Chapter 21: The Thigh, Hip, Groin, and Pelvis
advertisement

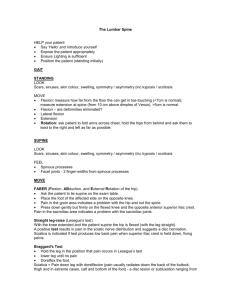
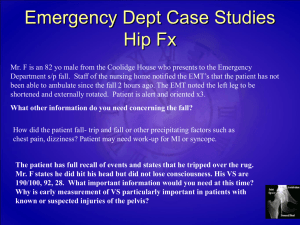
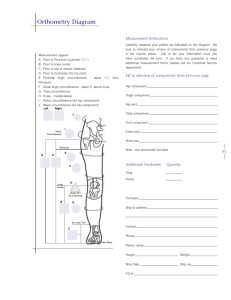
Chapter 21: The Thigh, Hip, Groin, and Pelvis Anatomy of the Thigh Nerve and Blood Supply • Tibial and common peroneal are given rise from the sacral plexus which form the largest nerve in the body the sciatic nerve complex • The main arteries of the thigh are the deep circumflex femoral, deep femoral, and femoral artery • The two main veins are the superficial great saphenous and the femoral vein Fascia • The fascia lata femoris is part of the deep fascia that invests the thigh musculature • Thick anteriorly, laterally and posteriorly but thin on the medial side • Iliotibial track (IT-band) is located laterally serving as the attachment for the tensor fascia lata and greater aspect of the gluteus maximum Functional Anatomy of the Thigh • Quadriceps insert in a common tendon to the proximal patella • Rectus femoris is the only quad muscle that crosses the hip – Extends knee and flexes the hip • Important to distinguish between hip flexors relative to injury for both treatment and rehab programs • Hamstrings cross the knee joint posteriorly and all except the short of head of the biceps crosses the hip • Bi-articulate muscles produce forces dependent upon position of both knee and hip joints • Position of the knee and hip during movement and MOI play important roles and provide information to utilize w/ rehab and prevention of hamstring injuries Assessment of the Thigh • History – – – – Onset (sudden or slow?) Previous history? Mechanism of injury? Pain description, intensity, quality, duration, type and location? • Observation – – – – – Symmetry? Size, deformity, swelling, discoloration? Skin color and texture? Is athlete in obvious pain? Is the athlete willing to move the thigh? •Palpation: Bony and Soft Tissue • Medial and lateral femoral condyles • Greater trochanter • Lesser trochanter • Anterior superior iliac spine (ASIS) • Sartorius • Rectus femoris • Vastus lateralis • • • • • • Vastus medialis Vastus intermedius Semimembranosis Semitendinosis Biceps femoris Adductor brevis, longus and magnus • Gracilis • Sartorius •Palpation: Soft Tissue (continued) • Pectineus • Iliotibial Band (ITband) • Gluteus medius • Tensor fasciae latae • Special Tests – If a fracture is suspected the following tests are not performed – Beginning in extension, the knee is passively flexed • A normal muscle will elicit full range of motion pain free (one w/ swelling or spasm will have restricted motion) – Active movement from flexion to extension • Strong and painful may indicate muscle strain • Weak and pain free may indicate 3rd degree or partial rupture – Muscle weakness against an isometric resistance may indicate nerve injury Prevention of Thigh Injuries • Thigh must have maximum strength, endurance, and extensibility to withstand strain • In collision sports thigh guards are mandatory to prevent injuries Recognition and Management of Thigh Injuries • Quadriceps Contusions – Etiology • Constantly exposed to traumatic blunt blow • Contusions usually develop as a result of severe impact • Extent of force and degree of thigh relaxation determine depth and functional disruption that occurs – Signs and Symptoms • Pain, transitory loss of function, immediate effusion with palpable swollen area • Graded 1-4 = superficial to deep with increasing loss of function (decreased ROM, strength) Quad Contusion • Management – RICE, NSAID’s and analgesics – Crutches for more severe cases – Aspiration of hematoma is possible – Following exercise or re-injury, continued use of ice – Follow-up care consists of ROM, and PRE w/in pain free range – Heat, massage and ultrasound to prevent myositis ossificans – General rehab should be conservative – Ice w/ gentle stretching w/ a gradual transition to heat following acute stages – Elastic wrap should be used for support – Exercises should be graduated from stretching to swimming and then jogging and running – Restrict exercise if pain occurs – May require surgery of herniated muscle or aspiration – Once an athlete has sustained a severe contusion, great care must be taken to avoid another • Myositis Ossificans Traumatica – Etiology • Formation of ectopic bone following repeated blunt trauma (disruption of muscle fibers, capillaries, fibrous connective tissue, and periosteum) • Gradual deposit of calcium and bone formation • May be the result of improper thigh contusion treatment (too