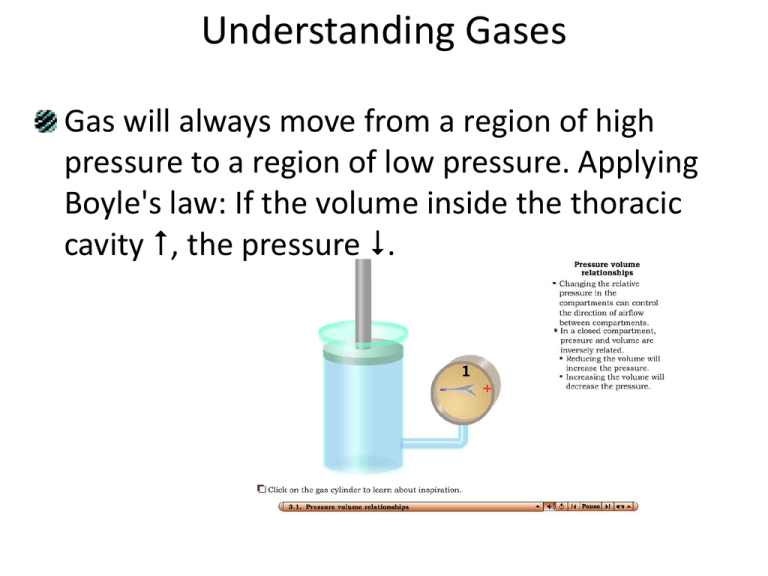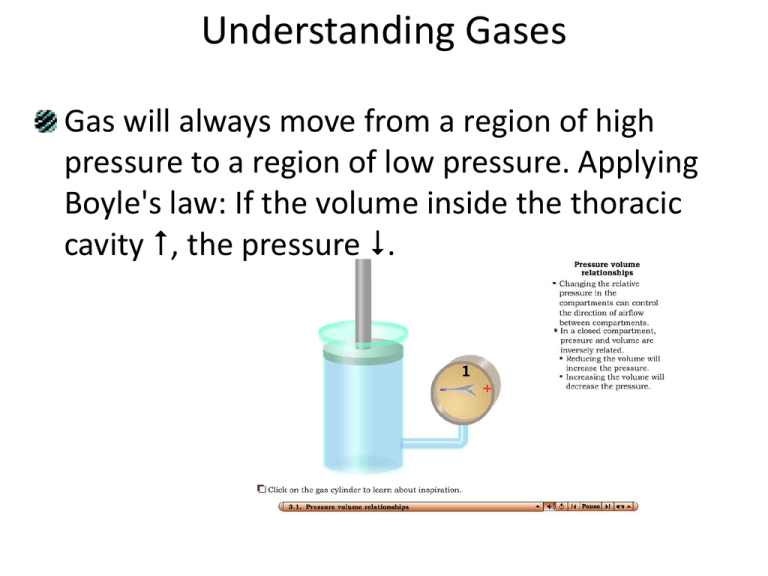
Understanding Gases
Gas will always move from a region of high
pressure to a region of low pressure. Applying
Boyle's law: If the volume inside the thoracic
cavity , the pressure .
Ventilation and Respiration
Pulmonary ventilation is the movement of air
between the atmosphere and the alveoli, and
consists of inhalation and exhalation.
– Ventilation, or
breathing, is made
possible by changes
in the intrathoracic
volume.
Ventilation and Respiration
In contrast to ventilation,
respiration is the exchange of
gases.
– External respiration
(pulmonary)
is gas exchange between the
alveoli and the blood.
– Internal respiration (tissue)
is gas exchange between
the systemic capillaries and
the tissues of the body.
Ventilation and Respiration
External respiration in the lungs is possible
because of the implications of Boyle’s law: The
volume of the thoracic cavity can be increased
or decreased by the action of the diaphragm,
and other muscles of the chest wall.
– By changing the volume of the thoracic cavity (and
the lungs – remember the mechanical coupling of
the chest wall, pleura, and lungs), the pressure in
the lungs will also change.
