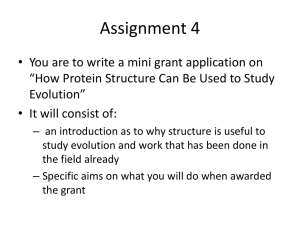
PPT - University of California | Office of The President
advertisement

Impact of Electronics in the
Healthcare Setting
Susan L. Penney, JD
David Robinowitz, MD
Heidi Collins
UCSF Medical Center
The Train Has Left the Station
Goal:
Know & Manage the Risks, Benefits & Alternatives
Of the E-World
Overview
• Unexpected photos videos
• Posting about work
environment, patient care
• Disease Management Sites
• Patient Portals
• E-mailing with Patients
• Documentation
• E-Discovery
• Privileged Communications on
the Internet
• Posting Test Results
• Medical Record Amendments
• E-Consultations
• Texting Risks
3
Do you have a Social Media Site?
• Hospital or medical group social media
hosted sites—you are asking patients
to comment on your business?
• What happens if a patient posts an
unflattering review?
4
Websites—the good and the bad
•
Websites used for marketing, but you want to
be careful of false advertising
•
Watch out for advertisements with
endorsements
•
Disclaimers on websites are really important
•
Transparency of Quality Data: Joint
Commission and litigation use
Websites and the ADA-evolving
rules
•
Access by blind, deaf or patients with manual
dexterity limitations
•
ADA Title III: must provide auxiliary aids and
services necessary to ensure equal access—this
includes electronic and information technology
•
2010 Statement confirms that websites that
provide goods and services must be accessible
http://www.reginfo.gov/public/do/eAgendaViewRu
le?pubId=201210&RIN=1190-AA61
Patients filming and posting on
YouTube
Joe has quite a few psycho-social issues
He has gone to many public official locations
and filmed individuals to further his opinion that
the world is a corrupt place
He comes into a hospital’s outpatient clinic and
begins to film your staff –he isn’t even a patient
He then posts the films on YouTube and makes
derogatory comments
What do you do?
7
Filming
• It is illegal to film or record an image or voice
without permission
• Penal Code section 632;
• Civil Code section 3344
• Make it clear in your photography policy
• Educate staff and physicians
• Terms and Conditions/patients’ rights and
responsibilities can reiterate this
8
Removal of posting Social Media
Sites
•
Most sites have a privacy complaint process
e.g. YouTube
www.youtube.com/t/privacy_guidelines
•
Person whose image is inappropriately posted
usually must make the complaint—eg. They
usually require that the image allows others to
recognize you
•
Cease and Desist letters can mirror the
language of the site’s privacy policy
Responding to Negative comments
•
Privately respond and address concern and ask
them to remove—but opinion may not be
removable
•
Counter act with positive stories, But don’t:
•
Have patients sign agreements not to post
•
Make up positive fiction
•
Respond with PHI to explain
•
Attack the poster
10
Employment Issues
• Employee made a request from his manager
• Confidential discussion between manager and
employee
• Employee dissatisfied with the manager’s
response
• Employee goes to the Facebook page and trashes
the manager-mentions the facility
• Question: Can anything be done about the
employee’s behavior?
• Freedom speech?
• Slander/libel?
• Institutional reputation?
Discussing Work Activity
• TJC survey is on-going
• Surveyor comes to a nursing unit
• Nurse gets on Facebook after surveyor visit
• Discusses other nurses’ performance
• Opines on probability of
re-accreditation issues
• Identifies patient room number
• What do you do?
Balancing:
Employees’ Rights:
•Speech
•Organizing
•Privacy
With…
Employers’ Rights
•Reputation
•Privacy
•Patient Safety
Employment activity
•
NLRB has issued advice memos related to social
media policies http://www.nlrb.gov/newsoutreach/fact-sheets/nlrb-and-social-media
•
Employees cannot say anything they want: Not
protected includes:
•
Disparagement of company’s or competitors’
products, services, executive leadership, employees,
strategy and business prospects
Expectation of Privacy?
•
Billy has had several workers comp claims but
there is something fishy going on
•
One of Billy’s co-employees shows Billy’s
manager some Facebook posts showing Billy
demonstrating extraordinary physical abilities
•
The posts are used to deny the workers comp
claim
•
Is this ok?
Multi-Tasking?
•
Everyone said that the sponge count was
correct, but the day after surgery, one was
identified.