aggressive) – Signs and Symptoms • X-ray shows calcium deposit 2-6 weeks following injury • Pain, weakness, swelling, decreased ROM • Tissue tension and point tenderness w/ – Management • Treatment must be conservative • May require surgical removal if too painful and restricts motion (after one year - remove too early and it may come back) • Quadriceps Muscle Strain – Etiology • Sudden stretch when athlete falls on bent knee or experiences sudden contraction • Associated with weakened or over constricted muscle – Signs and Symptoms • Peripheral tear causes fewer symptoms than deeper tear • Pain, point tenderness, spasm, loss of function and little discoloration • Complete tear may live athlete w/ little disability and discomfort but with some deformity – Management • RICE, NSAID’s and analgesics • Manage swelling, compression, crutches • Move into isometrics and stretching as healing progresses • Neoprene sleeve may provide some added support • Hamstring Muscle Strains (second most common thigh injury) – Etiology • Multiple theories of injury – Hamstring and quad contract together – Change in role from hip extender to knee flexor – Fatigue, posture, leg length discrepancy, lack of flexibility, strength imbalances, – Signs and Symptoms • Muscle belly or point of attachment pain • Capillary hemorrhage, pain, loss of function and possible discoloration • Grade 1 - soreness during movement and point tenderness (<20% of fibers torn( • Grade 2 - partial tear, identified by sharp snap or tear, severe pain, and loss of function (<70% of fiber torn) – Signs and Symptoms (continued) • Grade 3 - Rupturing of tendinous or muscular tissue, involving major hemorrhage and disability, edema, loss of function, ecchymosis, palpable mass or gap • >70% muscle fiber tearing – Management • RICE, NSAID’s and analgesics • Grade I - don’t resume full activity until complete function restored • Grade 2 and 3 should be treated conservatively w/ gradual return to stretching and strengthening in later stages of healing (modalities and isometrics) • When soreness is eliminated, isotonic leg curls can be introduced (focus on eccentrics) • Recovery may require months to a full year • Greater scaring = greater recurrence of injury • Acute Femoral Fractures – Etiology • Generally involving shaft and requiring great force • Occurs in middle third due to structure and point of contact – Signs and Symptoms • Pain, swelling, deformity – Management • Treat for shock, verify neurovascular status, splint before moving, reduce following X-ray • Analgesics and ice • Extensive soft tissue damage will also occur as bones will displace due to muscle force • Femoral Stress Fractures – Etiology • Overuse (10-25% of all stress fractures) • Excessive downhill running or jumping activities • Compression or distraction fracture generally occur – Signs and Symptoms • Persistent pain in thigh • X-ray or bone scan will reveal fracture • Commonly seen in femoral neck – Management • Analgesics, NSAID’s RICE • ROM and PRE exercises are carried out w/ pain free ROM • Rest, limited weight bearing • Complete stress fracture may require pins Anatomy of the Hip, Groin and Pelvic Region Functional Anatomy • Pelvis moves in three planes through muscle function – Anterior tilting changes degree of lumbar lordosis, lateral tilting changes degree of hip abduction • Hip is a true ball and socket joint w/ intrinsic stability • Hip also moves in all three planes, particularly during gait (body’s relative center of gravity) • Tremendous forces occur at the hip during varying degrees of locomotion • Muscles are most commonly injured in this region • Numerous injuries attach in this region and therefore injury to one can be very disabling and Assessment of the Hip and Pelvis • Body’s center of gravity is located just anterior to the sacrum • Injuries to the hip or pelvis cause major disability in the lower limbs, trunk or both • Low back may also become involved due to proximity • History – – – – Onset (sudden or slow?) Previous history? Mechanism of injury? Pain description, intensity, quality, duration, type and location? • Observation – Symmetry- hips, pelvis tilt (anterior/posterior) • Lordosis or flat back – Lower limb alignment • Knees, patella, feet – Pelvic landmarks (ASIS, PSIS, iliac crest) – Standing on one leg • Pubic symphysis pain or drop on one side – Ambulation • Walking, sitting - pain will result in movement distortion •Palpation: Bony • Iliac crest • Anterior superior iliac spine (ASIS) • Anterior inferior iliac spin (AIIS) • Posterior superior