5. 5-FU 5% Vs 5-FU 5% + INF
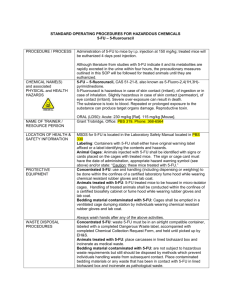
advertisement

Also known as condylomata acuminata or venereal warts, is one of the most common types of sexually transmitted infection and primarily affect younger people. The disease usually is caused by HPV genotypes 6 or 11, which normally are not involved with cancers but can cause abnormal pap smear. In 8 to 14%, the person has been infected with more than one type of HPV 50 to 80 percent of sexually active women are infected at least once in their lifetime. Transient or undetectable Women under 25 to 30 years have higher rates of infection although a second peak has been described in postmenopausal women. Association with HPV genotypes 16 and 18 can give rise to subclinical lesions associated with CIN and squamous cancer. Approximately 1 million cases of genital warts occur each year in the United States and an estimated 32 million cases occur worldwide. In women, genital warts can appear on the vulva, the walls of the vagina, the perianal area, and the cervix. May increase in size during pregnancy. In men, they may be found on the tip or shaft of the penis, the scrotum, or the anus. In neonates, respiratory & laryngeal papillomatosis follows NVD but can occur after C/S. Typically presents between 2 & 3 years of age and extends into adolescence. About 37% of laryngeal papillomatosis become malignant. Occurs more commonly in first-born children and in the children of young mothers who had genital warts. 100 types of HPV ( double stranded DNA virus) Viral replication takes place only in fully differentiated epithelium. Cutaneous and mucosal types, High, intermediate and low risk types Papule or plaque can also remain dormant within epithelial cells without visible disease HPV type 2 on hands and feet Benign lesion: the viral genome replicates separately to the host cell’s DNA. Malignant lesion: the HPV DNA is integrated into the host cell’s chromosomes. After integration a series of events leads to deregulation of the E6 and E7 genes of HPV. 5 - Fluoruracil (5-Fu) Bichloroacetic or Trichloroacetic Acid Cryotherapy Surgical Excision or Curettage Cautery Imiquimod Interferon CO2 Laser Podophyllin Podophyllotoxin Vacinne Antimetabolic Tissue Chemical Destruction Physical Freezing Surgical Removal Tissue Physical Destruction Immunomodulator Antiviral(immunomodulator) Tissue Vaporization Antimitotic Antimitotic Antiviral(immunomodulator) Claudio S Batista, Álvaro N Atallah, HumbertoSaconato, Edina MK da Silva 2010 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd. Types of studies, Only randomized controlled trials (RCTs) were included in this review Types of participants, Women and men aged 18 years or more, nonimmunocompromised, with clinical or subclinical genital warts. 5-FU Vs placebo 5-FU 5% Vs Meta-cresol-sulfonic Acid (MCSA) 5-FU 5% Vs Podophyllin 5-Fu 5% Vs CO2 Laser 5-FU 5% Vs 5-FU 5% + INF -2a (Low dose) 5-FU 5% Vs 5-Fu 5% + INF -2a (High dose) 5- FU 5% Vs 5-FU 5% + CO2 Laser + INF -2a (High dose) 5-FU 5% + CO2 Laser Vs CO2 Laser plus Primary Outcomes • Patient or warts response: cure or partial improvement • Recurrence rate Secondary Outcomes • Local reactions • Other related adverse events (alteration in lab data) Botacini et al, 1993,5% vag. gel 5 gr Qod x15 Females with HPV infection 64 Vs 16 The outcomes after 12 wks Rx were: Cure(-ve colpo, pap & Bx): 52/64 vs 5/16 * Partial response (only+ve cyto): 7/64 vs 1/16 No response: 5/64 vs 10/16 * 0.02 Syed at al, 2000, 1% vag. gel 4 gr Qod x4 wks 30 females in each group with intravaginal warts 312 genital warts: 162 Vs 150 The results were: Cure (Nl colpo & -ve HPV): 25/30 Vs 4/30 * 0.02 side effects : 2/30 Vs 1/30 Lesion recurrence : 2/30 Vs 1/30 Warts cure:141/162 lesions Vs 21/150 * 0.0001 Low index of side effects ( local Rxn, dysuria & local hypersensitivity ) Weissmann et al, 1982, 0.5% gel. Anogenital warts 59 patients: 30 male (14 Vs 16) & 29 female (16 Vs 13 ) The results were: Cure: 18/30 patients (10/14 male & 8/16 female) Vs 8/29 patients (4/16 male & 4/13 female) * 0.031 Improvement: 