Chapter 23.

Chapter 22.
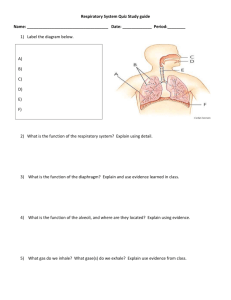
Respiratory System
Overview
• Respiratory anatomy
• Respiration
• Respiratory musculature
• Ventilation, lung volumes and capacities
• Gas exchange and transport
– O
2
– CO
2
• Respiratory centers
• Chemoreceptor reflexes
• Respiratory Diseases
Oxygen
• Is obtained from the air by diffusion across delicate exchange surfaces of lungs
• Is carried to cells by the cardiovascular system which also returns carbon dioxide to the lungs
Functions of the
Respiratory System
• Supplies body with oxygen and get rid of carbon dioxide
• Provides extensive gas exchange surface area between air and circulating blood
• Moves air to and from exchange surfaces of lungs
• Protects respiratory surfaces from outside environment
• Produces sounds
• Participates in olfactory sense
Components of the
Respiratory
System
Figure 23–1
Organization of the
Respiratory System
• Upper respiratory system
– Nose, nasal cavity, sinuses, and pharynx
• Lower respiratory system
– Larynx, trachea, bronchi and lungs
The Respiratory Tract
• Conducting zone :
– from nasal cavity to terminal bronchioles
– conduits for air to reach the sites of gas exchange
• Respiratory zone :
– the respiratory bronchioles, alveolar ducts , and alveoli
– sites of gas exchange
The Respiratory Epithelium
Figure 23–2
Respiratory Epithelia
• Changes along respiratory tract
• Nose, nasal cavity, nasopharynx = pseudostratified ciliated columnar epithelium
• Oropharynx, laryngopharynx = stratified squamous epitheium
• Trachea, bronchi = pseudostratified ciliated columnar epithelium
• Terminal bronchioles = cuboidal epithelium
• Respiratory bronchioles, alveoli = simple squamous epithelium
• Think about why each part has the lining that it does
– For example, in alveoli
• walls must be very thin (< 1 µ m)
• surface area must be very great (about 35 times the surface area of the body)
– In lower pharynx
• walls must be tough because food abrades them
The Respiratory Mucosa
• Consists of:
– epithelial layer
– areolar layer
• Lines conducting portion of respiratory system
• Lamina propria
– Areolar tissue in the upper respiratory system, trachea, and bronchi (conducting zone)
– Contains mucous glands that secrete onto epithelial surface
– In the conducting portion of lower respiratory system, contains smooth muscle cells that encircle lumen of bronchioles
Respiratory Defense System
• Series of filtration mechanisms removes particles and pathogens
• Hairs in the nasal cavity
• Goblet cells and mucus glands : produce mucus that bathes exposed surfaces
• Cilia : sweep debris trapped in mucus toward the pharynx ( mucus escalator )
• Filtration in nasal cavity removes large particles
• Alveolar macrophages engulf small particles that reach lungs
Upper Respiratory Tract
Figure 23–3
Upper Respiratory Tract
• Nose :
– Air enters through nostrils or external nares into nasal vestibule
– Nasal hairs in vestibule are the first particle filtration system
• Nasal Cavity :
– Nasal septum divides nasal cavity into left and right
– Mucous secretions from paranasal sinus and tears clean and moisten the nasal cavity
– Meatuses Constricted passageways in between conchae that produce air turbulence:
• Warm (how?) and humidify incoming air (bypassed by mouth breathing)
• trap particles
• Air flow: from external nares to vestibule to internal nares through meatuses , then to nasopharynx
The Pharynx
• A chamber shared by digestive and respiratory systems that extends from internal nares to the dual entrances to the larynx and esophagus at the C6 vertebrae
• Nasopharynx
– Superior portion of the pharynx (above the soft palate) contains pharyngeal tonsils; epithelium?
• Oropharynx
– Middle portion of the pharynx, from soft palate to epiglottis; contains palatine and lingual tonsils; communicates with oral cavity; epithelium?
