Progesterone for the Prevention of Preterm Birth
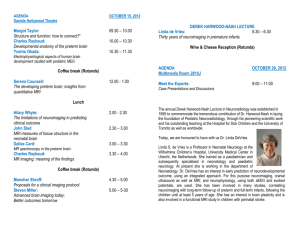
advertisement

Progesterone for the Prevention of Preterm Birth Paul Meis MD Preterm Delivery: Current Status Overview of the problem of preterm birth Strategies to prevent preterm delivery Progesterone for prevention of preterm birth Early trials NICHD MFMU Network trial QuickTime™ and a TIFF (LZW) decompressor are needed to see this picture. Preterm Births in United States QuickTime™ and a TIFF (LZW) decompressor are needed to see this picture. Preterm Births by Race QuickTime™ and a TIFF (LZW) decompressor are needed to see this picture. Very Low Birthweight Births Costs of Prematurity Preterm birth is the major determinant of infant mortality in developed countries Preterm birth is a leading cause of cerebral palsy and developmental delay of surviving children Costs of Prematurity The Institute of Medicine estimates that the total national cost of preterm birth to be $26.2 billion at a minimum. Initial hospital care of infants born at 2527 weeks costs 28 times as much as for those born at term Costs of Prematurity School Performance Age 9-11 Kirkegaard I, Pediatrics 8 7 6 5 33-36 37-38 39-40 4 3 2 1 0 Reading Difficuties Spelling Difficulties Kirkegaard I, Pediatrics 2006;118:1600 “…effective therapeutic interventions to decrease spontaneous preterm delivery have not been discovered.” R.L. Goldenberg 2002 Progesterone Treatment: An Old Idea Revisited A trial of 17 alpha Hydroxyprogesterone Caproate (17P) conducted in the NICHD Maternal Fetal Medicine Units Network. A trial of progesterone suppositories conducted in Brazil. Actions of Progesterone on the Myometrium Decreases conduction of contractions Increases threshold for stimulation Decreases spontaneous activity Decreases number of oxytocin receptors Suppresses the inflammatory cascade Actions of Progesterone on the Myometrium Inhibits T lymphocyte development Promotes expression of prostaglandin EP2 receptor Prevents formation of gap junctions Administration of progesterone antagonists stimulates onset of labor in women at term Early Trials of Progesterone Patients with symptoms of preterm labor in 19561957, University of Copenhagen Double blind study of progesterone (N = 63) vs placebo (N = 63) Daily dose was 200mg x3, 150mg x2, then 100mg per day Results showed no efficacy to prolong pregnancy “Progesterone unable to prevent PTD once clinical symptoms are present” Fuchs F, AJOG 1960 79:172 Early Trials of Progesterone Selected 99 women who were at risk for preterm delivery using a high risk scoring system and randomized them to treatment with 17P or placebo Treated with 250 mg 17P or placebo every three days from 28-32 weeks for a total of 8 doses Delivery at <37 weeks’ in 4% of the 17P group and 18% of the placebo group Papiernik E, 1970 Early Trials of Progesterone 43 patients with previous recurrent miscarriage or preterm birth Treated with 17P or placebo 41% of placebo group delivered <36 weeks of pregnancy All of treated group delivered after 36 weeks Johnson JWC. NEJM 1975;293:675-680 Early Trials of Progesterone 168 pregnant women in the military Treated with 17P or placebo Low birth weight infants: 7.5% in treated subjects 9.0% in placebo subjects Hauth JC. Am J Obstet Gynecol 1983;146:187 Early Trials of Progesterone 77 women with twin pregnancies, randomized to weekly injections of 250 mg 17P or placebo Started after 28 weeks and continued to 37 weeks Delivery at <37 weeks in 31% of the 17P group and 24% of the placebo group This is the only reported trial of 17P in twins Hartikainen A. Obstet Gynecol 1980;56:692 Meta-analysis of progesterone use in pregnancy 15 published trials of various progesterone compounds in women at high risk Pooled analysis of the results of the trials showed no effect on rates of: Miscarriage Stillbirths Preterm births Goldstein P. Brit J Obstet Gynecol 1989;96:265 Meta-analysis of 17P in pregnancy 5 trials which treated high risk women with 17P Pooled analysis of results showed: Reduction in rates of preterm birth. Odds ratio was 0.50, 95% CI: 0.30-0.85 Reduction in rates of low birthweight, Odds ratio was 0.46, 95% CI: 0.27-0.80 Keirse MJNC. Brit J Obstet Gynecol 1990;97:149 “The present study indicates that injections of (17P) may reduce the occurrence of preterm birth in women so treated.” “… further well-controlled research would be necessary before it is recommended for clinical practice.” Keirse MJNC. Brit J Obstet Gynecol 1990;97:149 The existence of the NICHD supported MFMU Network made such a large wellcontrolled trial possible Prevention of Recurrent Preterm Delivery by 17 AlphaHydroxyprogesterone Caproate Meis PJ, Klebanoff M, Thom E, Dombrowski M P, Sibai B, Moawad