iliac spine (PSIS) • • • • • Pubic symphysis Ischial tuberosity Greater trochanter Femoral neck •Palpation: Soft Tissue • • • • • • Rectus femoris Sartorius Iliopsoas Inguinal ligament Gracilis Adductor magnus, longus & brevis • Pectineus • Gluteus maximus, medius & minimus • Piriformis • Hamstrings • Tensor fasciae latae • Iliotibial Band - Major regions of concern are the groin, femoral triangle, sciatic nerve, lymph nodes Special Tests • Functional Evaluation – ROM, strength tests – Hip adduction, abduction, flexion, extension, internal and external rotation • Tests for Hip Flexor Tightness – Kendall test – for rectus femoris (hip flexor) tightness • Supine, injured leg flexed to chest, uninjured leg flexed off table • (+) tightness = uninjured leg moves off table with inj hip flexion Kendall’s Test •Femoral Anteversion (A) and Retroversion (B) – Relationship between neck and shaft of femur – Normal angle is 15 degrees anterior to the long axis of the femur and condyles – Internal rotation in excess of 35 degrees is indicative of anteversion, 45 degrees of external rotation is an indicator of retroversion •Test for Hip and Sacroiliac Joint • Patrick Test (FABER) – Detects pathological conditions of the hip and SI joint – Pain may be felt in the hip or SI joint •Testing the Tensor Fasciae Latae and Iliotibial Band • Renne’s test – Athlete stands w/ knee bent at 30-40 degrees – Positive response of TFL tightness occurs when pain is felt at lateral femoral condyle • Nobel’s Test – Lying supine the athlete’s knee is flexed to 90 degrees – Pressure is applied to lateral femoral condyle while knee is extended – Pain at 30 degrees at lateral femoral condyle indicates a positive test • Ober’s Test – Used to determine presence of contracted TFL or IT-band – Knee flexed to 90 and leg abducted as far as possible. – (+) = When released, thigh will remain in abducted position, not falling into adduction •Trendelenburg’s Test - Iliac crest on unaffected side should be higher when standing on one leg - Test is positive when affected side is higher indicating weak abductors (glut medius) • Measuring Leg Length Discrepancy – With inactive individual, difference of more that 1” may produce symptoms – Active individuals may experience problems w/ as little 3mm (1/8”) difference – Can cause cumulative stresses to lower limbs, hips, pelvis or low back – True or anatomical • Shortening may be equal throughout limb or localized w/in femur or lower leg • Measurement taken from medial malleolus to ASIS – Apparent or functional • Result of lateral pelvic tilt or from a flexion or adduction deformity • Measurement is taken from umbilicus to medial malleolus – True or anatomical • Shortening may be equal throughout limb or localized w/in femur or lower leg • Measurement taken from medial malleolus to ASIS – Apparent or functional • Result of lateral pelvic tilt or from a flexion or adduction deformity • Measurement is taken from umbilicus to medial malleolus Leg Length Discrepancy Measures Recognition and Management of Specific Hip, Groin, and Pelvic Injuries • Groin Strain – Etiology • One of the more difficult problems to diagnose • generally adductor muscle group • Occurs from running , jumping, twisting w/ hip external rotation or severe stretch – Signs and Symptoms • Sudden twinge or tearing during active movement • Produce pain, weakness, and internal hemorrhaging • Groin Strain (continued) – Management • RICE, NSAID’s and analgesics for 48-72 hours • Rest is critical; daily whirlpool and cryotherapy, moving into ultrasound • Delay exercise until pain free • Restore normal ROM and strength -- provide support w/ wrap • Trochanteric Bursitis – Etiology • Inflammation at the site where the gluteus medius ties into the IT-band – Signs and Symptoms • Complaint of lateral hip pain that may radiate down the leg • Palpation reveals tenderness over lateral aspect of greater trochanter • IT-band and TFL tests should be performed – Management • RICE, NSAID’s and analgesics • ROM and PRE directed toward hip abductors and external rotators • Phonophoresis if pain doesn’t respond in 3-4 days • Look at biomechanics and Q-angle • Avoid inclined surfaces; • Sprains of the Hip Joint – Etiology • Due to substantial support, any unusual movement exceeding normal ROM may result in damage • Force from opponent/object or trunk forced over planted foot in opposite direction – Signs and Symptoms • Signs of acute injury and inability to circumduct hip • Similar S & S to stress fracture • Pain in hip region, w/ hip rotation