Mail Order Stories
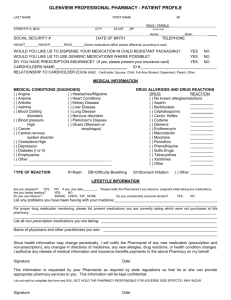
advertisement
Case Studies related to Mandatory Mail Order Pharmacy in New York State In 2012 NYS Insurance Law was changed so that consumers would not be forced to get prescription drugs through the mail if they preferred to obtain them from a local participating pharmacy. But the new law is not working. Consumers are being forced into mandatory mail programs. Why the law is not working for consumers: Pharmacy Benefit Managers (PBM’s) have ‘terms and conditions’ that that local pharmacies cannot meet - Requirements such as: Costly accreditations that favor large out-of-state pharmacies that are owned by Pharmacy Benefit Managers Accreditations designed to protect mail order pharmacies and discriminate against community pharmacies Insurance requirements such as $5 million policies when the norm is $2 million On-call nursing services, 24 hours per day, 365 days per year Prescriber surveys and other data collection Consumers have not been notified how the law applies to their health insurance coverage Consumers do not have a way to appeal mandatory mail Mandatory enrollment into “special” programs that are exclusively mail Participating local pharmacies that agree to meet the same price as mail order have been blocked with: Claims that cannot be processed for certain “excluded” drugs Terms and conditions that do not reasonably apply Termination from the existing network as a pre-condition New rules and procedures (i.e. must be requested in writing by the consumer) 1 Client Insurance Pharmacy Benefit Manager 1 United Health Care Optim Rx (formerly Prescription Solutions) 2 Blue Cross Blue Shield CuraScripts 3 Blue Cross Blue Shield CuraScripts 4 United Health Care Optim Rx (formerly Prescription Solutions) 5 United Health Care Optim Rx (formerly Prescription Solutions) 6 Blue Cross Blue Shield CuraScripts 2 Status of Mail order: Exempt/Still enrolled/ Enrolled denied exemption Exemption granted #1: Client Code: _________ Service Provider assisting Client: GMHC Date of complaint to service provider: June 2013 Health Insurance: United Healthcare Pharmacy Benefit Manager: Optim Rx (Prescription Solutions) Was a hardship exception sought?: Yes Was it approved: Initial: No On appeal: No Was the Case Resolved? Unknown If so how: _________________ Client Story I have been with Prescriptions Solutions, a mail order pharmacy, for about a year. I have been with them since my company switched their insurance to United Healthcare. Every month, I have to communicate with them on the phone to reorder my prescription. Though this is time consuming and an annoyance, overall everything was fine. Around the holiday time my meds didn’t arrive. Prescription Solutions has no policy or procedure in these situations to replace the order. I called them to work something out so I could maintain compliance with my treatment regimen, but on the phone they were completely unyielding to accepting any burden of responsibility. This left me high and dry for my medication. I called to speak with the upper management, and was still met with an unwillingness to help me out. I had to wait until the next month’s order cycle when I could reorder this medication—about three weeks after this incident. In addition to calling the mail order pharmacy, I called this doctor. The doctor said he could prescribe more medication, but insurance wouldn’t cover it. My medication is incredibly expensive and I cannot afford it. I had no choice but to wait until he could reorder from the pharmacy. I am normally 100% drug adherent and was incredibly affected by this incident. In those 3 weeks I was in a constant state of getting sick, which is highly unusual. I had three colds and the flu. I couldn’t get the sickness out of my system. I had never experienced that before. In all my years, I’ve never experienced anything like this. If I were still with my neighborhood pharmacist, this would not have happened. If for some reason my HIV medication was not found, they would work on getting me new meds. This mail order pharmacy that I was forced to switch to has compromised my health. I am now on COBRA and that will end by February. I am nervous about what is going to happen after that. 3 #2 Client Code: _________ Service Provider assisting Client: GMHC Date of complaint to service provider: June 2013 Health Insurance: Blue Cross Blue Shield Pharmacy Benefit Manager: CuraScript Was a hardship exception sought?: Yes Was it approved: Initial: No On appeal: No Was the Case Resolved? No If so how: _________________ Client Story In November, BlueCross BlueShield gave me an ultimatum that I had to switch to Curascript or they would stop my medication. I received a phone call from my pharmacist at Community Walgreens who is the pharmacy that I have been using for over 15 years now. My pharmacist said that this will be the last month that I will be able to use them for filling COMPLERA. He said he can override