AH, Spong CY, Hauth JC, Miodovnik M, Varner MW, Leveno KJ, Caritis SN, Iams JD, Wapner RJ, Conway D, O'Sullivan MJ, Carpenter M, Mercer B, Ramin SM, Thorp JM, and Peaceman AM for the NICHD MFMUN NEJM 2003;348:2379-85. Participating Centers of the MFMU Network Wake Forest University University of Tennessee University of AlabamaBirmingham University of Utah Magee-Womens Hospital Thomas Jefferson University University of Miami Columbia University University of North Carolina Case Western Reserve University George Washington University Wayne State University University of Chicago University of Cincinnati University of Texas, Southwestern Ohio State University University of Texas, San Antonio Brown University University of Texas, Houston Northwestern University Choice of Drug Hydroxyprogesterone Caproate, (17P) was chosen because it had been used in previous successful trials 17- Choice of Subjects Women who have had a previous spontaneous preterm birth are at especially high risk for recurrent preterm birth We chose this group of women for eligibility to participate in this trial 17 P and preterm birth inclusion criteria: Documented history of spontaneous preterm birth at 200 to 366 weeks’ gestation in a previous pregnancy Gestational age at entry of 15-203 weeks confirmed by ultrasound Singleton gestation, with no major fetal anomalies Exclusion Criteria Progesterone or heparin treatment during current pregnancy Current or planned cerclage Chronic hypertension Seizure disorder Delivery planned outside the Center Randomization and Follow-up If eligible, women were invited to participate and consented, using a form approved by the Center’s IRB Given a trial injection of the placebo inert oil, and asked to return in 1 week Randomization and Follow-up Second visit (at 160 - 206 weeks) centrally randomized using a 2 to 1 ratio to receive injection of 250 mg 17P or a placebo inert oil Then weekly injections of 17P or placebo until delivery or 37 weeks Power Calculations Primary outcome was delivery <37 weeks’ gestation Estimated rate of recurrent PTB = 37% 2 to 1 allocation of study drug to placebo Sample size = 500 to detect a 33% reduction in the rate of preterm birth Review by Data Monitoring and Safety Committee A scheduled interim analysis was performed after 351 subjects had delivered Analysis showed positive effect for the primary outcome Enrollment of new subjects was halted when 463 subjects randomized Screening and Randomization 2980 women screened 1941 ineligible 576 refused consent or declined after trial injection 310 17-P 1039 eligible 463 randomized 153 placebo Characteristics of Subjects Qualifying delivery Maternal age Married African American Mean BMI Smoking All p > 0.05 17P Placebo 30.5 26.0 51% 59% 26.9 22% 31.3 wks 26.5 yrs 46% 58% 25.9 19% Compliance and Side Effects Compliance with the weekly injections was excellent 91.5% of the women received their injections at the scheduled time Side effects were minor and were similar in the 17P and placebo groups Rates of Births < 37 Weeks 60% 54.9% 50% 36.% 40% 30% 20% 10% 0% p = 0.0001 PLACEBO 17 P Rates of Births < 35 Weeks 35% 30% 30.7% 25% 20.6% 20% 15% 10% 5% 0% P = 0.0165 PLACEBO 17 P Rates of Births < 32 Weeks 25% 20% 19.6% 15% 11.4% 10% 5% 0% p = 0.0180 PLACEBO 17 P Results by Race 70% 60% 50% 40% 58.7% 52.2% 37.6% 35.4% 30% 20% 10% 0% African American p=0.0103 PLACEBO Non African American p=0.0044 17P Rates of Low Birth Weight Birth 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% 41.1% 27.2% 13.9% 8.6% BIRTHS <2500 gm p=0.0029 BIRTHS <1500 gm p=0.0834 PLACEBO 17P Effectiveness of Treatment With 17P 5 to 6 Women with a previous spontaneous preterm birth would need to be treated to prevent one birth <37 weeks 12 Women with a previous spontaneous preterm birth would need to be treated to prevent one birth <32 weeks Rates of Neonatal Death 7% 6% 5.9% 5% 4% 2.6% 3% 2% 1% 0% p = 0.0805 PLACEBO 17P Rates of Neonatal Morbidity 16% 14% 12% 10% PLACEBO 17P 8% 6% 4% 2% 0% RDS BPD ROP IVH* NEC* Percent preterm birth by gestational age of previous preterm delivery 70 60 50 40 Placebo 17P 30 20 10 0 20-27 weeks' 28-33 weeks' 34-37 weeks' Percent preterm birth by number of previous preterm deliveries 80 70 60 50 Placebo 17P 40 30 20 10 0 One More than One Prematurity prevented without evidence of increased infection Chorioamnionitis 1.1 (0.4 – 3.1) Neonatal sepsis 1.1 (0.3 – 3.6) Caveats for 17P cohort versus controls: Fewer PTB in prior pregnancies: 1.4 v 1.6, P=.007 When adjusted for variance: Delivery <37wks RR = 0.7 (0.57, 0.85) More stillbirths: 2.0% v 1.3% P=NS More miscarriages: 1.6% v 0% P=NS Odds ratios for outcomes comparing previous 17P trials with the MFMU results 0.8 0.7 0.6 0.5 Previous 17P