increasing pain – Management • • • • X-rays or MRI should be performed to rule out fx RICE, NSAID’s and analgesics Depending on severity, crutches may be required ROM and PRE are delayed until hip is pain free • Dislocated Hip – Etiology • Rarely occurs in sport • Result of traumatic force directed along the long axis of the femur (posterior dislocation w/ hip flexed and adducted and knee flexed) – Signs and Symptoms • Flexed, adducted and internally rotated hip • Palpation reveals displaced femoral head, posteriorly • Serious pathology – Soft tissue, neurological damage and possible fx – Management • Immediate medical care (blood and nerve supply may be compromised) • Contractures may further complicate reduction • 2 weeks immobilization and crutch use for at least one month • Avascular Necrosis – Etiology • Result of temporary or permanent loss of blood supply to proximal femur • Can be caused by traumatic conditions (hip dislocation), or nontraumatic circumstances (steroids, blood coagulation disorders, excessive alcohol use compromising blood vessels) – Signs and Symptoms • Early stages - possibly no S&S • Joint pain w/ weight bearing progressing to at times of rest • Pain gradually increases (mild to severe) particularly as bone collapse occurs • May limit ROM • Osteoarthritis may develop • Progression of S&S can develop over the course of months to a year • Avascular Necrosis (continued) – Management • Must be referred for X-ray, MRI or CT scan • Must work to improve use of joint, stop further damage and ensure survival of bone and joint • Most cases will ultimately require surgery to repair joint permanently • Conservative treatment involves ROM exercises to maintain ROM; electric stim for bone growth; nonweight bearing if caught early • Medication to treat pain, reduce fatty substances reacting w/ corticosteroids or limit blood clotting in the presence of clotting disorders may limit necrosis Hip Problems in the Young Athlete • Legg Calve’-Perthes Disease (Coxa Plana) – Etiology • Avascular necrosis of the femoral head in child ages 4-10 • Trauma accounts for 25% of cases • Articular cartilage becomes necrotic and flattens – Signs and Symptoms • Pain in groin that can be referred to the abdomen or knee • Limping is also typical • Varying onsets and may exhibit limited ROM •Legg-Calve’-Perthes Disease (continued) • Management – Bed rest to alleviate synovitis – Brace to avoid direct weight bearing – Early treatment and head may reossify and revascularize • Complication – If not treated early, will result in ill-shaping and osteoarthritis in later life • Slipped Capital Femoral Epiphysis – Etiology • Found mostly in boys ages 10-17 who are characteristically tall and thin or obese • May be growth hormone related • 25% of cases are seen in both hips, trauma accounts for 25% • Head slippage on X-ray appears posterior and inferior – Signs and Symptoms • Pain in groin that comes on over weeks or months • Hip and knee pain during passive and active motion; limitations of abduction, flexion, medial rotation and a limp – Management • W/ minor slippage, rest and non-weight bearing may prevent further slippage • Major displacement requires surgery • If undetected or surgery fails severe problems will result • The Snapping Hip Phenomenon – Etiology • Common in young female dancers, gymnasts, hurdlers • Habitual movement predispose muscles around hip to become imbalanced (lateral rotation and flexion) • Related to structurally narrow pelvis, increased hip abduction and limited lateral rotation • Hip stability is compromised – Signs and Symptoms • Pain w/ balancing on one leg, possible inflammation – Management • Focus on cryotherapy and ultrasound to stretch musculature and strengthen weak musculature in hip region Pelvic Conditions • Athletes can suffer serious acute and chronic injuries to the pelvic region • Pelvis rotates along longitudinal axis when running, proportionate to the amount of arm swing • Also tilts as legs engage support and nonsupport • Combination of motion causes shearing and changes in lordosis throughout activity • Contusion (hip pointer) – Etiology • Contusion of iliac crest or abdominal musculature • Result of direct blow (same MOI for iliac crest fx and epiphyseal separation – Signs and Symptoms • Pain, spasm, and transitory paralysis of soft structures • Decreased rotation of trunk or thigh/hip flexion due to pain – Management • • • • RICE for at least 48 hours, NSAID’s, Bed rest 1-2 days Referral must be made, X-ray Ice massage, ultrasound, occasionally