Ventilation and Respiration
Changes in air pressure result in movement of
the air.
– Contraction of the diaphragm and external
intercostal (rib) muscles increases the size of the
thorax. This decreases the intrapleural pressure so
air can flow in from the atmosphere (inspiration).
– Relaxation of the diaphragm, with/without
contraction of the internal intercostals, decreases
the size of the thorax, increases the air pressure,
and results in exhalation.
Ventilation and Respiration
Certain thoracic
muscles
participate in
inhalation; others
aid exhalation.
– The diaphragm is
the primary
muscle of
respiration – all
the others are
accessory.
Ventilation and Respiration
The recruitment of accessory muscles greatly
depends on whether the respiratory
movements are quiet (normal), or forced
(labored).
Ventilation and Respiration
(Interactions Animation)
In the following animation, the mechanical
coupling mechanism can be understood by
relating the concepts of the gas laws to the
unique anatomical features of the airways,
pleural cavities, and muscles of respiration.
• Pulmonary Ventilation
You must be connected to the internet to run this animation
Airflow and Work of Breathing
Differences in air pressure drive airflow, but 3
other factors also affect the ease with which
we ventilate:
1. The surface tension of alveolar fluid causes the
alveoli to assume the smallest possible diameter
and accounts for 2/3 of lung elastic recoil. Normally
the alveoli would close with each expiration and
make our “Work of Breathing” insupportable.
• Surfactant prevents the complete collapse of alveoli at
exhalation, facilitating reasonable levels of work.
Airflow and Work of Breathing
2. High lung compliance means the lungs and
chest wall expand easily.
– Compliance is decreased by a
broken rib, or by diseases such
as pneumonia or emphysema.
Airflow and Work of Breathing
Measuring Ventilation
Ventilation can be measured using spirometry.
– Tidal Volume (VT) is the volume of air inspired (or
expired) during normal quiet breathing (500 ml).
– Inspiratory Reserve Volume (IRV) is the volume
inspired during a very deep inhalation (3100 ml –
height and gender dependent).
– Expiratory Reserve Volume (ERV) is the volume
expired during a forced exhalation (1200 ml).
Measuring Ventilation
Spirometry continued
– Vital Capacity (VC) is all the air that can be exhaled
after maximum inspiration.
• It is the sum of the inspiratory reserve + tidal volume +
expiratory reserve (4800 ml).
– Residual Volume (RV) is the air still present in the
lungs after a force exhalation (1200 ml).
• The RV is a reserve for mixing of gases but is not
available to move in or out of the lungs.
Measuring Ventilation
Old and new spirometers used to measure ventilation.
Measuring Ventilation
A graph of spirometer volumes and capacities
Measuring Ventilation
Only about 70% of the tidal volume reaches the
respiratory zone – the other 30% remains in the
conducting zone (called the anatomic dead
space).
– If a single VT breath = 500 ml, only 350 ml will
exchange gases at the alveoli.
• In this example, with a respiratory rate of 12, the minute
ventilation = 12 x 500 = 6000 ml.
• The alveolar ventilation (volume of air/min that actually
reaches the alveoli) = 12 x 350 = 4200ml.
Exchange of O2 and CO2
Using the gas laws and understanding the
principals of ventilation and respiration,
we can calculate the
amount of oxygen and
carbon dioxide
exchanged between
the lungs and
the blood.
Exchange of O2 and CO2
• Dalton’s Law states that each gas in a mixture
of gases exerts its own pressure as if no other
gases were present.
– The pressure of a specific gas is the partial pressure
Pp.
– Total pressure is the sum of all the partial
pressures.
– Atmospheric pressure (760 mmHg) = PN2 + PO2 +
PH2O + PCO2 + Pother gases
• Since O2 is 21% of the atmosphere, the PO2 is
760 x 0.21 = 159.6 mmHg.
Exchange of O2 and CO2
Each gas diffuses across a permeable
membrane (like the AC membrane) from the
side where its partial pressure is greater to the
side where its partial pressure is less.
