Uterine Tubes
advertisement

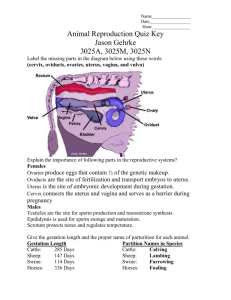
No. 13 1. Female Genital System 2. Perineum Section 2 The Female Genital Organs The female genital organs include the internal genital organs and the external genital organs. The internal genital organs lie in the pelvic cavity, and consist of: ① the gonads (the ovaries): produce the ova and secrete the female hormones. ② the reproductive canals or conveying ducts (uterine tubes, uterus and vagina). ③ the accessory glands: greater vestibular glands (Bartholin’s glands). They are the homologous organs of the bulbourethral glands in the male. The matured follicle ruptures on the surface of the ovary and the ovum is discharged into the peritoneal cavity, then the uterine tube. If the ovum is fertilized in the uterine tube, it is carried to the uterus and develops within the endometrium. The mature fetus passes through the ostium of the uterus, vagina during childbirth. If fertilization does not occur, the ovum begins degeneration after a short time. The female external genital organs is called the female pudendum collectively. Ⅰ. The Internal Genital Organs Ⅰ) The Ovaries They are a pair of oval organs, homologus with the testes in the male. The ovaries are female gonads, producing female reproductive cells— the ova and secrete the female hormones. 1. Location: They are situated one on each side of the uterus close to the lateral wall of the lesser pelvis, in the ovarian fossa, between the upper parts of the internal iliac artery and external iliac artery. 2. External features: Each ovary has: 1) Lateral and medial surfaces: The medial surface is close to the loops of small intestine. 2) Anterior and posterior borders: The posterior border is free, and the anterior border is attached to the posterior surface of the broad ligament by the mesovarium. At the middle part of the anterior border there is the hilum of ovary, through which the blood vessels and nerves pass. 3) Surperior and inferior extremities: The superior extremity, the tubal extremity, connectes with the fimbria of uterine tube. The inferior extremity, the uterine extremity, connects with fundus of uterus. In childhood, the ovaries are small with smooth surfaces. After puberty the ovary becomes progressively scarred, because of the ovulations. After the ages of 40~50, the ovaries become atrophy gradually as the menstruation has ceased. 3. The supporting structures of ovaries The ovaries are maintained in position by a series of ligaments: 1) The suspensory ligament of ovary, or infundibulopelvic ligament, extends from its superior extremity to the pelvic wall, which contains the ovarian vessels, lymphatic vessels, nerves and connective tissues. 2) The proper ligament of ovary passes from the inferior extremity to the fundus of uterus. It is a rounded cord of connective tissue. Ⅱ) The Uterine Tubes They are two tortuous muscular tubes which transmit the ovum. It is 10~14 cm long, 0.5 cm in diameter. 1. Location: They are situated on the upper margins of the broad ligaments of the uterus, and run from each side of the fundus of uterus to the wall of the pelvis. Just before reaching the pelvic wall they turn back upon themselves to open into the peritoneal cavity through the abdominal orifice. Its medial end opens into the superior angle of the cavity of uterus through the uterine orifice. 2. Divisions and their significance: The uterine tube is divided into four parts: the uterine part, the isthmus of uterine tube, the ampulla of uterine tube, the infundibulum of uterine tube, 1) The uterine part (or intramural part) It lies in the wall of the uterus, about 1 cm long. 2) The isthmus of uterine tube It is the medial and narrow portion of the tube, about 2.5 cm long. It is the place where the tubal ligation is performed usually. 3) The ampulla of uterine tube It is the longest and widest part of the tube, between the infundibulum and the isthmus. It forms about 2/3 of the entire length of the tube. It is the side of fertilization. 4) The infundibulum of uterine tube It is a funnel-shaped lateral end of the uterine tube around the ovary superiorly and posteromedially. It is fringed with numerous processes, fimbriae, which spread over most of the medial surface of the ovary. One of them attaching to the superior extremity of the ovary is called the ovarian fimbria. When an ovum is discharged from the ovary, it may be caught by the fimbrae and passes through the abdominal orifice of the tube. Sperm reach the infundibulum within hours after entering the cervix, and fertilization usually occurs in the ampulla. On occasion, a fertilized ovum fails to pass into the uterus and begins to develop in the uterine tube (usually the ampulla), or becomes implanted in the pelvic cavity. Both pelvic and tubular implantations are referred to as ectopic pregnancies. Ⅲ) The Uterus It is a single, hollow organ, with thick muscular wall, in which the fertilized ovum becomes embedded and the developing organism grows until its birth. 