Trials MFMU Study 0.4 0.3 0.2 0.1 0 Preterm <2500 gm Perinatal Death Sanchez-Ramos Obstet Gynecol 2005;105:273 Summary of Trial The women in this trial encountered very high rates of preterm delivery The previous preterm delivery was very early, mean = 30-31 weeks’ One third of the women had had more than one previous preterm delivery This rate of preterm birth was similar to other observational studies of high risk women in the MFMU Network Summary of Trial 17P treatment was effective in both African American and Non-African American women 17P treatment was effective in preventing very early as well as later preterm births 17P Treatment of the women resulted in significant reductions in the rates of IVH and NEC for their infants Conclusions from Trial injections of 17- Hydroxyprogesterone Caproate can provide significant and powerful protection against recurrent preterm birth and improve the neonatal outcome for pregnancies at risk Weekly Decision Analysis Model estimated costs of 17P treatment and the costs of preterm birth 17P treatment was cost effective for women with a prior delivery <32 weeks 17P treatment was also cost effective for a history of a prior delivery at 32-37 weeks Odibo AO Obstet Gynecol 2006;108:492 Prophylactic administration of progesterone by vaginal suppository to reduce the incidence of spontaneous preterm birth in women at increased risk: a randomized placebo-controlled trial Da Fonseca EB, Bittar RE, Carvalho MHB, Zugaib M Am J Obstet Gynecol 2003;188:419-24 Trial of progesterone suppositories Tertiary medical center in Brazil 144 women, 70% white Singleton pregnancies with no symptoms of preterm labor Main risk factor was history of a previous preterm delivery (33 weeks both arms) Randomized to daily progesterone (100mg) or placebo suppositories Treated from 24 to 34 weeks’ gestation da Fonseca EB Am J Obstet Gynecol 2003;188:419-424 Results of Trial of Progesterone Suppositories Placebo <37 wks 28.5% Progesterone 13.8% p 0.03 <34 wks 18.6% 2.8% 0.002 No information was given about neonatal outcomes Results were not analyzed by intent to treat da Fonseca EB Am J Obstet Gynecol 2003;188:419-424 Conclusions from Progesterone Suppository Trial The results of this trial show positive results in a population at lower risk for preterm birth than the MFMU Network progesterone study Suggest a possible alternative method of progesterone treatment Progesterone as a Tocolytic 6 trials have been reported Various progesterone compounds used Design of studies varied None of the trials found a significant prolongation of pregnancy with the use of the progesterone treatment Progesterone treatment of women with active uterine contractions should be discouraged outside of research protocols Progesterone Treatment for Prevention of Preterm Birth The results of these trials do not represent the solution to the over-all problem of preterm birth They apply only to women with a previous spontaneous preterm delivery Progesterone Treatment for Prevention of Preterm Birth These results represent a hopeful beginning: the first effective treatments to reduce the risk of preterm delivery in women at risk A major health insurance provider in the U.S. has developed a program of treatment with 17P at a cost of $120 per pregnancy This treatment is cost effective in the prevention of preterm delivery Current Problems with 17P Treatment The drug is currently available in the U.S. only from compounding pharmacies Some insurance plans, including Medicaid do not currently pay for this treatment Gestiva Adeza Biomedical has applied to the FDA to produce 17P for the indication of prevention of preterm delivery FDA approval should improve reimbursement by insurance providers including Medicaid Cost of drug will be higher Further Research Questions Mechanism of action of progesterone treatment Comparative efficacy of different progesterone compounds Effectiveness of progesterone treatment for women in other risk categories Multiple gestation Shortened cervix Continuing Prematurity Prevention Trials in the MFMU Network Trial of 17P vs. placebo in women with multiple gestation Trial of 17P with Omega-3 fatty acid supplement vs. 17P and placebo to prevent recurrent preterm delivery Trial of 17P vs. placebo in primigravid women with a short cervix Some Other Current Trials 17P vs. placebo in twins and triplets (Obstetrix group) Progesterone suppositories vs. placebo suppositories in women with a previous preterm delivery (Columbia Lab sponsored) Reducing Rates of Prematurity Future progress in prevention of preterm delivery is likely to come from primary or secondary prevention strategies Once the parturition process has begun, attempts to prevent preterm birth are not effective