•
Nurses said they followed the policy but felt
rushed to do the count
•
In a subsequent investigation/litigation,
attorneys identify nurse’s Facebook post made
during the surgery…..oops
Ethical issues of Social Media story
telling
Health care providers often share clinical stories on
social media:
•To reflect a meaningful experience
•Reach out for social support
The problem with this practice:
•Undermines the public trust in the profession
•Inadvertently identifies patients
•Violates expectations of privacy even if it doesn’t ID
the patient*
* University of Washington study “Sounding off on Social media”
Your Policy:
Reasonable terms
• Facility sponsored blogs or social media must
be approved to ensure:
• Compliance with Privacy rules
• That content is appropriate
• Use of facility name and logo is appropriate
• Consent rules must be followed
• Assert that facility has the right to suspend
blog activity if deemed inappropriate
• For sponsored sites, require notification if
knowledge of privacy breach
Friending Patients
• Develop Guidelines on Social Media
http://www.ucsf.edu/about/social-media-guidelines
• Risk recommends that you maintain clear
separation between personal and professional life
• Advise patients that you have a policy of not
friending patients and stick to it.
• Remember, if your “friend” a patient, if will likely
impact other providers because they will get
“friend” requests
• In general, be very careful about sharing personal
information with patients
19
Reasonable Policy Terms
• For institutional sponsored social media: prohibit
referrals or product endorsements
• Indemnification agreements for violations of law
Don’t forget the obligation for training
and policies related to privacy!!
Web Based Disease Management,
Advice Lines and Chat Rooms
• Often designed to increase referrals
• Need to consider
• Telemedicine rules
• Privacy Rules
• Rules of use, consider
• Reserve the right to censor, remove or ban for
• Sexual conversation, racial animus, glorification
of addiction, politics, software piracy, religious
discussion or disrespectful discussion
21
Blogs where health conditions are
discussed
Make sure to include a disclaimer related to
medical advice
• “We hope that the information obtained on this site will help
you to be better able to participate with your health care
providers in making informed decisions about your care. It
is not a substitute for appropriate professional medical
treatment or diagnosis. Always seek the advice of your
physician or other qualified health provider with any
questions you may have regarding a medical condition.
Never disregard professional medical advice or delay in
seeking it because of something you have read on this site.
Except where explicitly stated otherwise, it is not intended
as specific medical advice. Neither the institution nor its
officers, agents or employees assume any legal liability or
responsibility for the accuracy, completeness or usefulness
of any information, apparatus, product or medical
procedure described.”
Internet research to make
healthcare decisions
• Research varies widely on patient demographics
of internet research: 1/3 to 85%
• Even if patients use the web, the vast majority
base health decisions primarily on the information
provided by their physicians
• There is inconclusive data on what happens when
the patient brings internet data to the attention of
their provider
Internet Research—why are patients
doing it?
• They don’t want to bother the doctor
• More information on the internet than they have
time to discuss with their physician
• They want to show the physician that they have
invested time in their medical concern and want
to be taken seriously
• They are distrustful of their physician (not the
primary reason)
Patients report a wide range of
responses from providers*
•
Listening and acknowledgment
•
Non-verbal cues that they are “checking out”
•
Disregard or fail to acknowledge a lack of
knowledge
•
Accusatory behavior or a patriarchal or
threatened response
*I need her to the a doctor: British Journal of General
Practice November 2012
Patient Portals in your EHR
• Create expectations for response time to
patients/ limitations of use—not for an urgent or
emergent issue
• Have good “terms of use” so that it is clear how
the portal is to be used
• It can be a very efficient way to communicate
• Set rules up for discontinuation from use of
portal if abuse
• Providers are spending more time than ever
before responding to patients at all hours of the
day/night
• Kaiser says physicians on average receive 5 emails a day—is that your experience?
E-mailing with Patients
• Some institutions have changed by-laws to
prohibit using e-mail and allow electronic
communication via patient portal only
• If you don’t use e-mail:
• Reference it in the terms and conditions of admission
• Develop an auto message that states your policy on
how the patient should reach you
• Make sure the patient has an alternative efficient
method of communication
• PROBLEM: A GOAL OF CONSISTENCY AS
BETWEEN PROVIDERS IS UNREALISTIC
• WE ARE ALL DRIVEN BY PATIENT DEMAND &
SATISFACTION:
• “Marketing and listening to your customer should be
good enough reason {to use e-mail}” says a
consultant
27
E-mailing with Patients
• If you do use e-mail:
• Consider a consent form
• Don’t attempt to obtain a “waiver of HIPAA” ---it won’t work
• Move toward a secure e-mail system—internet providers do
not guarantee security but patients may not realize that
• This triggers the need for an IT Security plan to develop filters
so that personal health information (phi) does not leave the
organization
• If you are using personal e-mail for substantive e-mail
exchange, you need a system for transferring that information
to the EHR or the paper medical record—how do you monitor
compliance? (that is why e-mail is not typically included in the
definition of legal health record)
• Consider appropriate management by Allied health providers
within their scope of practice---set rules!! And Watch for Scope
Creep
• Control what you accept from patients via e-mail—external
records
28
Benefits of e-mail
• Prescription refill requests for certain
medications--watch your nurses/MA’s scope of
practice
• Appointment reminders
• Billing
• Administrative matters
• Patient education notification—web based
• Can eliminate phone tag and/or reduce calls
• Can provide documentation if within or
transferred to medical record
29
Benefits of e-mail
• Some studies say it improves quality measures
• Continuity of Care
• Patient-physician connectedness
• Supporting patient self-management
• Patient loyalty
• Getting Paid:
• The world of reasonable reimbursement will have to
catch up to allow physicians to be paid for the value
added and advice.