• Laryngopharynx
– Inferior portion of the pharynx, extends from hyoid bone to entrance to larynx and esophagus
Lower Respiratory Tract
• Air flow from the pharynx enters the larynx , continues into trachea , bronchial tree , bronchioles , and alveoli
Anatomy of the Larynx
Figure 23–4
Cartilages of the Larynx
• 3 large, unpaired cartilages form the body of the larynx (voice box)
– thyroid cartilage (Adam’s apple)
• hyaline cartilage
• Forms anterior and lateral walls of larynx
• Ligaments attach to hyoid bone, epiglottis, and other laryngeal cartilages
– cricoid cartilage
• hyaline cartilage
• Form posterior portion of larynx
• Ligaments attach to first tracheal cartilage
– the epiglottis
• elastic cartilage
• Covers glottis during swallowing
• Ligaments attach to thyroid cartilage and hyoid bone
Small Cartilages of the Larynx
• 3 pairs of small hyaline cartilages:
– arytenoid cartilages
– corniculate cartilages
– cuneiform cartilages
• Corniculate and arytenoid cartilages function in opening and closing the glottis and the production of sound
Larynx Functions
• To provide a patent airway
• To function in voice production
• To act as a switching mechanism to route air and food into the proper channels
– Thyroid and cricoid cartilages support and protect the glottis and the entrance to trachea
– During swallowing the larynx is elevated and the epiglottis folds back over glottis prevents entry of food and liquids into respiratory tract
Sphincter Functions of Larynx
• The larynx is closed during coughing, sneezing, and Valsalva’s maneuver
• Valsalva’s maneuver
– Air is temporarily held in the lower respiratory tract by closing the glottis
– Causes intra-abdominal pressure to rise when abdominal muscles contract
– Helps to empty the rectum
– Acts as a splint to stabilize the trunk when lifting heavy loads
• Glottis also “closed” (covered) by epiglottis during swallowing
The Glottis
Figure 23–5
Sound Production
• Air passing through glottis:
– vibrates vocal folds and produces sound waves
• Sound is varied by:
– tension on vocal folds
– voluntary muscles position cartilages
Anatomy of the Trachea
Figure 23–6
The Trachea
• Extends from the cricoid cartilage into mediastinum where it branches into right and left bronchi
• Has mucosa, submucosa which contains mucous glands, and adventitia
• Adventita made up of 15–20 C-shaped tracheal cartilages (hyaline) strengthen and protect airway
– Ends of each tracheal cartilage are connected by an elastic ligament and trachealis muscle where trachea contacts esophagus. Why?
The Primary Bronchi
• Right and left primary bronchi are separated by an internal ridge (the carina )
• Right primary bronchus
– larger in diameter than the left
– descends at a steeper angle
The Bronchial Tree
• Formed by the primary bronchi and their branches
• Each primary bronchus (R and L) branches into secondary bronchi, each supplying one lobe of the lungs (5 total)
• Secondary Bronchi Branch to form tertiary bronchi
• Each tertiary bronchus branches into multiple bronchioles
• Bronchioles branch into terminal bronchioles:
• 1 tertiary bronchus forms about 6500 terminal bronchioles
Bronchial
Tree
Figure 23–9
Bronchial Structure
• The walls of primary, secondary, and tertiary bronchi:
– contain progressively less cartilage and more smooth muscle, increasing muscular effects on airway constriction and resistance
• Bronchioles:
– Consist of cuboidal epithelium
– Lack cartilage support and mucus-producing cells and are dominated by a complete layer of circular smooth muscle
Autonomic Control
• Regulates smooth muscle:
– controls diameter of bronchioles
– controls airflow and resistance in lungs
• Bronchodilation of bronchial airways
– Caused by sympathetic ANS activation
– Reduces resistance
• Bronchoconstriction
– Caused by parasympathetic ANS activation or
– histamine release (allergic reactions)
The Bronchioles
Figure 23–10
Conducting Zones
Figure 22.7
Lungs
Figure 23–7
The Lungs
• Left and right lungs: in left and right pleural cavities
• The base :
– inferior portion of each lung rests on superior surface of diaphragm
• Hilus
– Where pulmonary nerves, blood vessels, and lymphatics enter lung
– Anchored in meshwork of connective tissue
Lung Anatomy
• Lungs have lobes separated by deep fissures
• Right lung is wider and is displaced upward by liver. Has 3 lobes:
– superior, middle, and inferior
– separated by horizontal and oblique fissures
• Left lung is longer is displaced leftward by the heart forming the cardiac notch. Has 2 lobes:
– superior and inferior
– separated by an oblique fissure
Relationship between
Lungs and Heart
Figure 23–8
Respiratory Zone
• Each terminal bronchiole branches to form several respiratory bronchioles , where gas exchange takes place ( Exchange Surfaces )
• Respiratory bronchioles lead to alveolar ducts , then to terminal clusters of alveolar sacs composed of alveoli
• Approximately 300 million alveoli:
– Account for most of the lungs’ volume
– Provide tremendous surface area for gas exchange
Respiratory Zone
Alveoli
• Alveoli Are air-filled pockets within the lungs where all gas exchange takes place
• Alveolar epithelium is a very delicate, simple squamous epithelium
