The Heart
advertisement

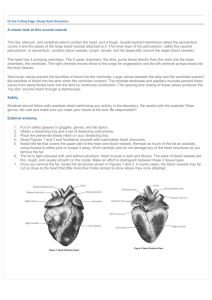
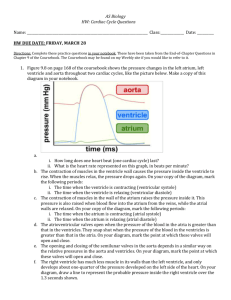
Heart Hold up your clenched fist Your heart is about the size of your fist ◦ Varies by gender, and age of the owner Age changes are due to increases in the size of cells, not number of cells Average mass of a heart 230-350 grams (0.5 – 0.8 pounds) Location and Coverings of the Heart ◦ ◦ ◦ ◦ Heart located between two lungs in thoracic cavity 2/3 of mass is left of body’s midline Apex pointed end formed at tip of left ventricle Base formed by atria, mostly left atrium Major blood vessels enter and exit at the base Pericardium: membrane that surrounds and protects the heart and holds it in place Two parts of pericardium: (1) Fibrous pericardium (2) Serous pericardium Pericarditis build up of pericardial fluid; compresses the heart = cardiac tamponade Heart Wall ◦ Three layers: ◦ EXTERNAL (1) epicardium or visceral layer of serous pericardium Thin, transparent outer layer of the wall Composed of mesothelium and connective tissue MIDDLE (2) myocardium Bulk of heart wall Consists of cardiac muscle Responsible for pumping action of heart Cardiac muscle two separate networks connected by intercalated discs ◦ Atrial ◦ Ventrical Gap junctions in the discs allow action potential conduction from one muscle fiber to the next INTERNAL (3) endocardium Thin layer of squamous epithelium lining inside of myocardium Covers valves of heart and tendons attached to the valves Continuous with epithelial lining of large blood vessels Chambers of the Heart ◦ Four chambers: Two upper are the atria Right atrium Left atrium Two lower are the ventricles Right ventricle Left ventricle Great Vessels of the Heart ◦ Right atrium receives deoxygenated blood through three veins… Superior vena cava Inferior vena cava Coronary sinus ◦ Right ventricle pumps blood into the pulmonary trunk Right pulmonary artery goes to right lung Left pulmonary artery goes to left lung Blood becomes oxygenated 6 3 3 5 5 1 4 4 7 2 8 Valves of the Heart (4) ◦ Prevent blood from flowing backward ◦ Composition: dense connective tissue covered by endothelium ◦ TWO Atrioventricular (AV) valves lie between the atria and ventricles Between the right atrium and right ventricle is the AV called the (1) tricuspid valve, which has the three cusps Chordae tendineae ◦ tendon-like chords that connect the pointed ends of the cusps to cardiac muscle projections on inner surface of the ventricles ◦ prevent the cusps from pushing up into the atria when the ventricles contract ◦ AV between the left atrium and left ventricle is called the (2) bicuspid (mitral) valve It has two cusps ◦ TWO Semilunar valves are located near origin of pulmonary trunk and aorta Prevent blood from flowing back into the heart Pulmonary valve Aortic valve Both consists of three semi-lunar cusps attached to the artery wall Blood Flow Through the Heart ◦ Flow follows pressure high to low Blood Supply of the Heart Natural ‘pacemaker’ of the heart Recordings of the electrical changes that accompany the heartbeat are called electrocardiograms or EKG or ECG Heart Sounds ◦ Come mainly from turbulence created by blood flow when valves close First sound lubb Loud booming sound from AV valves closing after ventricular systole begins Second sound dubb Short, sharp sound from SL valves closing at end of ventricular systole Next a pause…so lubb, dubb, pause, lubb, dubb, pause Cardiac output volume of blood ejected per minute from left ventricle into aorta ◦ Determined by stoke volume (SV) and heart rate (HR) Stroke volume amount of blood ejected by left ventricle during each beat Heart rate number of heart beats per minute Sample calculation of cardiac output: Average resting adult male stroke volume = 70 mL Average heart rate = 75 beats per minute SO…average cardiac output SV X HR 70 mL/beat X 75 beats/min 5250 mL/ min or 5.25 L / min Regulation of Stroke Volume Three factors: ◦ The degree of stretch in the heart before it contracts More stretch means more forceful contraction ◦ The forcefulness of contraction of individual ventricular muscle fibers ◦ The pressure required to eject blood from the ventricle Autonomic Regulation of Heart Rate ◦ Originates in cardiovascular center (CV) in medulla oblongata ◦ Input comes in from a variety of sensory receptors (barorecptors and chemoreceptors) from higher brain centers ◦ Then output is directed through increasing or decreasing frequency of nerve impulses sent to sympathetic and parasympathetic branches Sympathetic neurons reach heart through cardiac accelerator nerves that innervate conduction system, atria, and ventricles releasing norepinephrine to increase heart rate Parasympathetic neurons reach heart through vagus (X) nerves that extend conduction system and atria releasing acetylcholine (ACh) to decrease heart rate Chemical Regulation of Heart Rate ◦ Hormones Epinedrine Norepindrine Increase heart pumping effectiveness by increasing heart rate and contraction force ◦ Ions K+ and Na+ Decrease heart rate and contraction force Ca+ Increase heart rate and contraction force Other Factors in Heart Rate Regulation ◦ ◦ ◦ ◦ Age Gender Physical fitness Body temperature