Case Studies
advertisement

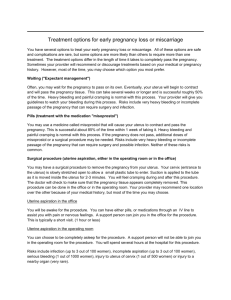
Early Pregnancy Loss Definition • Nonviable intrauterine pregnancy charactized by empty gestational sac or embryo/fetus <13 weeks with no fetal heart activity • 10% of all pregnancies • 50% are generally chromosomal abnormalities Signs and Symptoms • First trimester cramping/bleeding • DDx: early pregnancy loss, viable intrauterine pregnancy, ectopic pregnancy • A pelvic exam is important before testing Testing • Ultrasound is the prefered method to determine viabilty • HCG levels are important in interpreting ultrasound findings and for serial follow up Beta HCG • Discriminatory zone 1500-2000 mIU/ml is associated with a gestational sac in singleton pregnancies • A rise of < 50% in 48 hours is associate with an abnormal pregnancy with a sensitivity of 99% Treatment Options • Expectant • Medical treatment • Surgical treatment Expectant • May take up to 8 weeks • 80% success • What is success – HCG < 5 mIU/ml – Endometrial stripe of < 3 cm – Return of normal menstrual function • Patient needs to be prepared for moderate to heavy bleeding with cramps and may need a suction currettage Medical Treatment • Goal is to shorten the time to complete explusion as compared to expectant • 85% success with complete expulsion with in 3 days for 70% of patients • Patient should expect moderate to heavy bleeding and cramping issues as well as possible suction currettage Surgical • Suction curettage has replaced sharp curetting • It is immediate and 99% successful • Clinically important intrauterine adhesions are a rare complication Complications of all treatments • Incomplete requiring curettage • Infection 2% • Transfusion 1% Rh Negative Mother • Give 50-300 micrograms rhogam within 72 hrs of diagnosis of early pregnancy loss Subsequent Pregnancy • No evidenced based data on when it is safe to get pregnant again • BCP or IUD can be started as soon as you are sure the process is complete • Consider workup for recurrent EPL after the 2nd consecutive EPL • No proven treatment for threatened abortion • Progesterone in first trimester after at least 3 EPL may be beneficial Case Studies Am I ready to do office gyn? Sally is a 23 y/o GoPo complaining of irregular bleeding Gyn Hx: sexually active uses condoms most times PE: 105 lb Abdomen soft nontender Pelvic exam: no vaginal bleeding, Cervix is closed nontender, uterus normal, adenexa neg Test Results • Quantative Beta HCG < 1 • Ultrasound normal uterus, endometrium, and ovaries What if Ultrasound Shows • uterus 11x9x8 cm with multiple leiomyoma about 2-3 cm in diameter, endometrial thickness 6 mm, normal ovaries Sally returns after 3 months on her new birth control pill still having breakthrough bleeding Pelvic exam is normal Test: STD negative pregnancy test negative Judy is a 30 y/o G2P2 for annual exam on Ortho Tricyclen Lo Social hx: married, monogamous She is complaining that she had regular periods for a while but now having breakthrough bleeding for 6 months Exam: Normal Differential diagnosis? Mary is a 45 y/o G3P3 status post tubal ligation Menstral formula: 2 weeks/3 days heavy on day 1 PMH: negative Pelvic exam: Cervix normal, pap done Uterus 6 weeks size, irregular, firm, nontender Ovaries not enlarged, nontender Guidelines for Endometrial Biopsy • All women with history of AUB of 2-3 yrs duration • All women > 45 yrs old with AUB • All women who do not respond to treatment Endometrial Biopsy Results • Complex hyperplasia with atypia • Complex hyperplasia • Simple hyperplasia • Proliferative endometrium • Secretory endometrium Vicki is a 60 y/o complaining of 3 days of light bleeding 3 weeks ago PMH: Illnesses: diabetes controlled on diet mild hypertension Meds: Atenolol Continuous hormone replacement therapy Exam: 5’4”, 175 lb Pelvic:vagina slightly atrophic cervix stenotic, pap done uterus NS/NS adenexa negative Endometrial thickness • < 4 mm generally atrophic endometrium • > 4 mm you can’t rule out cancer 60 yr old menopausal female complaining of incontinence PI: leaking urine for several months now worse PMH: TAH/BSO for benign disease age 45 Lumbar disk fusion 1 years ago PE: Pelvic – 1st degree cystocoele and 1st degree rectocoele • Complaining of urgency, frequency, nocturia, sudden loss of large amounts of urine • Residual urine 10 ml • Urine culture positive > 100,000 e-coli • Loss of urine with coughing, sneezing, laughing, squatting, jumping • Residual 50 ml and culture negative • Residual > 200 ml 22 yr old female complaining of amenorrhea for 1 yr PI: LMP 1 yr ago prior menstral formula 28d/5d BC: none Gyn Hx delivered a baby 2 yrs ago PMH: Schizophrenic on anti-psychotic med Soc Hx: Occasionally sexually active without condoms PE: Thin female, no distress Breasts bilateral milky discharge Pelvic exam normal • Prolactin 100 ng/ml., TSH 5.5 uU/ml., • Prolactin, TSH normal