steroid injection Recovery lasts 1-3 weeks • Osteitis Pubis – Etiology • Seen in distance runners • Repetitive stress on pubic symphysis and adjacent muscles – Signs and Symptoms • • • • Chronic pain and inflammation of groin Point tenderness on pubic tubercle Pain w/ running, sit-ups and squats Acute case may be the result of bicycle seat – Management • Rest, NSAID’s and gradual return to activity • Athletic Pubalgia – Etiology • Chronic pubic region pain caused by repetitive stress to pubic symphysis from kicking, twisting, or cutting – Forced adduction, from hyperextended position, creates shearing forces that are transmitted through pubic symphysis to insertion of rectus abdominus, hip adductors and conjoined tendon – Result in microtears of tranversalis abdominis fascia, aponeurosis of obliques, or conjoined tightness – Create weakening of anterior wall and inguinal canal – Signs and Symptoms • No presence of hernia • Chronic pain during exertion, sharp and burning that later radiates into adductors and testicles – Signs and Symptoms (continued) • Point tenderness on pubic tubercle • Pain increased w/ resisted hip flexion, internal rotation, abdominal contraction, resisted hip adduction (adductors not painful = adductor strain) – Management • • • • • Conservative treatment (even though rarely effective) Massage, stretching after 1 week of surrounding musculature 2 weeks, strengthening of abs and hip flexors and adductors 3-4 weeks begin running progression Aggressive treatment involves cortisone injection or tightening of pelvic wall surgically • Stress Fractures – Etiology • Seen in distance runners - repetitive cyclical forces from ground reaction force • More common in women than men • Common site include inferior pubic ramus, femoral neck and subtrochanteric area of femur – Signs and Symptoms • Groin pain, w/ aching sensation in thigh that increases w/ activity and decreases w/ rest • Standing on one leg may be impossible • Deep palpation results in point tenderness • Intense interval or competitive racing may cause • Stress Fractures (continued) – Management • Rest for 2-5 months • Crutch walking for ischium and pubis fractures • X-ray normal 6-10 weeks and bone scan will be required • Swimming can be used -- breast stroke avoided • Avulsion Fractures and Apophysitis – Etiology • Traction epiphysis (bone outgrowth) • Common sites include ischial tuberosity, AIIS, and ASIS • Avulsions seen in sports w/ sudden accelerations and decelerations – Signs and Symptoms • Sudden localized pain w/ limited movement • Pain, swelling, point tenderness • Muscle testing increases pain • Avulsion Fractures and Apophysitis – Management • X-ray • If uncomplicated, RICE, NSAID’s, crutch toe-touch walking • After control pain and inflammation, 2-3 weeks of gradual stretching • When 80 degrees of ROM have been regained, athlete can return to competition Thigh and Hip Rehabilitation Techniques • General Body Conditioning – Must maintain cardiovascular fitness, muscle endurance and strength of total body – Avoid weight bearing activities if painful • Flexibility – Regaining pain free ROM is a primary concern – Progress from passive to PNF stretching Mobilization • Will be necessary if injury and subsequent limitation is caused by tightness of ligaments and capsule surrounding the joint • Use to re-establish appropriate arthrokinematics • Series of glides (anterior and posterior) and rotations can be used to restore motion Strength • Progression should move from isometric exercises until muscle can be fully contracted to isotonic strengthening PRE’s into isokinetics • PNF strengthening should then be incorporated to enhance functional activity • Active exercise should occur in pain free ranges -- in an effort not to aggravate condition • Exercises for the core must also be included – Develop optimal levels of functional strength and dynamic stabilization Neuromuscular Control • Establish through combination of appropriate postural alignment and stability strength • As neuromuscular control is enhanced, the ability of the kinetic chain to maintain appropriate forces and dynamic stabilization increases • Focus on balance and closed kinetic chain activities Balance Shoe for Neuromuscular Control Functional Progression and Return to Activity • Begin in pool, non-weight bearing • Depending on activity, progression of walking, to jogging, to running and more difficult agility tasks can occur • Before returning to play, athlete should demonstrate pain free function, full ROM, strength, balance and agility