Preterm Labor
advertisement

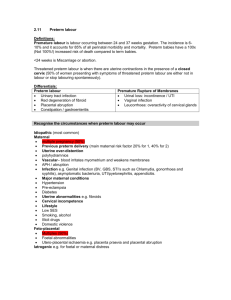
Preterm Labor Williams CH.36 Preterm Birth Death, severe neonatal morbidities Common before 26 weeks Universal before 24 weeks Worse Outcomes Chronic lung disease Grade 3 and 4 intraventricular hemorrhage Periventricular leukomalacia Threshold for neonatal mortality: 1600g Threshold for neonatal morbidity: 1900g Cause of Preterm Birth Medical and obstetrical complications Preeclampsia, fetal distress, IUGR, placenta abruption History of threatened abortion Lifestyle factors Smoking, inadequate weight gain, drug abuse, age, short stature, occupation, poverty Genetic factors Chorioamnionitis Prior Preterm Birth Incompetent Cervix Mean cervical length at 24 weeks: 35 mm Cervical Dilation 2~4 mm during 2nd trimester: predict birth prior to 35 weeks Infections Bacterial vaginosis Tricomonas (low birth weight, preterm birth, perinatal death) Periodontal disease Premature Membrane Rupture PPROM Incidence during 24~34 weeks 1.7 % of pregnancy 20 % of all prenatal deaths 7 % delivery delayed > 48 hours Volume of amniotic fluid after PPROM Better outcome Prognositc importance before 26 weeks PPROM < 23 weeks: lung hypoplasia Antimicrobial therapy Prolong latency period after PPROM If chorioamnionitis is diagnosed Fever Vaginal delivery If PPROM beyond 34 weeks Oxytocin to induction of labor C/S if indicated Preterm Labor Preterm Labor Signs and symptoms Painful or painless uterine contractions Pelvic pressure Menstrual-like cramps Watery vaginal discharge Low back pain Diagnostic critiria Uterine contraction 4 in 20 mins 8 in 60 mins with cervical change Cervical dilatation > 1 cm Cervical effacement > 80% Glucocorticoid Betamethasone 12mg IM stat and 24 hours later Effective: 24 hours after initial dose Effect up to 7 days Adverse effect: Pulmonary edema Infection Difficult glucose control in DM women Bed rest (+) Hydration (-) Antimicrobials (-, if no PPROM) Emergency cerclage (+) Drug to Inhibit Preterm Labor Beta-Adrenergic Agonist Ritodrine Beta-adrenergic receptor desensitization Side effect: Pulmonary edema Hyperglycemia Arrhythmia Magnesium Sulfate Calcium antagonist Cleared almost by renal excretion 4 g loading dose 2 g/hr continuous dose Therapeutic range: Deep tendon reflex disappear 4~7 mEq/L 1 mEq/L = 1.2 mg/dl = 0.5 mmol/L 10 mEq/L Respiratory arrest 12 mEq/L Prostaglandin Inhibitors Indomethacin Total 24 hours dose < 200 mg Side effect: Oligohydramnios (reversible) Calcium Channel Blockers Nifedipine (adalat) Side effect: Hypotension Decrease uteroplacental perfusion Atosiban Nonapeptide oxytocin analogue Competitive antagonist of oxytocininduced contractions Side effect: Nausea, vomiting, headache, dizziness, money loss 18000 NTD/day 感恩