1. The features of the uterus In the adults, the uterus is shaped like an inverted pear, and flattened anteroposterioly. In the young nulliparous adult, it measures 7~8 cm long, 4 cm wide at its superior end, and 2~3 cm in thickness. It has the anterior and posterior surfaces, right and left borders. The anterior surface is related to the urinary bladder, and posterior surface to the rectum. (1) Divisions of the uterus The uterus consists of three portions: cervix, body and fundus. ① Fundus The fundus is the superior domeshaped portion above the uterine orifice of the uterine tube. ② Cervix The inferior portion is narrow, and opens into the vagina, called the cervix. The cervix of uterus is 2.5~3.0 cm long. Its inferior 1/3 is surrounded by the superior portion of the vagina, so called the vaginal part. The superior 2/3 is called the supravaginal part. The cavity of cervix is called the cervical canal of uterus. The lower end of the cervical canal has the round opening, called the orifice of uterus which is smooth and round in nullipara, and in the multipara it is a transverse fissure. The anterior border of the orifice of uterus is called the anterior lip and the posterior border the posterior lip, which is longer and higher than the anterior lip. Isthmus: Between the body and the cervix is a constricted region about 1 cm in length, the isthmus. During pregnancy the isthmus enlarges greatly and is taken up by the body, it is therefore often referred to by obstricians as the “lower uterine segment”. The caesarean section is usually performed at here. ③ Body Between the cervix and the fundus is the body. (2) The interior cavity of uterus The interior cavity of the uterus is narrow during nonpregnancy. It is divided into two parts: ① The cavity of uterus It is the superior part, the cavity of uterus, within the body of uterus, is triangular in coronal section with the base upwards. Its upper two angles communicate with the uterine tubes by the uterine orifice of the uterine tube. ② The cervical canal of uterus The inferior part within the cervix is called the cervical canal of uterus, which is spindle-shaped and communicates above, through the internal ostium, with the cavity of the body, and below, through the orifice of uterus, with the vaginal cavity. 2. The location of uterus Normally, the uterus is located entirely in the lesser pelvis between the urinary bladder and the rectum. Its inferior end lies in the vagina. There are uterine tube, ovary and broad ligament on its two sides. The fundus of the uterus is below the level of the pelvic inlet, and the inferior end above the ischial spine. Anteversion and anteflexion: When the bladder is empty the entire uterus is inclined forward upon the bladder, forming an angle (about 90o) between the long axis of the uterus and the vagina, called the anteversion. And also the long axis of the body of the uterus is bent forward on the long axis of the cervix forming an angle of about 170o, which is called the anteflexion. As the bladder fills, the uterus gradually becomes more and more erect. The uterus varies in shape, size, location and structure, depending upon age and other circumstances, such as pregnancy etc. The peritoneum which covers the posterior part of surface of uterus runs down to the posterior part of fornix of vagina, then it reflects onto the rectum, forming the rectouterine pouch. But the peritoneum on the anterior surface of the uterus reflects onto the superior surface of the urinary bladder at the junction of the body and the neck of uterus, forming the vesicouterine pouch. 3. The supports of uterus The normal position of the uterus is maintained by various ligaments and other supports such as the muscles of pelvic floor, neighbouring organs and connective tissue. Damage to these structures may result downward displacement of uterus, called prolapse. (1) The broad ligaments The broad ligaments are composed of two layers of peritoneum, from the lateral margin of the uterus to the lateral wall and floor of the pelvis. The free superior edge of the broad ligament contains the uterine tube. The inferior and lateral margins continue with the peritoneum on the wall of pelvis. In the broad ligament there are the uterine tube, ovary, proper ligament of ovary, round ligament of uterus, blood vessels, lymphatic vessels, nerves and connective tissue. The portions of the broad ligament: The broad ligament is divided into three portions, the mesovarium extending from