– The greater the difference, the faster the rate of
diffusion.
– Since there is a higher PO2 on the lung side of the
AC membrane, O2 moves from the alveoli into the
blood.
– Since there is a higher PCO2 on the blood side of the
AC membrane, CO2 moves into the lungs.
Exchange of O2 and CO2
PN2
= 0.786
x 760 mmHg
= 597.4 mmHg
PO2
= 0.209
x 760 mmHg
= 158.8 mmHg
PH2O
= 0.004
x 760 mmHg
= 3.0 mmHg
PCO2
= 0.0004
x 760 mmHg
= 0.3 mmHg
Pother gases
= 0.0006
x 760 mmHg
= 0.5 mmHg
Total
= 760.0 mmHg
Partial pressures of gases in inhaled air for sea level
Exchange of O2 and CO2
• Henry’s law states that the quantity of a gas
that will dissolve in a liquid is proportional to
the partial pressures of the gas and its
solubility.
– A higher partial pressure of a
gas (like O2) over a liquid (like
blood) means more of the gas
will stay in solution.
– Because CO2 is 24 times more soluble in blood (and
soda pop!) than in O2, it more readily dissolves.
Exchange of O2 and CO2
Even though the air we breathe is mostly N2,
very little dissolves in blood due to its low
solubility.
– Decompression sickness (“the bends”) is a result of
the comparatively insoluble N2 being forced to
dissolve into the blood and tissues because of the
very high pressures associated with diving.
• By ascending too rapidly, the N2 rushes out of the tissues
and the blood so forcefully as to cause vessels to “pop”
and cells to die.
Transport of O2 and CO2
In the blood, some O2 is dissolved in the plasma
as a gas (about 1.5%, not enough to stay alive –
not by a long shot!). Most O2 (about 98.5%) is
carried attached to Hb.
– Oxygenated Hb is called oxyhemoglobin.
Transport of O2 and CO2
CO2 is transported in the blood in three
different forms:
1. 7% is dissolved in the plasma, as a gas.
2. 70% is converted into carbonic acid through the
action of an enzyme called carbonic anhydrase.
• CO2 + H2O
H2CO3
H+ + HCO3
3. 23% is attached to Hb (but not at the same binding
sites as oxygen).
Transport of O2 and CO2
The O2 transported in the blood (PO2 = 100 mmHg) is
needed in the tissues to continually make ATP (PO2 = 40
mmHg at the capillaries).
CO2 constantly diffuses
from the tissues
(PCO2 = 45 mmHg) to
be transported in
the blood
(PCO2 = 40 mmHg)
Internal Respiration occurs at
systemic capillaries
Transport of O2 and CO2
• The amount of Hb saturated with O2 is called
the SaO2.
– Each Hb molecule can carry 1, 2, 3, or 4 molecules
of O2. Blood leaving the lungs has Hb that is fully
saturated (carrying 4 molecules of
O2 – oxyhemoglobin).
• The SaO2 is close to 95-98% .
– When it returns, it still has 3 of
the 4 O2 binding sites occupied.
• SaO2 = 75%
Transport of O2 and CO2
The relationship between the amount of O2
dissolved in the plasma and the saturation of
Hb is called the oxygen-hemoglobin saturation
curve.
– The higher the PO2
dissolved in the plasma,
the higher the SaO2.
Transport of O2 and CO2
• Measuring SaO2 has
become as
commonplace in clinical
practice as taking a
blood pressure.
– Pulse oximeters which
used to cost $5,000 can
now be purchased at
your local pharmacy.
3660 Group,
Inc/NewsCom
Transport of O2 and CO2
• Although PO2 is the most important
determinant of SaO2, several other factors
influence the affinity with which Hb binds O2 .
– Acidity (pH), PCO2 and blood temperature shift the
entire O2 –Hb saturation
curve either to the left
(higher affinity for O2), or
to the right (lower affinity
for O2).