• Contains scattered and specialized cells
• Lines exchange surfaces of alveoli
Alveolar
Organization
Figure 23–11
Alveolar Organization
• Respiratory bronchioles are connected to alveoli along alveolar ducts
• Alveolar ducts end at alveolar sacs: common chambers connected to many individual alveoli
• Each individual alveolus has an extensive network of capillaries and is surrounded by elastic fibers
Alveolar Epithelium
• Consists of simple squamous epithelium (Type I cells)
• Patrolled by alveolar macrophages , also called dust cells
• Contains septal cells (Type II cells) that produce surfactant:
– oily secretion containing phospholipids and proteins
– coats alveolar surfaces and reduces surface tension
Alevolar problems
• Respiratory Distress : difficult respiration
– Can occur when septal cells do not produce enough surfactant
– leads to alveolar collapse
• Pneumonia : inflammation of the lung tissue
– causes fluid to leak into alveoli
– compromises function of respiratory membrane
Respiratory Membrane
• The thin membrane of alveoli where gas exchange takes place. Consists of:
– Squamous epithelial lining of alveolus
– Endothelial cells lining an adjacent capillary
– Fused basal laminae between alveolar and endothelial cells
• Diffusion across respiratory membrane is very rapid because distance is small and gases (O
2 and CO
2
) are lipid soluble
Blood Supply to
Respiratory Surfaces
• Pulmonary arteries branch into arterioles supplying alveoli with deox. blood
• a capillary network surrounds each alveolus as part of the respiratory membrane
• blood from alveolar capillaries passes through pulmonary venules and veins, then returns to left atrium with ox. blood
Blood Supply to the Lungs Proper
• Bronchial arteries provide systemic circulation bringing oxygen and nutrients to tissues of conducting passageways of lung
– Arise from aorta and enter the lungs at the hilus
– Supply all lung tissue except the alveoli
• Venous blood bypasses the systemic circuit and just flows into pulmonary veins
• Blood Pressure in the pulmonary circuit is low
(30 mm Hg)
• Pulmonary vessels are easily blocked by blood clots, fat, or air bubbles, causing pulmonary embolism
Pleural Cavities and
Membranes
• 2 pleural cavities are separated by the mediastinum
• Each pleural cavity holds a lung and is lined with a serous membrane = the pleura :
– Consists of 2 layers:
• parietal pleura
• visceral pleura
– Pleural fluid: a serous transudate that lubricates space between 2 layers
Respiration
• Refers to 4 integrated processes:
– Pulmonary ventilation – moving air into and out of the lungs (provides alveolar ventilation)
– External respiration – gas exchange between the lungs and the blood
– Transport – transport of oxygen and carbon dioxide between the lungs and tissues
– Internal respiration – gas exchange between systemic blood vessels and tissues
Gas Pressure and Volume
Figure 23–13
Boyle’s Law
• Defines the relationship between gas pressure and volume:
P 1/V
Or
P
1
V
1
• In a contained gas:
= P
2
V
2
– external pressure forces molecules closer together
– movement of gas molecules exerts pressure on container
Pulmonary
Ventilation
Respiration:
Pressure Gradients
Figure 23–14
Respiration
• Air flows from area of higher pressure to area of lower pressure (it’s the pressure difference, or gradient, that matters)
• Volume of thoracic cavity changes
(expansion or contraction of diaphragm or rib cage) creates changes in pressure
• A Respiratory Cycle Consists of:
– an inspiration (inhalation)
– an expiration (exhalation)
Lung Compliance
• An indicator of expandability
• Low compliance requires greater force to expand
• High compliance requires less force
• Kind of like capacitance
• Affected by:
– Connective-tissue structure of the lungs
– Level of surfactant production
– Mobility of the thoracic cage
Pressure Relationships
Figure 22.12
Gas Pressure
• Normal atmospheric pressure (P atm
) = 1 atm (or 760 mm Hg) at sea level
• Intrapulmonary Pressure (intra-alveolar pressure) is measured relative to P atm
• In relaxed breathing, the difference between P atm and intrapulmonary pressure is small: only -1 mm Hg on inhalation or +1 mm Hg on expiration
• Max range: from -30 mm Hg to +100 mm
Hg)
Intrapleural Pressure
• Pressure in space between parietal and visceral pleura
• Actually a “potential space” because serous fluid welds the two layers together (like a wet glass on a coaster)
• Remains below P atm throughout respiratory cycle due to:
– Elasticity of lungs causes them to assume smallest possible size
– Surface tension of alveolar fluid draws alveoli to their smallest possible size
• These forces are resisted by the bond between the layers of pleura so there is always a negative pressure trying to pull the lungs into a smaller voluume
• If lungs were allowed to collapse completely, based on their elastic content they would only be about 5% of their normal resting volume
P and V Changes with
Inhalation and Exhalation
Figure 23–15
The Respiratory Pump
• Cyclical changes in intrapleural pressure operate the respiratory pump which aids in venous return to heart
Lung Collapse
• Injury to the chest wall can cause pneumothorax : when air is allowed to enter the pleural space.