30
Risks of e-mailing patients
• Use of personal versus professional e-mail
• Storage and backup of e-mail
• Tracking of e-mail and e-mailing during work
hours
• Appropriate use—not for urgent medical advice
• See AMA Guidelines for Physician-Patient
Electronic Communication
http://hosted.ap.org/specials/interactives/_docum
ents/patient_physician_email.pdf
Well intended but risky use of e-mail
to give clinical advice
• 55 year old patient seen in a sports medicine clinic for
hip pain—under went hip surgery
• Prior to surgery, patient had an EKG reported as
“abnormal record, marked sinus bradycardia”
• 3 months after surgery, patient contacts the surgeon
complaining of chest pain while exercising
• The doctor was on vacation, but believes he called the
patient (no documentation)
• Ordered EKG—otherwise normal EKG, sinus
bradycardia
• Patient e-mailed with more pain—no response
• Patient died from heart failure 3 days later
32
Issues
• Is there an on-call system within the physician’s
practice?
• Does the physician have an auto response when
on vacation to manage patient’s expectations?
• None of the e-mail or communication was
documented in the patient’s medical record
• E-mail used was the physician’s personal e-mail
• E-mail gets deleted, e-mail services change, which
reduces the ability to locate e-mail to defend the
case
33
E-Discovery
• Litigation involves a phase called Discovery
• Typical topics of discovery: medical records;
policies and procedures
• California and Federal law now require ediscovery—the production of:
• Texts
• E-mails
• Instant messages
• Telephone messages
• Strong penalties for failure to comply
34
E-Discovery Issues
• Who has control over your electronic
communications?
• Individual physicians are responsible but who
controls their e-mails?
• When is the obligation to retain electronic data
triggered? Adverse Event? Notice of Intent?
• Will need a process for “litigation holds”
• Will need IT specialists or consultants who can
retrieve the data
• Can you assert a privilege related to any of these
communications?
35
Declarations Against Interest
• Patient undergoes a high risk heroic surgery for a
brain tumor—surgery is a success
• Patient develops a Surgical Site Infection with a
rare bug and has a significant set back
• The plaintiff alleges that the surgeon made all
sorts of statements about the cause of the
infection and the treatment for the infection
• The surgeon routinely communicated via e-mail
with the patient’s family
• Over 500 e-mails were retrieved from the
surgeon’s e-mail alone...what do they say?
36
Communication re Quality Reviews
• Evidence Code section 1157 allows for the
confidentiality of the activities of medical staff
committees related to quality and patient safety
activity
• Committee activity has evolved to include e-mail
communication and follow-up
• Update policies as to what constitutes the
activities of these committees
• Properly label the e-mail communications to
identify 1157 Activity
• Assert the privilege
37
Other Risks and Benefits
• Auto release of test results—unintended
consequences
• Patients’ misinterpretation of test results
• Radiology results—are radiologists ready to receive
calls from patients?
• Providers lulled into false sense of security that patient
has seen the results, resulting in the risk that:
• The physician will not review and act on results
• Follow up may not occur
• Providers who do not check their message inbasket—same problem, new system
• Managing in-basket with a pool—manage carefully!
Other Risks and Benefits
• Sharing the problem list with patients
• Increased requests for medical record amendments
• Make sure your providers know the rules
• Alcohol and substance use—will a patient ever
agree?
• Does the patient see the diagnosis of
• Schizophrenia or Munchausen by Proxy?
The Problem with Problem Lists
• Many web based patient portals allow patients to
view their problem lists
• We have seen a dramatic increase in patient
requests for medical record amendments
40
The Merchant Marine Applicant
• Patient presents to the GI clinic and a history is
taken by a resident
• The history includes the patient’s report that he
smokes marijuana
• Subsequent to the visit, the patient applies to be a
merchant marine—records are sent
• The patient sees on his problem list the use of
marijuana and wants the record changed
• The physician amended the record because of the
plaintiff’s pressure that he would be denied by
Merchant Marines
41
Amendments and Addendums to the
Medical Record
• The use of a patient portal and the patient’s ability
to see his or her problem list or history should not
change your policy on when medical record
amendments should be made
• Changes should be made if there was an error, not
because the patient disagrees with the note
• Difficult to manage for sensitive diagnoses
• Physicians would benefit from education/support in
managing these requests.
42
Texting
• Studies are showing that providers are texting
during surgery or other work activity
• And the new generation thinks that texting is a
nifty way to send orders?