this one time prescription this month, but next month I will have to go through CuraScript mail order. This is adding stress, inconvenience and confusion for me. Why do I have to start mail order when presently I use Community Walgreens who send me my meds via FedEx because I live up here in Plattsburgh, NY since 2009. Now I will have to deal with another company to get medication? This is wrong. BlueCross BlueShield’s new third party, CuraScript, is only adding inconvenience for me. I called them to set up an order system with them to refill my prescriptions. I was on the phone for two hours! She kept asking me to verify my birthday and put me on hold, and after a half hour on hold the representative would ask me information she already asked me. They told me that I would have to start paying copays. After two hours I ran out of patience and time. I told her I didn’t have time to deal with this and hung up. No one followed up and I have yet to find out if they will order my prescription. 4 #3: Client Code: _________ Service Provider assisting Client: GMHC Date of complaint to service provider: June 2013 Health Insurance: Blue Cross Blue Shield Pharmacy Benefit Manager: CuraScript Was a hardship exception sought?: Yes Was it approved: Initial: No On appeal: No Was the Case Resolved? _____ If so how: _________________ Client Story I am a longtime GMHC client, currently covered by a BlueCross HMO policy arranged for me by GMHC when I was about to lose my insurance about a decade ago. My premiums are paid by ADAP (for the moment). Blue Cross has (admittedly with some warning) refused to pay for my prescriptions due for renewal unless I obtain them from their mail-order source. I live in an old Manhattan building with no doorman and no bells or buzzers. I am unable to receive packages at home. Even if such service was provided at my residence I couldn't, as I am an outside salesperson and I am simply never at home during business/delivery hours. I work entirely alone, have no family in NYS and have no alternative address to which I could send sensitive confidential materials such as my medical prescriptions. Certainly, no one in my professional circles is aware of my status, and it would be extremely compromising should they become aware of it. Moreover, I have gone to the same local pharmacist, who has evening and weekend hours, for close to 30 years and rely upon his advice and assistance as well as his accommodating schedule. In fact, I tried this mail-order service several years ago -- my package was lost in shipment and not located for 3 months because they were unable to deliver it; I had extreme difficulty obtaining my needed medications during that interval. I have tried to follow the developments negotiated among the various parties subsequent to the passage of Governor Cuomo's prescription choice law, but I don't understand how it applies to my situation. My insurance is private, although paid through ADAP, so it is effectively analogous to Medicaid coverage, as far as I can see. ADAP has however declined to discuss the matter with me. I may moreover soon be taking over my own premiums, and were I to do so would the criteria that apply to me differ? My prescription will run out next week, we will see what happens. By way of update: I had to go through two separate mail order entities to place the mail orders for my prescriptions. Total time spent on the phone was approximately 2.5 hours. 5 Since I had no way of receiving packages at home, I had to have deliveries made to my work location. As there is no one there to sign for packages, and they will arrive in two shipments, I will have to schedule two entire work days to sit here and wait for the deliveries. As I am an outside salesperson and really only work on the road, this is a complete waste of my time and significant inconvenience. I will have tracking information for one, but no idea when during the day it may arrive, and for the second I just have no idea at all, but apparently it won't require a signature so I assume they will just leave the package sitting on the sidewalk outside my office door. Once the second order was placed and my credit card charged (what do people do who don't use credit?) I was forced to wait an additional 30 minutes on hold to talk to a "nurse." Her level of expertise was demonstrated by the fact that she was unable to pronounce the names of either of my medications. It turned out that her responsibility was to tell me what the dosage schedule is, which as I have already taken these medications for fifteen years, was not information that I needed to wait 30 minutes on hold to have reiterated to me. The only conceivable benefit of this is that they did approve 90-day shipments, so I will only have to take 8 days off from work per year to wait for my deliveries. Needless to say, after my experience with their "nurse"-expert, I won’t bother seeking any further advice from them. 6 #4: Client Code: _________ Service