the anterior border of the ovary to the posterior layer of the broad ligament, the mesosalpinx between the uterine tube and the mesovarium and mesometrium. (2) The round ligaments of uterus The round ligaments of uterus are two bands of fibromuscular tissue between the layers of the broad ligament. Each one attaches to the uterus just below and in front of the uterine orifice of the uterine tube and runs anterolaterally to the lateral wall of the pelvis, then traverses the inguinal canal, ends in the subcutaneous tissue of the greater lip of pudendum. The round ligament tends to hold the uterus in the anteverted position. (3) The cardinal ligaments The cardinal ligaments extend below the base of the broad ligaments between the pelvic wall and the cervix of uterus. These ligaments contain fibrous tissue, smooth muscle, uterine blood vessels, nerves and are the chief ligaments supporting the position of the uterus to prevent from dropping down into the vagina. (4) The uterosacral ligaments The uterosacral ligaments are also called the rectouterine ligaments. They are two folds of peritoneum containing a considerable amount of fibrous tissue and smooth muscular fibers. The ligaments pass backwards from each side of the cervix of uterus, the sides of the rectum, to the front of the second and third sacral vertebrae. The ligaments hold the cervix of uterus in its normal position relative to the sacrum. The uterosacral ligament tends to hold the uterus in the anteflexion position. 4. The structures of uterus The wall of uterus is made up of three coats. 1) The endometrium, the inner coat is mucous membrane, which grows and breaks away during the menstrual cycle. 2) The myometrium, the middle coat is made up of smooth muscle. It is 0.8 cm thick and composed of smooth muscle fibers interspersed with connective tissue and is highly vascular. This coat thickens to 2.5 cm during pregnancy. 3) The outer serous coat is composed of visceral peritoneum. This coat covers most of the uterine surface except for the cervix. Ⅳ) The Vagina It serves as a passage for the menstrual flow and as the female organ of copulation and the lower portion of the “birth canal”. Location: The vagina is situated between the bladder and urethra anteriorly and the rectum and anal canal posteriorly. It consists of three coats: mucous membrane, muscular coat and external coat. It is 8-10 cm long, extending from the cervix of the uterus to the vaginal vestibule. Its upper portion lies above the pelvic floor and the lower portion is narrow and opens to the vaginal vestibule through the vaginal orifice, which is protected in the virgin by a thin mucosal fold called the hymen, which is perforated at its center. Where it passes through the urogenital diaphragm, the urethrovaginal sphincter encircles it. Fornix of vagina: The upper end of vagina surrounds the vaginal portion of the cervix of uterus to form a circular recess, called the fornix of vagina. Its posterior part is higher than the ventral part and two lateral parts. Between the posterior part and the rectouterine pouch, an aspiration or a drainage may be performed through the posterior part. Ⅴ. The Greater Vestibular Glands (Bartholin’s glands) They are about the size of pea and situated one on each side of the vaginal orifice posterior to the bulb of vestibule, deep to the sphincter of vagina. Each gland has a duct which opens between the hymen and the lesser lip of pudendum. They are the homologous organs of the bulbourethral glands in the male. Ⅱ. The External Genital Organs The external genital organs of female are known collectively as the vulva, or female pudendum, which comprises: ①the mons pubis, ②the greater lip of pudendum, ③the lesser lip of pudendum, ④the clitoris, ⑤the vaginal vestibule: It is a cleft between the lesser lips of pudendum, behind the clitoris. It contains the external orifice of urethra anteriorly, 2.5 cm inferoposterior to the clitoris, and the vaginal orifice posteriorly. On the each side of the vaginal orifice there is the orifice of greater vestibular gland. ⑥the hymen. Ⅲ. The Mammae in Female Ⅰ) The Location In the young adult female each mamma forms a round eminence lying within the superficial fascia over the pectoralis major and the deep fascia. It extends from the third to seventh ribs vertically, and from the parasternal line to midaxillary line transversely. Ⅱ) The Features The mammary nipple is on the center of the mamma and commonly lies at the level of the fourth intercostal space. On the wrinkled tip of the nipple there are orifices of 15~20 lactiferous ducts. The base of nipple is encircled by a pigmented area of skin called the areola of breast. On its surface there are many small eminences of areolar glands, which