• Joint Commission standards prohibit texting of
orders
http://www.jointcommission.org/standards_infor
mation/jcfaqdetails.aspx?standardsFAQid=401&
StandardsFAQChapterd=79
Joint Commission FAQ’s
• Texting Orders New | November 10, 2011
• Is it acceptable for physicians and licensed
independent practitioners (and other practitioners
allowed to write orders) to text orders for patients to
the hospital or other healthcare setting?
• No it is not acceptable for physicians or licensed
independent practitioners to text orders for patients
to the hospital or other healthcare setting. This
method provides no ability to verify the identity of
the person sending the text and there is no way to
keep the original message as validation of what is
entered into the medical record.
Texting Risks--15 Year Old
Neurosurgery Patient
• 15 year old underwent spine surgery
• On the unit, issue as to whether there should be
neuro checks q 4 hours.
• Post-op orders were confusing
• Post-op, a resident attempted a hand-off to
another resident by sending a text instructing
them to do a post-op exam
• The resident did not confirm receipt of the text,
sent it to a device not working and no post op
exam was done
• The following morning the patient was found to be
paraplegic
Texting and other electronic
communication
• Develop clear guidelines on what constitutes a
hand off
• Mandate confirmation of receipt of
communication
• Develop rules of accountability
• Develop rules of supervision
46
Limit your risk related to Texting
because you can’t stop it
• No personal health information
• Workforce training—especially your young staff
and trainees
• Encrypt and password protect
• Require note in medical record when
information received by text influences a
medical decision
Conclusion
• The Web has changed the world and there is no
going back
• Patient demand is important, but avoid the
response “if the patient wants it, we must do it”
• Manage the issue with
• policy
• training
• quality reviews
• Rules of the road
• Consent
48
The Best of all Worlds
Enterprise Risk Management for the E-world
IT, Clinical Users
& Medical
Records Dept
Regulatory,
Compliance &
Legal
Privacy &
Operations
Planning requires the willingness to
understand stakeholders’ points of view
Risk
Management &
Defense Counsel
Finance &
Strategic
Planning
What is Standard of Care Related to EHR?
• EHR systems can allow unlimited scanning of outside
records
• Some hospitals for particular referral programs are
allowed access to another facility’s record for a patient.
E.g. transplant
• “Care Everywhere” allows Emergency Departments
immediate access to records from other facilities
but…
What is the standard for accountability for knowing or acting
on shared information?
Suggestion: when drafting agreements and consent forms
include disclaimer that review of record will depend upon
patient’s condition and urgency of care
The Anesthetic Record
What is the purpose of the anesthetic record?
“The goal of the anesthetic record is to capture a
patient’s response to anesthesia and surgery by
recording the procedures, physiologic changes,
key events, and pharmacologic administration
that occur throughout the perioperative period.” 1
1. Kadry, B., Feaster, W. W., Macario, A. & Ehrenfeld, J. M. Anesthesia
information management systems: past, present, and future of
anesthesia records. Mt Sinai J Med 79, 154-165 (2012).
Limitations of Paper Records1
• Recall Bias
• Data analysis requires manual chart review
• Illegible (or impressionistic) records
• Lost/missing records
• Incomplete data – issues with documentation
of compliance and billing requirements
• Handwritten records may have less
medicolegal “heft” (no audit trail)
1.
Kadry, B., Feaster, W. W., Macario, A. & Ehrenfeld, J. M. Anesthesia information
management systems: past, present, and future of anesthesia records. Mt Sinai J Med 79,
154-165 (2012).
History of AIMS
• First AIMS was mechanical device (E. I. McKesson
1930’s) to record
1. Featherstone, R. J., Adams, C. N. & Bacon, D.
R. Physiological monitoring and record-keeping
in anaesthesia - an unrecorded contribution.
American Society of Anesthesiologists (2012).
History of AIMS
• 1950’s – 1990’s development of automated anesthesia
record keepers (AARKs)
– Limited by availability of sophisticated, inexpensive, and
reliable hardware and software1
– Pioneering Systems2
• DAME (Duke Anesthesia Monitoring
Equipment)
– A few ORs at Duke
• ARKIVE (Anesthesia Record Keeper
Integrating Voice Recognition)
– Installed at Vero Beach, Duke, and Fitchburg
• 1990’s – slow rollout of commercial products
1.
2.
Shah, N. J., Tremper, K. K. & Kheterpal, S. Anatomy of
an anesthesia information management system.
Anesthesiol Clin 29, 355-365 (2011).
Stonemetz, J. Anesthesia information management
systems marketplace and current vendors. Anesthesiol
Clin 29, 367-375 (2011).
AIMS – Adoption Challenges
• Usability
– Concerns of decreased productivity
– Technology Adoption Model
• System will be used against me1
• Return on Investment
– ~$25,000 per anesthetic location
1.