Provider assisting Client: GMHC Date of complaint to service provider: June 2013 Health Insurance: United Health Care Oxford Pharmacy Benefit Manager: OptimRx (formerly Prescription Solutions) Was a hardship exception sought?: No Was it approved: Initial: No Was the Case Resolved? _____ On appeal: No If so how: _________________ Client Story I take a lot of medications. It’s a pain. I used to get all of his prescriptions at Rite Aid. I had a great relationship with them. It was very personal and very easy. They know me, I know them. I’ve been going there since 2009. I enrolled in OptumRX (used to be Prescription Solution) in September 2011 because my insurance company, Oxford, made me. It took a long time to enroll me because they needed to get fresh prescriptions from the doctor. They did not allow me to help and insisted they would take care of getting the prescriptions. The initiative to refill my prescription was in their hands, but it took them a long time to do it. I was persistent in reminding them, and still it took a month to get! It was by sheer luck that the new medication arrived on the same day that my old prescription ran out. Once it arrived, they sent me the wrong medication completely! I have no idea why; maybe the doctor gave them the wrong prescription. But, if this was the case, I told them what I was on, so they should’ve consulted with me before sending it. That’s what Rite Aid would do. I sent the wrong one back and they replaced it with the right prescription. I was tenacious, so luckily, they got it within the same day. This system worked without complications for a while. No question it is definitely an annoyance. Every month I have to call and reorder. It’s a least a 15 minute phone call. I talk to a different person each time so they always got through all the security checks and go through the medications (like take this 2x a day). Randomly they’ll call me and then put me on hold. Then a sales assistant will come on and ask “How can I help you?” Recently they’ve offered to reach out to my doctor to refill my prescriptions. When I refilled them, I used to refill them all at the same time, but now they messed up the cycle. Three prescriptions got approval for five weeks and one got approval for three. They said they would take care of refilling the prescription and, once again, they didn’t. I got a call saying they wouldn’t refill the prescription because no one placed the refill to my doctor- I was confused and frustrated. They say they’ll refill the prescription, but then they don’t. Three of the prescriptions I have received, but because they messed up my refill cycle, one of them is about to expire. With these 7 types of medications (HIV/AIDS medications), they NEED to order them with no complications. It’s all the worse for the recipients if it’s the wrong prescription or it’s late. It would be nice if they had an automatic refill option, or at least said when they needed to refill the prescription, perhaps a calendar or something. They should also confirm when they order your prescription. I can certainly say that if I didn’t push them, these things would take a lot longer. 8 #5: Client Code: Unknown Service Provider assisting Client: GMHC Date of complaint to service provider: 2013 Health Insurance: United Health Care Oxford Pharmacy Benefit Manager: Optim Rx (formerly Prescription Solutions) Was a hardship exception sought?: Yes Was it approved: Initial: Unknown On appeal: Unknown Was the Case Resolved? Unknown If so how: Client Story I was diagnosed with HIV three years ago. I never experienced a delay in medication. In November, Oxford switched me to the mail order system. Since then there have been some problems. Currently, I haven’t had my medications in a few days. This is the third time this has happened in three months. Part of this problem is their delivering. It has to be delivered to work so someone can sign for it but they had the wrong address. They were good about calling to rectify the situation, but there is an overall lack of communication between the mail order pharmacy and the client. When I call them to communicate it’s not too bad. There is also always a concern for drop off—who is liable, them or you? Overall, it’s been a below average experience being on the mail order pharmacy. I’ve missed doses- that would’ve never happened with an old pharmacy. My old pharmacy would never allow for a prescription to run out, they would be proactive. This mail order pharmacy is not. They are apologetic, sympathetic even but ultimately, the mail order system for some medications is really silly. It’s really dangerous to miss HIV medication. I just think they have an inefficient and problematic system. They have to reach out to me to refill the prescription. This would be ok if they do that, but they don’t and if they do it is not in a timely manner. I can’t reach out to them to fill my prescription. I’ve tried, and my in-person pharmacies have been working to improve this process but they haven’t been successful. Update: My insurance switched specialty pharmacies without telling me. I am running out of medication and don’t know who to call and if they are going to refill my prescriptions. I have had to go to the doctor multiple times this week to get a shot that normally I give myself and pick up various medications. This is incredibly annoying and inconvenient. 