• Caused by equalization of the intrapleural pressure with the intrapulmonary pressure
(the bond between lung and pleura breaks)
• Causes atelectasis (a collapsed lung)
The Respiratory Muscles
Figure 23–16a, b
Respiratory Muscles
• Inhalation: always active
– Diaphragm : contraction flattens it, expanding the thorax and drawing air into lungs, accounts for 75% of normal air movement
– External intercostal muscles: assist inhalation by elevating ribs, accounts for 25% of normal air movement
• Exhalation: normally passive
– Relaxation of diaphragm decreases thoracic volume
– Gravity causes rib cage to descend
– Elastic fibers in lungs and muscles cause elastic rebound
– All serve to raise intrapulmonary pressure to +1atm
Muscles of Active Exhalation
• Internal intercostals actively depress the ribs
• Abdominal muscles compress the abdomen, forcing diaphragm upward
Both serve to greatly decrease the thoracic volume, thus increasing the pressure more air leaves (and does so faster)
Resistance in Respiratory Passageways
• As airway resistance rises, breathing movements become more strenuous
• Severely constricted or obstructed bronchioles:
– Can prevent lifesustaining ventilation
– Can occur during acute asthma attacks which stops ventilation
• Epinephrine release via the sympathetic nervous system dilates bronchioles and reduces air resistance
Figure 22.15
Modes of Breathing
• Quiet Breathing (Eupnea) involves active inhalation and passive exhalation
– Diaphragmatic breathing or deep breathing :
• is dominated by diaphragm
– Costal breathing or shallow breathing :
• is dominated by ribcage movements
• usually occurs due to conscious effort or abdominal/thoracic obstructions (e.g. pregnancy)
• Forced Breathing (hyperpnea) involves active inhalation and exhalation
• Both assisted by accessory muscles
Respiratory Rates and Volumes
• Respiratory system adapts to changing oxygen demands by varying:
– the number of breaths per minute ( respiratory rate )
– the volume of air moved per breath ( tidal volume )
Both can be modulated
• Minute Volume (measures pulmonary ventilation) = respiratory rate
tidal volume
– kind of like CO = HR x SV)
• Both RR and TV can be modulated
Dead Space
• Only a part of respiratory minute volume reaches alveolar exchange surfaces
• Volume of air remaining in conducting passages is anatomic dead space
Alveolar Ventilation
• Alveolar ventilation is the amount of air reaching alveoli each minute = respiratory rate
(Tidal
Volume - anatomic dead space)
– for a given respiratory rate:
• increasing tidal volume increases alveolar ventilation rate
– for a given tidal volume:
• increasing respiratory rate increases alveolar ventilation
• Alveoli contain less O
2
, more CO
2 than atmospheric air because inhaled air mixes with exhaled air
Mammalian Respiratory System – poor design?
• Inhaled air mixes with exhaled air
• Lots of dead space in the system
• These are the results of a bi-directional, blind ended ventilation system – what if water entered and left your sink through the same spout?
• Birds, fish have unidirectional circuits so fresh and stale air never mix
Respiratory Volumes and Capacities
Figure 23–17
Lung Volumes
• Resting tidal volume
• Expiratory reserve volume (ERV)
• Residual volume
– minimal volume (in a collapsed lung)
• Inspiratory reserve volume (IRV)
Calculated
Respiratory Capacities
• Inspiratory capacity
– tidal volume + IRV
• Functional residual capacity (FRC):
– ERV + residual volume
• Vital capacity :
– ERV + tidal volume + IRV
• Total lung capacity :
– vital capacity + residual volume
Gas Exchange
• Occurs between blood and alveolar air across the respiratory membrane
• Depends on:
– partial pressures of the gases
– diffusion of molecules between gas and liquid in response to concentration or pressure gradients
The Gas Laws
• Rate of diffusion depends on physical principles, or gas laws
– Boyle’s law : P 1/V
– Dalton’s law : each gas contributes to the total pressure in proportion to its number of molecules
– Henry’s Law : at a given temperature, the amount of a gas in solution is proportional to partial pressure of that gas
Composition of Air
• Nitrogen (N
2
) = 78.6%
• Oxygen (O
2
) = 20.9%
• Water vapor (H
2
O) = 0.5%
• Carbon dioxide (CO
2
) = 0.04%
• Atmospheric pressure produced by air molecules bumping into each other = 760 mmHg
• Partial Pressure = the pressure contributed by each gas in the atmosphere
• Dalton’s Law says P
O2
= .209 x 760 = 160mmHg
Normal Partial Pressures
• In pulmonary vein plasma (after visiting lungs):
– P
– P
CO
2
= 40 mm Hg
= 100 mm Hg
– P
O
2
N
2
= 573 mm Hg
Mixing in Pulmonary Veins
• Oxygenated blood mixes with deoxygenated blood from conducting passageways that bypasses systemic circuit
• Remember the bronchial arteries? There are no bronchial veins – these venules join the pulmonary veins that otherwise have oxygenated blood.