2.
Stonemetz, J. Anesthesia information management systems marketplace and current
vendors. Anesthesiol Clin 29, 367-375 (2011).
Vigoda, M. M., Rothman, B. & Green, J. A. Shortcomings and challenges of information
system adoption. Anesthesiol Clin 29, 397-412 (2011).
AIMS Prevalence: 20071
~ 44% of US Academic Medical Centers had implemented an AIMS
or were in process…
1. Egger Halbeis, C. B., Epstein, R. H., Macario, A.,
Pearl, R. G. & Grunwald, Z. Adoption of anesthesia
information management systems by academic
departments in the United States. Anesth Analg 107,
1323-1329 (2008).
AIMS Prevalence: 2013 & Beyond1
Survey of US Academic
medical centers
• By 2014, approximately
75% will have AIMS
installed
• Logistic regression predicts
that 84% will have AIMS by
2018-2020
• Academic medical centers
are outpacing private
practices
• It is possible that within a
few years, trainees will
graduate from anesthesia
residencies never having
used a paper record.
1. Stol, I. S., Ehrenfeld, J. M. & Epstein, R. H. Technology
diffusion of anesthesia information management systems
into academic anesthesia departments in the United
States. Anesth Analg 118, 644-650 (2014).
Benefits of AIMS
Improved Quality of
Care?
Anesthesiologists can focus on higher level
tasks in lieu of charting data
vs.
Loss of vigilance or situational awareness
AIMS and Situational Awareness
The act of recording information on the chart
forces the anesthesiologist to be aware of the time course
and detail of anesthetic events. This awareness is the most
important factor in anticipating future events, and
correcting untoward events. A mechanically created record
… has the capacity to be formed without ever passing
through the consciousness of the anesthesiologist… The
effort to create automated anesthetic records, while
interesting technical exercises, are dangerous, because
they bypass the anesthesiologist, making it easier for
essential information to go unrecognized.
- Theodore Noel, 1986
1. Noel, T. A. Computerized anesthesia
records may be dangerous.
Anesthesiology 64(2), 300 (1986).
Deeper limitation of graphical paper records
(and AARK): What’s the story?
• Both traditional written anesthesia record and the
AARK have been criticized as poor vehicles for telling
the story of an anesthetic.
“The current anesthesia record whether handwritten, or
automatic, is mindless.”1
Answered in part by “Case Summary Note” and ongoing
free text notes in which commentary and narrative can
be stored? Or increased sophistication of meta-data?
(more later)
1. Zeitlin, G. L. History of anesthesia records.
ASA Newsletter APSF 25th Anniversary
Edition, 26-29 (2011).
AIMS and Clinical Practice
Task Analysis: Manual Recording
• Analysis of 3 CABG cases in a teaching hospital, 1976
• 10-15% of time spent “logging data on anesthetic record.”
• Recommended adoption of electronic system to record data
automatically
1. Kennedy, P. J., Feingold, A., Wiener, E. L. & Hosek, R.
S. Analysis of tasks and human factors in anesthesia for
coronary-artery bypass. Anesth Analg 55, 374-377 (1976).
AIMS and Clinical Practice
Task Analysis: Manual Recording
• UCSD 1994 task analysis, workload, and
vigilance study – 11 GETA cases by new junior
residents vs. 11 GETA cases by senior residents
and experienced CRNAs
• Pre-intubation 0.9 vs. 0.4 mins mean time spent
on recording
• Post-intubation 13.9 vs. 9.4 mins
1. Weinger, M. B. et al. An objective methodology for
task analysis and workload assessment in
anesthesia providers. Anesthesiology 80, 77-92
(1994).
AIMS and Clinical Practice
Task Analysis: Manual Recording
1. Weinger, M. B. et al. An objective methodology for
task analysis and workload assessment in
anesthesia providers. Anesthesiology 80, 77-92
(1994).
63
AIMS and Clinical Practice
Vigilance: Electronic vs. Manual
Recording
• Is writing in the paper record necessary or beneficial
for anesthesia provider vigilance?
– 1995 UC Davis Study1 of anesthesia residents
• Manual recording vs. human scribe/assistant
• 36 GA outpatient cases, ASA 1 and 2
• Vigilance assessed by detection rate and
response time to simulated abnormal value
on monitor
• Similar response rates and times for both
groups
1. Loeb, R. G. Manual record keeping is
not necessary for anesthesia
vigilance. J Clin Monit 11, 9-13 (1995).
AIMS and Clinical Practice
Vigilance: Electronic vs. Manual
Recording
1. Loeb, R. G. Manual record keeping is
not necessary for anesthesia
vigilance. J Clin Monit 11, 9-13 (1995).