9 #6: Client Code: SCHC08 Service Provider assisting Client: GMHC Date of complaint to service provider: 2013 Health Insurance: Blue Cross Blue Shield Pharmacy Benefit Manager: CuraScript Was a hardship exception sought?: Yes Was it approved: Initial: Yes On appeal: No appeal Was the Case Resolved? Yes If so how: Blue Cross Granted an exemption based on agreement they reached with the Attorney General’s Office. Client Story I am a long-time AIDS survivor (I tested positive for HIV in 1985 when the test for the virus became available and I received an AIDS diagnosis in 1992). I have had my prescriptions filled at my local retail pharmacy, which has many customers with HIV/AIDS, for over a decade. Beginning in 2013 my private insurer, Empire Blue Cross, mandated that I order so-called “specialty” medicines, including my HIV medications, through its mail order pharmacy (then known as CuraScript). This mandate created enormous problems for me in filling certain prescriptions. In one instance, the mail order pharmacy delayed filling a prescription for a type of Human Growth Hormone (used, among other things, to combat AIDS wasting and lipodystrophy in people with AIDS) because it required special internal documentation. It also spent several weeks seeking additional information from my doctor because he prescribed the medicine in a lower dosage than it usually dispensed it. After finally clearing up the dosage issue, it turned out the mail order pharmacy did not even carry the particular brand my doctor prescribed. When my doctor ordered a brand the pharmacy did carry, its record of the first prescription kept it from filling the second. It took a couple of months to resolve the issue. A mistake was also made that for no reason simply voided my prescription of the HIV medicine Stribild. The mail order pharmacy did not contact me to tell me there was a problem with either of the above prescriptions. My local retail pharmacy would have informed me there was a problem either by calling me or when I came into the store. (In the past, I have been able to facilitate resolutions with my local retail pharmacy. Mistakes happen.) In contrast, it is the procedure of the mail order pharmacy only to deal with the doctor’s office concerning prescriptions. Indeed, if I had not scheduled a delivery for my Stribild before I had run out of the medicine and not double-checked on why it had been delayed, I would have had to arrange for an emergency dosage either through a hospital or through a same-day insurance over-ride. Because of these problems with the mail order pharmacy, Empire Blue Cross -- to its credit -granted me a “hardship exemption” to having to use their mail order pharmacy and I can now get my prescriptions filled at my local retail pharmacy. It is important to highlight how the mandate to use a mail order pharmacy takes the patient out of the loop regarding drug delivery and interferes with the speedy implementation of medical decisions I make with my doctor. As a patient I prefer to review my prescriptions for medica- 10 tions. I not only can head off any mistakes, but I gain the psychological benefit of being a proactive patient. And while I can see my doctor, get a prescription, and have it filled at my local retail pharmacy all in the same day -- using a mail order pharmacy requires information to be transmitted from the doctor to the pharmacy, playing phone tag with the mail order pharmacy to schedule a delivery, and then waiting at least 24 hours more for delivery (excluding Sundays and holidays). Finally, and perhaps most importantly, the mandate to use a mail order pharmacy disrupts the trusting relationship I have with my local retail pharmacists. My local retail pharmacists know all the “specialty,” non-”specialty,” and over-the-counter drugs I take. I often request confidential advice about how to deal with side effects, for example. My pharmacists also play a unique role in my support system. My social sphere has become extremely limited over the years. Although I speak to friends and family often, I go to my local retail pharmacy several times a week. Going to the pharmacy literally gets me out of the house and breaks my isolation. My pharmacists are aware of my bouts of illness and hospitalizations and they assess my health and well-being based on visible cues. They tailor their conversation to buck me up or to pass on information about programs of drug manufacturers that assist with co-pays of private insurers, empowering me to continue coping with the challenges of having of AIDS. 11