• Lowers the PO
2 of blood entering systemic circuit (about 95 mm Hg)
Henry’s
Law
Figure 23–18
Henry’s Law
• When gas under pressure comes in contact with liquid, gas dissolves in liquid until equilibrium is reached
• At a given temperature, the amount of a gas in solution is proportional to partial pressure of that gas
• The amount of a gas that dissolves in solution
(at given partial pressure and temperature) also depends on the solubility of that gas in that particular liquid : CO
2 soluble, N
2 is very soluble, O has very low solubility
2 is less
Overview of Pressures in the Body
P
P
O
2
(atmosphere) = 160 mm Hg
(lungs) = 100 mm Hg [104]
P
O
2
(left atrium) = 95 mm Hg
P
O
2
(resting tissue) = 40 mm Hg
P
O
2
O
2
(active tissue) = 15 mm Hg
P
P
CO
2
CO
2
(lungs) = 40 mm Hg
(tissue) = 45 mm Hg
Diffusion and the
Respiratory Membrane
• Direction and rate of diffusion of gases across the respiratory membrane are determined by:
– partial pressures and solubilities
– matching of alveolar ventilation and pulmonary blood perfusion (gotta have enough busses)
Efficiency of Gas
Exchange
• Due to:
– substantial differences in partial pressure across the respiratory membrane
– distances involved in gas exchange are small
– O
2 and CO soluble
2 are lipid
– total surface area is large
– blood flow and air flow are coordinated
Respiratory
Processes and Partial
Pressure
Figure 23–19
O
2
and CO
2
• Blood arriving in pulmonary arteries has low P high P
CO
• The concentration gradient causes: O and CO
2 to leave blood
2
O
2 and to enter blood
• Blood leaving heart has high P
• Interstitial Fluid has low P
45 = mm Hg
O
2
O
2 and lowP
CO
2
= 40 mm Hg and high P
CO
2
• Concentration gradient in peripheral capillaries is opposite of lungs so CO
2 diffuses into blood and O
2 enter tissue to
• Although carbon dioxide has a lower partial pressure gradient (only 5mmHg)
– It is 20 times more soluble in plasma than oxygen
– It diffuses in equal amounts with oxygen
Gas Pickup and Delivery
• Red Blood Cells (RBCs): transport O
2 and CO
2 from, peripheral tissues
• Remove O
2 and CO
2 from plasma, allowing gases to diffuse into blood to,
• Hb carries almost all O
2
, while only a little
CO
2 is carried by Hb
Oxygen Transport
• O
2 binds to iron ions in hemoglobin (Hb) molecules in a reversible reaction
• Each RBC can bind a billion molecules of
O
2
• Hemoglobin Saturation : the percentage of heme units in a hemoglobin molecule that contain bound oxygen
Respiration: Oxygen and Carbon Dioxide
Transport
Environmental Factors
Affecting Hemoglobin
• P
O
2 of blood
• Blood pH
• Temperature
• Metabolic activity within RBCs
Respiration: Hemoglobin
Respiration: Percent O
2
Hemoglobin
Saturation of
Hemoglobin Saturation Curve
Figure 23–20 (Navigator)
Oxyhemoglobin Saturation
Curve
• Graph relates the saturation of hemoglobin to partial pressure of oxygen
• Higher P
O
2 results in greater Hb saturation
• Is a curve rather than a straight line because Hb changes shape each time a molecule of O
2 makes next O
2
( cooperativity ) is bound. Each O
2 binding easier bound
Oxygen Reserves
• Notice that even at P
O
2
= 40 mm Hg,
Oxygen saturation is at 75%. Thus, each
Hb molecule still has 3 oxygens bound to it. This reserve is needed when tissue becomes active and P
O
2 drops to 15 mm
Hg
Carbon Monoxide Poisoning
• CO from burning fuels:
– Binds irreversibly to hemoglobin and takes the place of O
2
pH, Temperature, and
Hemoglobin Saturation
Figure 23–21
Hemoglobin
Saturation Curve
• When pH drops or temperature rises:
– more oxygen is released
– curve shift to right
• When pH rises or temperature drops:
– less oxygen is released
– curve shifts to left
The Bohr Effect
• The effect of decreased pH on hemoglobin saturation curve
• Caused by CO
2
– CO
2
: diffuses into RBC
– an enzyme, called carbonic anhydrase , catalyzes reaction with H
2
O
– produces carbonic acid (H
2
CO
3
)
• Carbonic acid (H ion (HCO
3
—
)
2
CO
3