65
AIMS and Clinical Practice
Vigilance: Electronic vs. Manual
Recording
• Woods and Cognitive Science colleagues at The Ohio State
University criticism of the UC Davis study1
– The automation simulator – the human scribe – “functioned as a team
player: responsive, directable, intelligent, nonintrusive”
– In contrast, automated systems are typically not team players when
they are
• Strong (act autonomously)
• Silent (provide poor feedback)
• Clumsy (interrupt human teammates during high
workload or critical periods; or add mental burdens
during these periods)
• Difficult to direct (costly for human to instruct the
automatic system re: how to change as circumstances
change)
1. Woods, D. D., Cook, R. I. & Billings, C. E.
The impact of technology on physician
cognition and performance. J Clin Monit 11, 58 (1995).
AIMS and Clinical Practice
Task Analysis, Workload, Vigilance:
Electronic vs. Manual Recording
• 1997 Study of senior residents providing anesthesia for
20 CABG cases1
– Randomized to an actual automated system – an electronic
anesthesia record keeper (EARK) or manual recording
– Two groups had similar task distributions by task analysis
– EARK group spent slightly less time record keeping after
intubation and before bypass (more time observing monitors
and talking with attending)
– No significant differences between two groups in self
reported workload scores, workload density (weighted
scores of tasks/minute), or vigilance latency (measured as
response time to randomly activated light)
– (Only 4/20 cases had any record keeping prior to
intubation)
“charting comes last”
1. Weinger, M. B., Herndon, O. W. & Gaba, D. M. The
effect of electronic record keeping and transesophageal
echocardiography on task distribution, workload, and
vigilance during cardiac anesthesia. Anesthesiology 87,
144-55; discussion 29A (1997).
Motivation for AIMS1
• Automated anesthesia record keeper (AARK) is only
one component of an AIMS
– AIMS also includes metadata not necessarily captured
by an AARK
• Case events (e.g. in-room, cross-clamp-on)
• Medication administration
– A full AIMS is an AARK interfaced with numerous
systems such as
• Pharmacy
• Admit/Discharge/Transfer systems
• Laboratory
• Billing
• Perioperative Scheduling
1. Kadry, B., Feaster, W. W., Macario, A. & Ehrenfeld,
J. M. Anesthesia information management systems:
past, present, and future of anesthesia records. Mt
Sinai J Med 79, 154-165 (2012).
One word of caution
• Not all AIMS are created equal
–
–
–
–
–
–
Different vendors/products
Different configurations
Different hardware
Different workflows
Different case mixes
Different cultures
• Design matters!
Interpret literature in this context
AIMS will impact care processes, but alone
cannot fix all problems
AIMS wanted for more than record keeping…
Motivations to adopt AIMS:1 the Black Box
•
Quality/Safety group endorsements
– APSF (2001): “… endorses and advocates the use
of automated record keeping in the perioperative
period and the subsequent retrieval and analysis of
the data to improve patient safety.”2
– Analyze incidents and outcomes data
•Demonstrate compliance1
•Streamline billing processes1
1.
2.
Stonemetz, J. & Lagasse, R. Rationale for purchasing an AIMS,
in Anesthesia informatics (eds Stonemetz, J. & Ruskin, K.) 7-22
(Springer-Verlag London Limited, 2008).
APSF Board of Directors. American Society of Anesthesiologist
Annual Meeting (New Orleans), 2001, Board of Directors Motion.
APSF Newsletter Winter, 2001.
AIMS as AARK
Straightforward AARK serves as
clinical tool
•Decreases charting burden
• Allows the anesthesiologist to
“face the field” and have
greater immediate situational
awareness
Has this fundamental goal been overwhelmed by the
use of AIMS for research, compliance, billing, and other
purposes?
AIMS – Here to Stay
Who wants (or demands)
anesthesia/peri-op data?
• SCIP (CMS, CDC)
•
•
•
•
•
•
•
•
•
NSQIP
The Joint Commission
PQRS
APSF
MOCA
P4P
Private Insurance
Third party payers
Research and Quality
Consortia/Registries
Who else?
• Your medical center,
department, colleagues
• Consumers/potential
patients
• ACGME
And don’t forget
• Benefits of Meaningful use1
– Non-hospital based
anesthesiologists – if EHR
by 2015 up to $44,000$63,750; after 2015 avoid
payment reduction
– Or, support hospital
meaningful use and share
in benefit?
1. Lai, M. & Kheterpal, S. Creating a real return-oninvestment for information system implementation: life after
HITECH. Anesthesiol Clin 29, 413-438 (2011).
AIMS – Here to Stay
Who wants (or demands)
anesthesia/peri-op data?
• SCIP (CMS, CDC)
•
•
•
•
•
•
•
•
•
NSQIP
The Joint Commission
PQRS
APSF
MOCA
P4P
Private Insurance
Third party payers
Research and Quality
Consortia/Registries
Who else?