secrete oily secretion to lubricate the nipple. Ⅲ) The Structure The mamma is composed of the mammary gland and adipose tissue mainly. Each mammary gland consists of fifteen to twenty lobes, separated by the adipose tissue, which radiate out from the nipple. Each lobe has an excretory duct, the lactiferous duct, which is enlarged near the nipple called the lactiferous sinus, the end of which is narrowed and opens on the nipple. The incision in the operation on mamma should be made radially to avoid cutting across a number of the lactiferous ducts. Between the skin and the deep fascia, deep to the mammary glands, there are strands of connective tissue called the suspensory ligaments of breast or Cooper’s ligaments, which serve to support the mammary glands. These ligaments may become contracted by fibrosis in cancer of the mamma, thus the overlying skin becomes pitted and retracted. Thereby, it gives an appearance of orange-peel. Section 3 The Perineum The perineum is the diamond-shaped region of the outlet of the pelvis. It includes all the soft tissue between the pubic symphysis and the coccyx. It surrounded anteriorly by the inferior border of the pubic symphysis, laterally by the inferior rami of pubis, rami of ischium, ischial tuberosities, sacrotuberous ligaments, posteriorly by the apex of coccyx. A transverse line drawn between the ischial tuberosities divides the perineum into an anterior urogenital region (urogenital triangle) that contains the external genital organs and the urethra, and a posterior anal region (anal triangle) that contains the anus. In the female, the region between the vagina and anus is known as the obstetrical perineum, and it is often torn during childbirth. Ⅰ. The Anal Region The anus is in the center of this triangle. On each side of the anal canal there is a large space called the ischioanal fossa (ischorectal fossa). Ⅰ) The Sphincter Ani Externus Ⅱ) The Levator Ani Ⅲ) The Coccygeus Ⅳ) The Superior and Inferior Fasciae of Pelvic Diaphragm These fasciae cover the levator ani and coccygeus superiorly and inferiorly. The levator ani and coccygeus together with the superior and inferior fascia of pelvic diaphragm constitute the pelvic diaphragm. There is a hiatus of pelvic diaphragm anterior to the perineal central tendon between the levator ani of each side. In the male the prostate extends into the hiatus and the urethra passes through its center. In the female the urethra and the vagina pass through this hiatus. Inferior to hiatus there is the urogenital diaphragm. Ⅴ) The Ischiorectal Fossa (Ischioanal fossa) It is a space located between the skin of the anal region below, the obturator internus and its fascia, ischial tuberosity laterally, and the levator ani, sphincter ani externus, inferior fascia of pelvic diaphragm medially. It is filled with adipose tissue and contains the vessels and nerves. The internal pudendal artery, vein and the pudendal nerve pass through this fossa along its lateral wall from posterior to anterior to supply the perineum. Ⅱ. The Urogenital Region It is the area between the pubic arches of both sides. Its apex is directed forward and the base is backward. Ⅰ) The Fasciae of Urogenital Diaphragm 1. The superficial fascia Its deep layer is called superficial fascia of perineum (Colles fascia) 2. The inferior fascia of urogenital diaphragm 3. The superior fascia of urogenital diaphragm The three layers form two spaces of fascia the superficial perineal space is between the first and second layers, the deep perineal space is between the second and third layers. Ⅱ) The Muscles of Urogenital Diaphragm 1. The muscles in the superficial perineal space Superficial transverse muscle of perineum, Bulbocavernosus Ischiocavernosus. 2. The muscles in the deep perineal space The deep transverse muscle of perineum and the sphincter of urethra (sphincter of the membranous portion of urethra ) are in the deep perineal space. The sphincter of urethra is also called the external sphincter of urethra in male and the urethrovaginal sphincter in female. The muscles in the deep perineal space, the superior and inferior fasciae of perineum are called the urogenital diaphragm collectively, which is superficial to the pelvic diaphragm and closes the urogenital triangle. 3. The structures in the superficial and deep perineal spaces In the superficial perineal space besides the nerves and blood vessels to supply the perineum, there are the bulb of urethra and the crura of penis in male, the bulb of vestibule, crura of clitoris and greater vestibular glands in female. In the deep perineal space there are the blood vessels and nerves supplying the penis, membranous part of urethra, bulbourethral glands in male and the urethra and vagina in female.