):
– dissociates into hydrogen ion (H +
) and bicarbonate
• Hydrogen ions diffuse out of RBC, lowering pH
Hemoglobin and pH
2,3-biphosphoglycerate (BPG)
• RBCs generate ATP by glycolysis, forming lactic acid and BPG
• BPG directly affects O
2 binding and release: more BPG, more oxygen released
• There is always some BPG around to lower the affinity of Hb for O
2 not release oxygen)
(without it, hemoglobin will
• BPG levels rise:
– when pH increases
– when stimulated by certain hormones
Fetal and Adult Hemoglobin
Figure 23–22
Fetal and Adult Hemoglobin
• At the same P
O
2
:
– fetal Hb binds more O
2 allows fetus to take O
2 than adult Hb, which from maternal blood
KEY CONCEPTS
• Hemoglobin in RBCs:
– carries most blood oxygen
– releases it in response to low O pressure in surrounding plasma
2 partial
• If P
O increases, hemoglobin binds oxygen
• If P
O decreases, hemoglobin releases oxygen
• At a given P
O hemoglobin will release additional oxygen if pH decreases or temperature increases
Carbon
Dioxide
Transport
Figure 23–23 (Navigator)
CO
2
Transport
• CO
2 is generated as a byproduct of aerobic metabolism (cellular respiration)
• Takes three routes in blood:
– converted to carbonic acid
– bound to protein portion of hemoglobin
– dissolved in plasma
CO
2
in the Blood Stream
• 70% is transported as carbonic acid (H
2
CO which dissociates into H + and bicarbonate
(HCO
3
-
)
• Bicarbonate ions move into plasma by a
3
) countertransport exchange mechanism that takes in Cl
ions without using ATP (the chloride shift )
• At the lungs, these processes are reversed
– Bicarbonate ions move into the RBCs and bind with hydrogen ions to form carbonic acid
– Carbonic acid is then split by carbonic anhydrase to release carbon dioxide and water
– Carbon dioxide then diffuses from the blood into the alveoli, then is breathed out
CO
2
inside RBCs
CO
2
+ H
2
O H
2
CO
3
(Enzyme = carbonic anhydrase )
H
2
CO
3
H
+
+ HCO
3
-
CO
2
Carbon dioxide
+ H
2
O
Water
H
2
CO
3
Carbonic acid
H +
Hydrogen ion
+ HCO
3
–
Bicarbonat e ion
CO
2
in the Blood Stream
• 20 - 23% is bound to amino groups of globular proteins in Hb molecule forming carbaminohemoglobin
• 7 - 10% is transported as CO
2 plasma dissolved in
KEY CONCEPT
• CO
2 travels in the bloodstream primarily as bicarbonate ions, which form through dissociation of carbonic acid produced by carbonic anhydrase in RBCs
• Lesser amounts of CO
2 are bound to Hb and even fewer molecules are dissolved in plasma
Summary: Gas Transport
Figure 23–24
Influence of Carbon Dioxide on
Blood pH
• The carbonic acid–bicarbonate buffer system resists blood pH changes
• If hydrogen ion concentrations in blood begin to rise, excess H + is removed by combining with
HCO
3
–
• If hydrogen ion concentrations begin to drop, carbonic acid dissociates, releasing H +
• Changes in respiratory rate can also:
– Alter blood pH
– Provide a fast-acting system to adjust pH when it is disturbed by metabolic factors
Control of Respiration
• Ventilation – the amount of gas reaching the alveoli
• Perfusion – the blood flow reaching the alveoli
• Ventilation and perfusion must be tightly regulated for efficient gas exchange
• Gas diffusion at both peripheral and alveolar capillaries maintain balance by:
– changes in blood flow and oxygen delivery
– changes in depth and rate of respiration
Regulation of O
2
Transport
• Rising P
CO
2 levels in tissues relaxes smooth muscle in arterioles and capillaries, increasing blood flow there ( autoregulation )
• Coordination of lung perfusion (blood) and alveolar ventilation (air):
– blood flow is shifted to the capillaries serving alveoli with high P
– P
CO
2
O
2 and low P
CO
2 levels control bronchoconstriction and bronchodilation: high P
CO
2
(opposite of tissue) causes bronchodilation
(just like with blood in the tissues)
Ventilation-Perfusion Coupling
• In tissue high CO
2 causes vasodilation, in lungs, high CO
2 causes vasoconstiction
(Why?)