• Your medical center,
department, colleagues
• Consumers/potential
patients
• ACGME
And don’t forget
• Benefits of Meaningful use1
Medical Center
Lawyers
– Non-hospital based
anesthesiologists – if EHR
by 2015 up to $44,000$63,750; after 2015 avoid
payment reduction
– Or, support hospital
meaningful use and share
in benefit?
1. Lai, M. & Kheterpal, S. Creating a real return-oninvestment for information system implementation: life after
HITECH. Anesthesiol Clin 29, 413-438 (2011).
The Wing Leveler vs. The 787
1.
2.
3.
Popular mechanics
http://www.39pw.us/web/icons/autopilot.jpg accessed 12-March-14
http://en.wikipedia.org/wiki/File:Boeing_787-8_N787BA_cockpit.jpg
by Alex Beltyukov, Creative Commons
74
The Wing Leveler vs. The 787
1.
2.
3.
Popular mechanics
http://www.39pw.us/web/icons/autopilot.jpg accessed 12-March-14
http://en.wikipedia.org/wiki/File:Boeing_787-8_N787BA_cockpit.jpg
by Alex Beltyukov, Creative Commons
Caveat 2:
AIMS – Something for Everyone?
Once there is an AIMS, many parties will have ideas
of what it is:
It’s
•an AARK – decrease anesthesiologist reporting
burden!
•a compliance and liability reduction tool!
•a data acquisition tool for my clinical research
project!
•an improved clinical record keeper to smooth
transition to ICU care!
AIMS – and Clinical Decision
Support
Table from Vakharia, S. B. & Rinehart, J. Using
anesthesia AIMS data in quality management. Int
Anesthesiol Clin 52, 42-52 (2014).
AIMS – Clinical Decision Support
• Alert Criteria Matter
• Design Matters
- See [1] for theory
– Hard Stop
• Human Factors
Engineering
– See [2] for overview
– Modal Dialogue Box
– Audible Alert
– Icon
– CDS on demand
– Messaging
– Photos3
1.
2.
3.
Raymer, K. E., Bergstrom, J. & Nyce, J. M. Anaesthesia monitor alarms: a theory-driven approach.
Ergonomics 55, 1487-1501 (2012).
Weinger, M. B. & Gaba, D. M. Human factors engineering in patient safety. Anesthesiology 120, 801-806
(2014).
Hyman, D., Laire, M., Redmond, D. & Kaplan, D. W. The use of patient pictures and verification screens
to reduce computerized provider order entry errors. Pediatrics 130, e211-e219 (2012).
AIMS – Clinical Decision Support
An alarming issue….
•Excessive AIMS alerts may be
analogous to excessive monitor
alarms and could lead to
alarm/alert fatigue.
•A system for managing these
alerts is recommended. See [1]
for principles for alarm
management
1. American Society of Anesthesiologists
House of Delegates. Statement on
principles for alarm management for
anesthesia professionals. (2013).
AIMS – and Clinical Decision
Support - example
University of Washington AIMS
interface to near real time decision
support engine1
•“Pop-Up” screen alerts for
hypotension in context of high MAC
and hypertension in context of
ongoing phenylephrine infusion
–
–
Reduced frequency and duration of
hypotension-high MAC incidents
Hypertension-phenylephrine
frequency not changed but may
have been affected by
(retrospective) manual recording of
phenylephrine infusion
•Recommended incorporation of CDS
into AIMS, rather than as “add-on” to
increase data sampling frequency
1. Nair, B. G. et al. Anesthesia information
management system-based near real-time decision
support to manage intraoperative hypotension and
hypertension. Anesth Analg 118, 206-214 (2014).
AIMS – and Clinical Decision
Support - example
University of Michigan – AIMS alerting for
patients with potential Acute Lung Injury
(ALI) to promote low tidal volume
ventilation strategy in OR1
• “Just in time” randomized controlled trial
– Enrolled patients with PaO2/fiO2 <
300
– 60,960 patients analyzed; 100
total patients met criteria for
inclusion (had blood gas, > 18
years old, height recorded in
system; and ventilator data
received in AIMS)
– Intervention group received alert
recommending Vt of 6 mm/kg of
Predicted Body Weight
1. Blum, J. M. et al. Automated alerting
– Control group received
and recommendations for the
conventional care with no alert
management of patients with preexisting
•Results: Vt/PBW: control group: 8
mm/kg vs.. intervention: 7.2 mm/kg
hypoxia and potential acute lung injury: a
pilot study. Anesthesiology 119, 295-302
(2013).
AIMS and Risk/Liability
• Background
• Belief that AIMS could increase liability by
• Capturing transient physiologic changes —
of minimal clinical significance — that could be
misinterpreted by consumers of the electronic
record
• Incorporating artifactual data
• Or AIMS could reduce liability by
• Providing a “more contemporaneous,
complete, and legible rendition of actual
events than the handwritten record.”
