Female Reproductive Disorders
advertisement

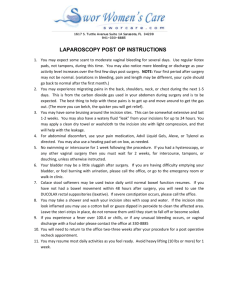
Female Reproductive Disorders Megan McClintock, MS, RN Fall 2011 Infertility Can’t conceive after 1 year of regular, unprotected intercourse Risk factors Tobacco/illicit drug use Abnormal BMI (obesity or too thin) Age > 35 (in women) Infertility Diagnostic Studies Detailed history and general physical exam Basal body temperature record (upon awakening, before any activity, decreased temp prior to ovulation, rise in temp with ovulation) Ovulation prediction kits (measure LH in urine, ovulation occurs 28-36 hrs after the first rise of LH) Hysterosalpingogram to look at tubal factors Postcoital cervical mucus exam Infertility Treatment Depends on the cause Ovarian problems – supplemental hormone therapy Cervicitis – antibiotics Inadequate estrogen stimulation - Estrogen Intrauterine insemination Assisted reproductive technologies (ART) Nursing care Education Emotional support Encourage participation in support groups Abortion Spontaneous (occurring naturally) Natural loss of pregnancy before 20 weeks s/s – uterine cramping with vaginal bleeding Tx – bed rest, no vaginal intercourse, D&C may be needed, emotional/grief support Induced (occurring due to mechanical or medical intervention) Intentional or elective termination of a pregnancy Technique depends on gestational age, women’s condition Care – give support/acceptance, prepare the pt, no intercourse or vaginal insertions for 2 weeks, can start contraception immediately Cx – abnormal vaginal bleeding, severe abdominal cramping, fever, foul drainage Menstrual Problems PMS Dysmenorrhea (pain) Abnormal bleeding Oligomenorrhea (long intervals between menses) Amenorrhea (no menstruation) Metrorraghia (spotting, breakthrough bleeding) Menorrhagia (excessive bleeding) Ectopic pregnancy Perimenopause Postmenopause Premenstrual Syndrome (PMS) PMS Always occurs cyclically before the onset of menstruation, not present at other times of the month s/s – extremely variable even from one cycle to another, breast tenderness, edema, bloating, binge eating, headache, dizziness, mood swings Dx – must rule out other possible causes, no definitive test, need to do a symptom diary for 2-3 months PMS Treatment No single treatment Drugs (diuretics, prostaglandin inhibitors, SSRIs, combination BCPs) Diet changes (no caffeine, reduce refined carbs, increase complex carbs with high fiber, vit B6, dairy, poultry, limit salt intake) Reassure that symptoms are real Stress management Exercise Adequate rest Dysmenorrhea Primary – no pathology, begins within first few years of menses s/s – starts 12-24 hrs before menses, rarely lasts more than 2 days, lower abd pain radiating to lower back/upper thighs, nausea, diarrhea, fatigue, headache Tx – heat, exercise, NSAIDs, BCPs Secondary – usu. caused by pelvic disease, begins age 30-40 after previous pain-free menses s/s – unilateral, constant pain that lasts longer than 2 days, can have painful intercourse, painful defecation, or irregular bleeding Tx – depends on the cause Abnormal Bleeding Age of the woman helps determine the cause Young – spontaneous abortion, ectopic pregnancy, clotting disorders 30s/40s – leiomyomas (fibroids), endometrial polyps Old – endometrial cancer Amenorrhea Primary – no menses by age 16 Secondary – had periods but they stopped Need to shed the endometrial lining 4-6 times/year Bleeding Treatment Depends on the cause, degree of threat to pt’s health, desire for children in the future Health history and physical exam first Combined oral contraceptives, fertility drugs, or progesterone Balloon thermotherapy Endometrial ablation Hysterectomy or myomectomy if due to uterine fibroids D&C is rarely done Nursing Care with Abnormal Bleeding Bathing and hair washing are safe Can swim, exercise, have intercourse Need to change tampons or pads frequently Be aware of TSS (s/s – high fever, vomiting, diarrhea,, weakness, myalgia, sunburn-like rash) With excessive bleeding, record the number and size of pads/tampons used and degree of saturation Check fatigue level, BP, and pulse Ectopic Pregnancy Life-threatening emergency! Implantation of a fertilized ovum anywhere outside the uterus Risk factors – PID, prior ectopic, progestin-releasing IUD, progestin-only birth control pills, prior pelvic or tubal surgery, infertility treatments s/s – abd/pelvic pain, missed period, irregular vaginal bleeding (spotting), if ruptured - pain will be severe and may be referred to the shoulder Ectopic Pregnanct Dx – difficult b/c it’s similar to other disorders, but has to be considered first! Serum pregnancy test Then serial beta-hCG levels Vaginal ultrasound CBC Tx – immediate surgery, may need blood transfusion Menopause Perimenopause – begins with first changes in menses and ends after cessation of menses Menopause – cessation of menses associated with declining ovary function, complete after 1 year of no periods Usu. occurs around age 51, naturally affected only by genetic factors, autoimmune conditions, cigarette smoking, racial/ethnic factors Increase in FSH, decrease in estrogen Remember culture Remember vaginal bleeding after menopause is a sign of possible endometrial cancer Perimenopause s/s – *irregular vaginal bleeding, *vasomotor instability (hot flashes), redistribution of fat, gain weight more easily, muscle/joint pain, loss of skin elasticity, change in hair amount/distribution, atrophy of external genitalia/breast tissue, dysparenunia, bladder changes Critical changes – increased risk for CAD and osteoporosis, higher risk for HIV transmission if exposed Perimenopause Diagnosis should only be made after ruling out other things Tx – hormone replacement therapy (HRT) Must weigh the risks and benefits Use lowest effective dose Estrogen side effects – nausea, fluid retention, headache, breast swelling Progesterone side effects – increased hunger, weight gain, irritability, depression, spotting, breast tenderness Depoprovera can cause sudden loss of vision, chest pain, calf pain Vaginal creams helpful with urogenital symptoms Transdermal estrogen bypasses the liver but causes skin irritation HRT Take only for short-term (4-5 years) relief of severe symptoms Estrogen alone can cause stroke, blood clots, breast changes but protects against osteoporosis, colorectal cancer, heart disease Estrogen & progesterone together can cause heart disease, breast cancer, stroke, blood clots, breast changes Do not take if you have a history of breast cancer, heart disease, or blood clots Non Hormonal Treatments Cool environment Vitamin E Limit caffeine and alcohol Adequate exercise and sleep Relaxation techniques Adequate calcium and vitamin D Increase air circulation Avoid bedding that traps heat Diet high in complex carbs and B6, soy, tofu, sunflower seeds Loose fitting clothes Black cohosh Kegel exercises Moisturizing soaps, lotion Vaginal lubrication Vulvar, Vaginal, Cervical Conditions Typically infection and inflammation related to sexual intercourse Risks – contaminated hands, clothing, douche equipment, intercourse, surgery, childbirth; BCPs, antibiotics, corticosteroids s/s – abnormal vaginal discharge, red lesions; yeast – thick, white, curd-like discharge, itching, dysuria; bacterial vaginosis – fishy odor; cervicitis – spotting after intercourse; lichen sclerosis – white lesions with “tissue paper” appearance Treatment Sexual history is important Microscopy and cultures Antibiotics and/or antifungals (must take full course) Abstain from intercourse for at least 1 week Douching should be avoided May need to treat sexual partners Vaginal creams should be inserted before going to bed Clean carefully after urination and bowel movements Use a non-judgmental attitude Pelvic Inflammatory Disease (PID) Infection of pelvic cavity (fallopian tubes, ovaries, pelvic peritoneum), often the result of untreated cervicitis Chlamydia and gonorrhea are most common organisms, but is not always from STDs Can cause infertility and chronic pelvic pain s/s – lower abdominal pain that starts gradually and becomes constant, movement increases the pain, spotting after intercourse, may have fever, chills Will have adnexal tenderness and positive cervical motion tenderness with bimanual pelvic exam (diagnostic), can also do a vaginal ultrasound PID Complications Septic shock Fitz-Hugh-Curtis syndrome (perihepatitis) Peritonitis Thrombophlebitis of the pelvic veins Adhesions of the fallopian tubes Ectopic pregnancy PID Treatment Antibiotics No intercourse for 3 weeks Sexual partner(s) must be treated Physical rest Lots of oral fluids Must be reevaluated in 48-72 hours to ensure they are improving If hospitalized: Corticosteroids Heat to abdomen or sitz baths Semi-Fowler’s position to promote drainage by gravity Analgesics, IV fluids May require surgery Endometriosis Normal endometrial tissue located in sites outside of the endometrial cavity Not life-threatening, but causes lots of pain Increases the risk of ovarian cancer Typical pt – late 20s or early 30s, white, never had a full-term pregnancy s/s – dysmenorrhea after year of painfree periods, infertility, pelvic pain, pain with intercourse, irregular bleeding, backache Cx – bowel obstruction, painful urination Endometriosis Treatment Definitive diagnosis – laparoscopy Tx determined by age, desire for pregnancy, symptom severity, extent/location of disease Drugs – NSAIDs, Depo-Provera or Lupron to imitate a state of pregnancy or menopause (is only controlled, not cured by