• In lungs high CO
2 causes bronchodilation
(Why?) while low CO
2 causes constriction
Blood goes to alveoli with low CO
2 goes to alveoli with high CO
2
, air
Ventilation-Perfusion Coupling
Reduced alveolar ventilation; excessive perfusion
P
O2
P
CO2 in alveoli
Pulmonary arterioles serving these alveoli constrict
Reduced alveolar ventilation; reduced perfusion
Enhanced alveolar ventilation; inadequate perfusion
P
O2
P
CO2 in alveoli
Pulmonary arterioles serving these alveoli dilate
Enhanced alveolar ventilation; enhanced perfusion
Figure 22.19
The Respiratory Rhythmicity
Centers
• Respiratory rhythmicity centers in medulla set the pace of respiration
• Can be divided into 2 groups:
– dorsal respiratory group (DRG)
• Inspiratory center
• Functions in quiet breathing (sets the pace) and forced breathing
• Dormant during expiration
– ventral respiratory group (VRG)
• Inspiratory and expiratory center
• Functions only in forced breathing
Quiet Breathing
• Brief activity in the DRG stimulates inspiratory muscles
• After ~2 seconds, DRG neurons become inactive, allowing passive exhalation
• Note that VRG is not involved
Forced Breathing
• Increased activity in DRG:
– stimulates VRG to become active
– which activates accessory inspiratory muscles
• After inhalation:
– expiratory center neurons stimulate active exhalation
Quiet Breathing
Forced
Breathing
Figure 23–25b
Centers of the Pons
• Paired nuclei that adjust output of respiratory rhythmicity centers:
– regulating respiratory rate and depth of respiration
• Pons centers:
– Influence and modify activity of the medullary centers
– Smooth out inspiration and expiration transitions and vice versa
• The pontine respiratory group (PRG) – continuously inhibits the inspiration center
Respiratory
Centers and Reflex
Controls
Figure 23–26
Sensory Modifiers of
Respiratory Center Activities
• Chemoreceptors are sensitive to:
– P
CO
2
, P
O
2
, or pH of blood or cerebrospinal fluid
• Baroreceptors in aortic or carotid sinuses:
– sensitive to changes in blood pressure
• Stretch receptors respond to changes in lung volume
• Irritating physical or chemical stimuli in nasal cavity, larynx, or bronchial tree promote airway constriction
Chemoreceptor Reflexes
• Respiratory centers are strongly influenced by chemoreceptor input from:
– carotid bodies (cranial nerve IX)
– aortic bodies (cranial nerve X)
– receptors in medulla that monitor cerebrospinal fluid
• All react more strongly to changes in pH and
P
CO
2
, to a lesser extent to changes in P
• So in general, CO
2
O
2 levels, rather than O
2 levels, are primary drivers of respiratory activity
• At rest, it is the H+ ion concentration in brain
CSF (which is a proxy measure of CO
2 levels)
Chemoreceptors and oxygen
• Arterial oxygen levels are monitored by the aortic and carotid bodies
• Substantial drops in arterial P
O2
(to 60 mm Hg) are needed before oxygen levels become a major stimulus for increased ventilation
• If carbon dioxide is not removed (e.g., as in emphysema and chronic bronchitis), chemoreceptors become unresponsive to P
CO2 chemical stimuli
• In such cases, P
O2 levels become the principal respiratory stimulus (hypoxic drive)
Chemoreceptor
Responses to PCO
2
Figure 23–27
Effect of Breathing on Ventilation
• Breathing faster and deeper gets rid of more CO
2
, takes in more O
2
• Breathing more slowly and shallowly allows CO
2 to build up, less O
2 comes in
Chemoreceptor Stimulation
• Leads to increased depth and rate of respiration
• Is subject to adaptation: decreased sensitivity due to chronic stimulation
Changes in Arterial P
CO
2
• Hypercapnia : an increase in arterial P
CO
2
– Stimulates chemoreceptors in the medulla oblongata to restore homeostasis by increasing breathing rate
• Hypocapnia : a decrease in arterial P
CO
– Inhibits chemoreceptors, breathing rate
2 decreases
Ventilation Issues
• Hypoventilation
– A common cause of hypercapnia
– Abnormally low respiration rate allows CO
2 blood, should result in increased RR build-up in
• Hyperventilation
– Excessive ventilation
– Results in abnormally low P
CO
2
( hypocapnia )
– Stimulates chemoreceptors to decrease respiratory rate
– Treatment? Why?
Baroreceptor Reflexes
• Carotid and aortic baroreceptor stimulation: affects both blood pressure and respiratory centers
• When blood pressure falls:
– respiration increases
• When blood pressure increases:
– respiration decreases
Breathing and Heart Rate
• Your ventilation and perfusion must be coordinated, otherwise the circulatory and respiratory systems not efficient.
