the system circulation is larger then pulmonary circulation. • • • • • • • • • • • III. Pathway of blood through the heart. A. This is the path that blood takes as it travels trough the pulmonary and systemic circulatory paths. 1. Blood empties into the right atrium through the inferior and superior vena cava and coronary sinus. 2. The atrium sligthly contracts and blood moves past the right atrioventricular valve (triscupid) into the right ventricle. 3. The ventricle fills with blood and contracts sending blood out of the heart as it passes through the pulmonary semilunar valve into the pulmonary trunk and then right and left pulmonary artery. 4. The pulmonary arteries carry the blood into the corresponding lungs where it eventually becomes oxygenated. 5. Oxygenated blood leaves the lungs and heads towards the heart via the right and left pulmonary veins. 6. The blood empties into the left atrium filling the chamber. The atrium slightly contracts as blood passes through the left atrioventricular valve (mitral or biscuspid) leaving the chamber. 7. The left ventricles fills with blood and powerfully contracts to send blood past the aortic semilunar valve into the aortic arch. 8. The aorta branches sending blood into all areas of the body (systemic circulation). B. Heartbeat is the sequence of atrial and ventricular contraction. Resting heart rate is 60-80 beats per minute. When the heart contracts it is called systole (associate stress=contraction) and when it relaxes it is called diastole (associate dialate= open= relax). Most often systole and diastole refers to the times when the ventricles contract or relax. IV. Heart valves These are thin structures composed of endocardium designed to prevent back flow of blood into the chambers. A. Valve structure- the flaps are thin and shaped like crescent moons. Each valve has two or three cusps: • Right atrioventricular valve (tricuspid valve)- three cusps • Left atrioventricular valve (bicuspid or mitral valve)- two cusps • Aortic semilunar valve- three cuspids • Pulmonary semilunar valve- three cuspids B. Valve function- The atrioventricular valves prevent blood from flowing back into the atria when the ventricles contract. The semilunar valves prevent blood from flowing back into the ventricles. C. Heart sounds- closing of valves causes vibrations that can be interpreted as sounds. The “lub-dub” is the familiar sound to describe heart beat. The “lub” is the closing of the AV valves. The “dub” sound is produced by closing of the semilunar valves. Because the valves do not close simultaneously it is possible to distinguish when each is closing. To listen to each valve the stethoscope should be placed at different locations (pg 511). • V. Fibrous Skeletondense connective tissue lies throughout the heart and serves the following functions: • • 1) anchor valves 2) prevent overdialation of valves 3) serves as insertion points for cardiac muscle 4) prevents direct electrical impulse travel from atria to ventricles. • • • VI. Conduction system and innervation• This section addresses how the heart generates electrical impulses and conducts rhythmic contractions. • A. Conducting system- cardiac muscle cells generate impulses that signal rhythmic contractions independent of nervous control. They control the sequence at which the chamber contract- thus establishing the basic heart rate. The component are: • 1. Sinoatrial node- starting point, lies in superior wall of right atrium, it is the pace maker, it sending out 70-80impulses per minute. • 2. Internodal fibers- fibers that transmit the impulse between SA and AV node • 3. Atrioventricular node- heart cells, specialized mass of conducting cells located in the interatrial septum. This is the site where signal is delayed so ventricles fill. • 4. Atrioventricular bundle (bundle of his)- heart cells that carry an impulse to the interventricular septum. • 5. Bundle branches (left/right)- heart cells that carry an impulse from the interventricular septum and become perkinge fibers. • 6. Purkinje fiber- long barrel like muscle cells specialized for conduction, they are located at a deep level and terminate at the apex where contraction of ventricles begins • • • B. The path of impulses travels is as follows: SA node – spread through cardiac muscle causing contraction—some travel down internodal pathway—to – atrioventricular node—to – atrioventricular bundle—to interventricular septum—to purkinje fibers towards apex. This initiates contraction at the apex. C. Innervation- heart rate is altered by nervous system control. The nerve fibers that reach the heart are parasympathetic and sympathetic fibers. They enter the heart plexus and branch to innervate all heart muscles, although most of the concentration is at the SA and AV node. • D. Blood supply- the heart muscle requires its own set of blood vessels to nourish the cardiac tissue. From the base of the aorta comes the right and left coronary arteries. The left coronary artery divides into anterior interventricular and circumflex arteries. The right coronary artery follows the coronary sulcus and branches into the marginal artery and posterior interventricular artery. Cardiac veins carry blood low in oxygen to the heartgreat, middle, and small cardiac vein empty into the wide coronary sinus that empties into the righ atrium. Some anterior cardiac veins empty directly into the right atrium. VII. Disorders of the heart • A. Coronary artery disease- caused by atherosclerosis (accumulation of fatty deposits), the arteries supplying the heart muscle become clogged causing chest pain. The heart cells are weaken by reduced oxygen amounts causing a pain called angina pectoralis. The pain can also come from stress spasm. A heart attack occurs when the cardiac cells die (myocardial infarction). Cardiac arrest may cause death in a third of the cases. Coronary bypass surgery restores blood supply to heart tissue. Silent ischemia is a painless silent fatal heart attack • B. Heart failure- weakening of the heart because it cannot pump at a rate adequate enough to keep up with the bodies oxygen demand. It can result form a heart attack, improper filling of ventricles, or congestive heart failure. • C. Disorders of the conduction system- these relate to heart arrhythmiaabnormal rhythums. – Ventricular fibrillation- random firing of electrical impulses allow for improper filling of ventricles, can cause cardiac arrest. – Atrial fibrillation- random stimulation of AV node signals by multiple signals in atrial myocardium ventrals. This causes ventricles to contract quickly and irregularly potentially forming blood clots. The clots can cause strokes. • D. Congestive heart failure- enlargement of the heart causing pumping inefficiency. Sometimes the right ventricles enlarges due to high pressure in the pulmonary circuit ( cor pulmonale) The heart beats after 22 days and the atrium are interconnected up until birth.