this), lots of side effects, will take for 9 months to shrink the endometrial tissue Surgery – only cure Leiomyomas Uterine fibroids, benign smooth-muscle tumors Seem to depend on ovarian hormones b/c they grown slowly during reproductive years and atrophy after menopause s/s – generally none, but may have abnormal uterine bleeding, pain, pelvic pressure Tx – depends on symptoms, age of pt, desire to bear children, location/size of tumors; lots of bleeding or large tumors mean surgery (hysterectomy, myomectomy, uterine artery embolization, or cryosurgery) Cervical Polyps Benign lesion on a stalk, seen through the cervical os during a speculum exam (bright cherry-red, soft, fragile, small (< 3 cm)) s/s – none usually, might have spotting, bleeding after BM straining, bleeding after sex, infection Tx – outpatient excision or polypectomy (send for biopsy to ensure no malignancy) Polycystic Ovary Syndrome (PCOS) Many benign cysts on both ovaries, usu. occurs in women < age 30, causes infertility s/s –irregular menses, infertility, hirsutism, obesity, acne, can even develop CV disease and type 2 diabetes Tx – BCPs, aldactone (for hirsutism), Lupron, Metform, may use fertility drugs (Clomid) to cause ovulation, may ultimately need hysterectomy with salpingectomy and oopherectomy Needs weight management and exercise Cervical Cancer Risk factors – low socioeconomic status, early sexual activity (< age 17), multiple sexual partners, HPV infection, immunosuppression, smoking Higher incidence in white women, but higher mortality in African American women (avg age-50) Best tx is prevention with regular Pap screens Cause – repeated injuries to the cervix s/s – early cancer is asymptomatic, thin/watery vaginal discharge becoming dark and foul-smelling, spotting that becomes heavier and more frequent, pain is a late symptom as is weight loss, anemia, muscle wasting Cervical Cancer Diagnostic studies *Pap testing – begin 3 years after first intercourse but no later than age 21 Not 100% accurate so very impt to follow up after abnormal Pap tests Minor changes in Pap – repeat Pap in 4-6 months for 2 years Prominent changes in Pap – colposcopy and biopsy, may have punch biopsy or conization (outpatient procedures with mild analgesics or sedation) Cervical Cancer Treatment Prevention with Gardasil vaccine for females age 9-26 Guided by tumor stage, pt’s age, general state of health (see pg 1364, Table 54-11) Can sometimes preserve fertility Invasive cancer is treated with surgery, radiation (4-6 weeks external, 1-2 internal implants), and chemo Endometrial Cancer Most common gynecologic cancer, grows slowly, metastasizes late, curable if diagnosed early Risk factors – estrogen, increasing age, no pregnancy, late menopause, obesity, smoking, diabetes, history of colorectal cancer s/s – *first sign is abnormal uterine bleeding in postmenopausal women, pain occurs late Tx - *endometrial biopsy, total hysterectomy/bilateral salpingo-oophorectomy with lymph node biopsy, may need radiation; may also need progesterone hormonal therapy (Megace) or Tamoxifen and chemo Ovarian Cancer Most have advanced disease at time of diagnosis Risk factors – family history of ovarian cancer, breast cancer, colon cancer, no pregnancies, increasing age, highfat diet, early menses or late menopause, HRT, use of infertility drugs Reduced risk – use of BCPs, breastfeeding, multiple pregnancies, early age at first pregnancy s/s – vague in early stages, abdominal enlargement, daily symptoms for at least 3 weeks (pelvic/abdominal pain, bloating, urinary urgency/frequency, difficulty eating or feeling full quickly), pain is a late symptom, vaginal bleeding is not a usual symptom Ovarian Cancer Diagnostics No screening tests other than a yearly bimanual pelvic exam (if postmenopausal should not have palpable ovaries) OVAI – can help detect whether a pelvic mass is benign or malignant If at high risk, can test for CA-125 (tumor marker) and use ultrasound with the yearly pelvic exam Ovarian Cancer Treatment If at high risk, prophylactic oophorectomy, BCPs Staging guides treatment decision Stage I – total abdominal hysterectomy/bilateral salpingo- oophorectomy and chemo Stage II – external irradiation and/or chemo Stage III – chemo and surgical debulking Metastasis often causes pleural effusion and shortness of breath Vaginal and Vulvar Cancer Both are relatively rare Treatment may be with surgery and radiation Vulvar surgery has a high risk of morbidity due to scarring and wound breakdown Surgeries Hysterectomy – removal of the uterus, may (total) or may not (subtotal) remove the cervix, removal of fallopian tubes (salpingectomy), removal of ovaries (oophorectomy); if all TAH-BSO Can be done vaginally or abdominally In both, the ligaments