Transport of O2 and CO2
Transport of O2 and CO2
As blood flows from the lungs toward the
tissues, the increasing acidity (pH decreases)
shifts the O2–Hb saturation curve “to the
right”, enhancing unloading of O2 (which is
just what we want to happen).
– This is called the Bohr effect.
At the lungs, oxygenated blood has a reduced
capacity to carry CO2 ,and it is unloaded as we
exhale (also just what we want to happen).
– This is called the Haldane effect.
Fetal and Maternal Hemoglobin
Fetal hemoglobin (Hb-F) has a higher affinity
for oxygen (it is shifted to the left) than adult
hemoglobin A, so it binds O2 more strongly.
– The fetus is thus able
to attract oxygen
across the placenta
and support life,
without lungs.
Control of Respiration
The medulla rhythmicity area, located in the brainstem,
has centers that control basic respiratory patterns for
both inspiration and expiration.
– The inspiratory center
stimulates the diaphragm
via the phrenic nerve, and
the external intercostal
muscle via intercostal nerves.
• Inspiration normally lasts about 2 sec.
Control of Respiration
Exhalation is mostly a passive process, caused
by the elastic recoil of the lungs. Usually, the
expiratory center is inactive during quiet
breathing (nerve impulses cease for about 3
sec).
– During forced exhalation,
however, impulses from this
center stimulate the internal
intercostal and
abdominal
muscles to contract.
Control of Respiration
Other sites in the pons help the medullary centers
manage the transition between inhalation and
exhalation.
– The pneumotaxic center limits inspiration to prevent
hyperexpansion.
– The apneustic
center coordinates
the transition between
inhalation and exhalation.
Control of Respiration
Other brain areas also play a role in respiration:
– Our cortex has voluntary control of breathing.
– Stretch receptors sensing over-inflation arrests
breathing temporarily (Herring Breuer reflex).
– Emotions (limbic system) affect respiration.
– The hypothalamus, sensing a fever, increases
breathing, as does moderate pain (severe pain causes
apnea.)
Control of Respiration
(Interactions Animation)
• Regulation of Ventilation
You must be connected to the internet to run this animation
Response to Pollutants
Initial Response
– Mucous layer thickens.
– Goblet cells over-secrete
mucous.
– Basal cells proliferate.
Normal columnar epithelium in
the respiratory tract
Advanced Response to Irritation
– Mucous layer and goblet cells disappear.
– Basal cells become malignant & invade deeper tissue.
Diseases and Disorders
Asthma is a disease of hyper-reactive airways
(the major abnormality is constriction of
smooth muscle in the bronchioles, and
inflammation.) It presents as attacks of
wheezing, coughing, and excess mucus
production.
– It typically occurs in response to allergens; less
often to emotion.
– Bronchodilators and antiinflammatory corticosteroids
are mainstays of treatment.
Pulse Picture Library/CMP mages /Phototake
Diseases and Disorders
Chronic bronchitis and emphysema are caused
by chronic irritation and inflammation leading
to lung destruction. Patients may cough up
green-yellow sputum due to
infection and increased mucous
secretion (productive cough).
–They are almost exclusively
diseases of cigarette smoking.
Diseases and Disorders
Pneumonia is an acute infection of the lowest
parts of the respiratory tract.
– The small bronchioles and alveoli become filled
with an inflammatory fluid exudate.
• It is typically caused by infectious agents such as
bacteria, viruses, or fungi.
Diseases and Disorders
Normal Lungs
Patient
Du Cane Medical Imaging, Ltd./Photo Researchers, Inc
Pneumonia
End of Chapter 23
Copyright 2012 John Wiley & Sons, Inc. All rights reserved.
Reproduction or translation of this work beyond that permitted
in section 117 of the 1976 United States Copyright Act without
express permission of the copyright owner is unlawful. Request
for further information should be addressed to the Permission
Department, John Wiley & Sons, Inc. The purchaser may make
back-up copies for his/her own use only and not for distribution
or resale. The Publisher assumes no responsibility for errors,
omissions, or damages caused by the use of these programs or
from the use of the information herein.