• Examples:
– Increase HR but not RR – no more O
2 coming in than before so blood can’t deliver it to tissues
– Increase RR but not HR – O
2 is coming in more quickly but it can’t get to the tissues
• Also, if BP falls, RR and HR rise and vice versa
The Hering –Breuer Reflexes
• 2 baroreceptor reflexes involved in forced breathing:
– inflation reflex :
• Caused by stretch receptor in lungs
• prevents lung overexpansion
– deflation reflex :
• inhibits expiratory centers and stimulates inspiratory centers during lung deflation so inspiration can start again
Changes in Respiratory
System at Birth
1. Before birth: pulmonary vessels are collapsed and lungs contain no air
2. During delivery blood P
O
2 falls, P
CO
2 rises
3. At birth newborn overcomes force of surface tension to inflate bronchial tree and alveoli and take first breath
4. Large drop in pressure at first breath pulls blood into pulmonary circulation, closing foramen ovale and ductus arteriosus redirecting fetal blood circulation patterns
5. Subsequent breaths fully inflate alveoli
Respiratory Disorders
• Restrictive disorders : lung cancer, fibrosis, pleurisy
– Fibrosis: decreases compliance
– harder to inhale
• Obstructive disorders : emphysema, asthma, bronchitis (COPD)
– Loss of elasticity: increases compliance
– Harder to exhale (FRC increased)
COPD – Chronic Obstructive
Pulmonary Disease
• Includes: emphysema , chronic bronchitis , asthma. Often, both emphysema and bronchitis are present but in differing proportions
• Symptoms
– difficult to exhale
– May have barrel chests due to trapped air in lungs
– dyspnea (shortness of breath) accompanied by wheezing, and a persistent cough with sputum
COPD - Emphysema
• Loss of elastic tissue in the lung alveoli lead to their enlargement and degeneration of the respiratory membrane leaving large holes behind
• Suffers are called “ pink puffers ” because they are thin, usually maintain good oxygen saturation, and breathe through pursed lips
(Why?)
• Caused by smoking or (rarely) by alpha1 antitrypsin deficiency – this is a congenital lack of the gene for alpha1 antitrypsin which normally protects alveoli from enzyme neutrophil elastase; without it, elastase eats away the elastic fibers
COPD Chronic Bronchitis
• Inflammation of airways causes narrowing of bronchioles and a buildup of mucus, both of which restrict air flow
• During exhalation, airways collapse (why not during inhalation?)
• These patients are often called “ blue bloaters ” because they have low oxygen saturation (cyanosis), and often have systemic edema secondary to vasoconstriction and right-sided heart failure
• Adaptation of the chemoreceptors occurs especially in the ones sensitive to CO
2
• Thus, their only drive to breathe is provided by low O
2 levels! This is why they are always blue. DO NOT GIVE
THESE PATIENTS O
2
! They will stop breathing totally.
Altitude
• Altitude sickness: low pressure leads to hypoxia, can cause cerebral and pulmonary edema
• Normal response to acute high altitude exposure include:
– Increased ventilation – 2-3 L/min higher than at sea level due to
Increased RR and tidal volume
– Increased HR
– Substantial decline in P
O2 stimulates peripheral chemoreceptors:
– Chemoreceptors become more responsive to P
CO2
• Over time
– Increased hematocrit
– Increased BPG causes a right shift in Hb making it easier to offload oxygen at the tissues
Lung fluid
• Pleural effusion – fluid buildup in pleural cavity/space (kind of like pericarditis)
• Pulmonary edema – fills exchange surfaces
Cystic Fibrosis
• Recessive genetic disease caused by simple mutation in both copies of the gene for a chloride transporter.
• Without it, Cl- cannot be pumped onto the lung surface, Na+ doesn’t follow and neither does water.
• Sticky mucus builds up inside lungs and infections are common. Often fatal before age 30
Others
• Decompression sickness –the bends, nitrogen bubbles exit the blood, enter the tissues: painful and dangerous
• Shallow water blackout: hyperventilation leads to artificially reduced CO2, allows you to hold your breath to the point of passing out
Pneumothorax
• Hole in pleural membrane causes lung collapse
(atelectasis)
• Non-tension pneumothorax – a hole through both lung and pleural membrane breaks tension between the pleura, lung elasticity causes it to pull away from the chest wall
• Tension pneumothorax – a hole in the lung allows air to escape into the pleural space with each breath, further raising in the intrapleural pressure and collapsing the lung
SIDS
• Sudden infant death syndrome
• Disrupts normal respiratory reflex pattern
• May result from connection problems between pacemaker complex and respiratory centers
• See extra credit options
Lung cancer
• 50% die within one year of diagnosis
• Only 20% or so survive 5 years
• Around 90% of cases are due exclusively to smoking