that support the uterus are attached to the vaginal cuff to maintain the normal depth of the vagina Care after Hysterectomy Abdominal dressing or sterile perineal pad (vaginal approach) Observe closely for bleeding for first 8 hours Watch for urinary retention (may have catheter for 1-2 days ) Report backache or decreased urine output to surgeon Watch for paralytic ileus Prevent DVTs – turn, no high-Fowler’s, no pressure under the knee Assist with grief over loss of fertility May need HRTs Discharge – no intercourse for 4-6 weeks, may be temporary loss of vaginal sensation, no heavy lifting for 2 months, avoid pelvic congestion for several months (ie. Dancing, walking swiftly), wear a girdle Vulvectomy, Vaginectomy Vulvectomy – removal of vulva and wide margin of skin, Vaginectomy – removal of vagina Post-op care Perineal wound extending to the groin that may be covered or left exposed, usu. has a drain Meticulous wound care – clean with NS twice daily Use heat lamp or hair dryer to dry the area Prevent stool straining Be very careful not to dislodge urinary catheter Lots of discomfort due to heavy, taut sutures Ambulation on 2nd post op day Easy to get discouraged due to mutilation of perineum and slow healing Pelvic Exenteration Radical hysterectomy, total vaginectomy, removal of bladder with urinary diversion, resection of bowel with colostomy (anterior – no bowel resection, posterior – no bladder removal Post-op care - similar to care after radical hysterectomy, abd perineal resection and ileostomy and/or colostomy; lots of physical, emotional, and social adjustments Radiation Therapy (Brachytherapy) In the OR, places radiation near or into the tumor causing less damage to surrounding normal tissue, delivered using wires, capsules, needles, tubes, seeds; left in for 24-72 hrs Preparation – cleansing enema to prevent stool straining, indwelling catheter to prevent distended bladder Care – lead-lined private room, absolute bed rest (can be turned from side to side), analgesics for uterine contractions, deodorizer, cluster care, nurses can spend no more than 30 minutes/day in room, stay at foot of bed or entrance to room, visitors must stay 6 feet from bed and stay less than 3 hours/day, discharge to home after radioactive material and catheter are removed Common to have foul-smelling vaginal discharge from destruction of cells, may also have n/v, diarrhea, malaise Cx – fistulas, cystitis, phlebitis, hemorrhage, fibrosis Problems with Pelvic Support Uterine Prolapse Displacement of uterus into the vaginal canal First degree – cervix in lower part of vagina Second degree – cervix at vaginal opening Third degree – uterus protrudes through vaginal opening s/s – feeling of “something coming down”, pain with sex, backache, stress incontinence Tx – Kegel exercises, pessary, vaginal hysterectomy Cystocele and Rectocele Cystocele – weakening between vagina and bladder Rectocele – weakening between vagina and rectum Common and asymptomatic Tx – Kegel exercises, pessary, surgery to tighten the vaginal wall, colporrhaphy (post-op care includes catheter to prevent suture strain) Fistula Abnormal opening between internal organs or between an organ and the exterior of the body Causes – gyneocologic procedures, injury during childbirth, cancer s/s – excoriation, irritation, severe infections, wetness, odors Tx – if small may heal on own, can’t do surgery until inflammation and edema is resolved Care – perineal hygiene every 4 hours, warm sitz baths 3 times/day, good fluid intake, post-op – catheter for 7-10 days, delay the first post-op stool to prevent wound contamination Sexual Assault Forcible perpetration of a sexual act on a person without their consent s/s – may have no signs of physical trauma, may have bruising and/or lacerations, STDs, pregnancy; may have a range of psychologic symptoms; may have post-traumatic stress disorder weeks to months to years after assault (rapetrauma syndrome) Tx - *highest priority is ensuring emotional and physical safety, SANE RN provides care while ensuring evidence is safeguarded (obtain consent, collect and label data, have as few people handle the data as possible, gynecologic/sexual history, account of the assault, lab tests looking for sperm and pregnancy), need follow-up physical and psychological care (return weekly for the first month) Sexual Assault Nursing care Encourage all women to learn self-defense Quiet, private area for exam Never leave the patient alone Maintain a non-judgmental attitude Let the patient talk, listen carefully Be supportive during the pelvic exam Provide a change of clothing Offer the “morning after pill” Explain about application for financial compensation Never send them home alone Let them know about the crisis center