6/30 patients (2/14 male & 4/16 female) Vs 4/29 patients, (1/16 male & 3/13 female), No response: 6/30 patients (4/14 male & 2/16 female) Vs 17/29 patients (8/16 male & 9/13 female). * 0.0068 Data from these 3 studies Botacini 1993; Syed 2000; Weismann 1982 could be pooled but demonstrated heterogeneity (I 2= 62%). [RR 0.39 (95% CI, 0.23 -0.67)]. NNT = 2 Botacini et al, 1993, all females 74 patients Vs 9 (MCSA Qod x30 days) Results after 12 weeks were: Cure: 52/74 Vs 3/9 * Partial response: 7/74 patients Vs 1/9 No response: 15/74 patients Vs 5/9 * 0.0075 Botacini et al, 1993, all females 74 pts 5-FU 5% gel (2/wk x8 wks), 40 pts Podophyllin 2% (vag.gel 5gr Qod x15) 5 pts Podophyllin 4%. (vag. gel 5gr Qodx15) The results after 12 weeks: Cure: 52 patients /19/ 3 * Partial response: 7 patients/5/1 No response: 15 patients/16/1 * 0.039 Wallin et al, 1977, All males 42 male patients:20 patients(cream qhs x2w) Vs 22 ( solution by doctor weekly x 4) Withdrawals: 2 Vs 3 The results after 4 and 9 weeks. Cure after 4 weeks : 10/18 patients Vs 11/19 0.89 Cure after 9 weeks: 6/18 patients Vs 10/19 Recurrence of lesions p less than 0.00001 Data from two studies (Botacini 1993; Wallin 1977) could be pooled and did not demonstrate heterogeneity (I2 = 32%). [RR 1.26 (95% CI, 0.86 - 1.82)]. NNT = 6 Relakis, 1996, performed 3 study groups all males Condyloma Acuminatum (CA): cream qhsx5, if no response other 3 courses, Condyloma Plain (CP): single dose Condyloma acuminatum & plain (CA+CP): single dose The only studied outcome was Treatment Failure. Lesion Recurrence observed in the first year after treatment was considered as Treatment Failure Side Effects were observed in 11% of the patients treated with 5-FU In CA group, 33 males Vs 12 Treatment Failure was: 8/33 Vs 4/12 0.53 In CP Group, 156 males Vs 39 Results were: 29/156 Vs 12/39 0.085 In CA + CP Group, 29 males Vs 20 Results were: 14/29 Vs 14/20 0.12 Relakis et al, 1996, all male patients 5FU 2 courses x 5 days + INF 1.5 SC x 6 days In CA group: 33 Vs 27 Results were 8/33 Vs 7/27 0.88 In CP group: 156 Vs 18 Results: 29/156 Vs 2/18 0.34 In CA + CP Group: 29 patients Vs 0 Results 14 patients Relakis et al, 1996, all males 5FU 5% cream 2 courses x 5days + INF 3 IU SC x 6 days In CA Group: 33 Vs 0 Treatment Failure in 8/33 In CP Group: 156 patients Vs 58 Result: 29/156 Vs 1/58 In Ca + CP Group : 29 Vs 0 Result: 14/29 patients Relakis et al., 1996, All males CO2 laser after 2 courses of 5FU cream In CA group: 33 Vs 30. Results: 8/33 patients Vs 0/30 0.056 In CP group: 156 Vs 20 Results: 29/156 Vs 1/20 0.18 In CA + CP group: 29 Vs 16 Results: 14/29 patients Vs 3/16 Treatment failure * 0.00001 Carpinello et al., 1988, all males 5FU 5% one wk after Laser x 30 days 68 patients, 41 Vs 27 The outcome studied was Lesion Recurrence Even one lesion after treatment Results: 28/41 Vs 19/27 0.86 Considering cure alone, 5-FU was superior to placebo, to MCSA and the Podophylin considering only treatment failure/ no response, 5-FU was superior to placebo, to MCSA, Podophylin 2% and equal to CO2 Laser and 5FU + INF-2a (low dose) and inferior to 5-FU + INF - 2a ( high dose) and 5FU + Co2 Laser +INF- 2a (high dose). There was no statistical significance between the treatments of 5-FU + INF - 2a (high dose) and 5-FU + Laser of Co2 + INF- 2a (high dose). 5-FU is a good treatment option in view of the costs of INF- 2a and the CO2 Laser. Six trials involving 988 pts (645 women and 343 men) and reporting 8 comparisons were evaluated. Two studies reported withdrawals and dropouts. 5-FU presented better results for cure than placebo or no treatment (relative risk RR 0.39), meta-cresol-sulfonic acid (MCSA) (RR 2.11, 95% ), Podophyllin 2%, 4% or 25% (RR 1.26, 95% CI 0.86 to 1.82). There were no statistical differences for treatment failure for 5-FU Vs CO2 Laser (RR 0.69, 95% CI 0.43 to 1.11) Vs 5-FU + INF-2a (low dose) (RR 1.02, 95% CI 0.87 to 1.119). Worse results were found for 5-FU Vs 5-FU + INF-2a (high dose) (RR 10.78, 95% CI 1.50 to 77.36), and 5-FU + CO2 Laser + INF-2a (high dose) (RR 7.97, 95% CI 2.87 to 22.13). Thank You