1. Feldman, J. M. Do anesthesia information
systems increase malpractice exposure? Results
of a survey. Anesth Analg 99, 840-3, table of
contents (2004).
AIMS and Risk/Liability
•
2004 Survey: 22/55 Departments of Anesthesia1 Completely
Responded
•
41 malpractice cases
– 30 dropped
• In 5 of these, AIS helped “document absence of negligence”
– 11 settlement or litigation
• In 5 of these, AIS “facilitated decision to settle”
• For litigation case: 2 instances of AIS assisting defense; no cases in
which AIS hindered the defense
•
18 respondents: AIS valuable for risk management
•
2 respondents: AIS essential for risk management
•
Zero respondents believed AIS to be harmful for risk management.
•
19/22 recommended use of AIS as part of risk management strategy
1. Feldman, J. M. Do anesthesia information
systems increase malpractice exposure? Results
of a survey. Anesth Analg 99, 840-3, table of
contents (2004).
AIMS and Risk/Liability
Selected survey comments1
•“I know of 3 cases where the [automated] anesthesia
record directly contributed to the anesthesiologist
being dismissed (from the case).”
•“We have few suits in part because we have an
electronic anesthetic record.”
•“Concern about artifacts is misplaced – they’re easy
to spot.”
1. Feldman, J. M. Do anesthesia information systems increase malpractice
exposure? Results of a survey. Anesth Analg 99, 840-3, table of contents (2004).
AIMS and Risk/Liability
• University of Miami case
• 58 y/o patient underwent craniotomy and suffers postoperative quadriplegia.
• Automated record keeping (PICIS (v 6.3))
• During the case, CRNA provided break, returned the
AIMS to vitals signs screen, and noticed that device
data were not being recorded.
• Although IT/engineering fixed problem, missing data
were not entered into the chart (and anesthesia
attending was not notified).
1. Vigoda, M. M. & Lubarsky, D. A. Failure to
recognize loss of incoming data in an anesthesia
record-keeping system may have increased medical
liability. Anesth Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case1
• Claim filed
• Investigation: 93 minutes of missing data, likely due
to disconnected cable
• Problems with anesthesia documentation contributed
to decision to settle case
1. Vigoda, M. M. & Lubarsky, D. A. Failure to recognize loss of incoming
data in an anesthesia record-keeping system may have increased medical
liability. Anesth Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case1
– Issue 1: Lack of awareness of incomplete record
• Missing data that possibly could refute
claim (or support it)
• Challenged legitimacy of other items in
record
– Required to have every five minute charting
1. Vigoda, M. M. & Lubarsky, D. A. Failure to recognize loss of incoming
data in an anesthesia record-keeping system may have increased
medical liability. Anesth Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case1
– Issue 1: Lack of awareness of incomplete record
• Medication window could cover the vital
signs display
– Added an alert for missing data stream(s)
– Post-case review of chart data integrity
• Natural anesthesiologist’s scan did not
include AIMS screen
– Re-mounted AIMS display on left side of anesthesia
machine, near vitals signs monitor
1. Vigoda, M. M. & Lubarsky, D. A. Failure to recognize
loss of incoming data in an anesthesia record-keeping
system may have increased medical liability. Anesth
Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case1
– Issue 1: Lack of awareness of incomplete record
D E S I G N
M AT T E R S
• Medication window could cover the vital
signs display
– Added an alert for missing data stream(s)
– Post-case review of chart data integrity
• Natural anesthesiologist’s scan did not
include AIMS screen
– Re-mounted AIMS display on left side of anesthesia
machine, near vitals signs monitor
1. Vigoda, M. M. & Lubarsky, D. A. Failure to recognize
loss of incoming data in an anesthesia record-keeping
system may have increased medical liability. Anesth
Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case1
– Issue 2: Timing of Chart Entries
• Lack of concordance of blood pressure
changes and notation of re-zeroing of art
line at ear
• “Pre-attestation” of presence at
extubation by attending
– Audit trail subpoenaed
1. Vigoda, M. M. & Lubarsky, D. A. Failure to recognize
loss of incoming data in an anesthesia record-keeping
system may have increased medical liability. Anesth
Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case1
– Issue 2: Timing of Chart Entries
• Challenged practice: charting
immediately with option to edit
– Now documentation at end with option to change time,
but never future charting
1. Vigoda, M. M. & Lubarsky, D. A. Failure to recognize
loss of incoming data in an anesthesia record-keeping
system may have increased medical liability. Anesth
Analg 102, 1798-1802 (2006).
AIMS and Risk/Liability
• University of Miami case Follow-up effort1
– Present at emergence attestation
– Automated feedback to discourage pre-attestation
1.
Vigoda, M. M. & Lubarsky, D. A. The medicolegal
importance of enhancing timeliness of
documentation when using an anesthesia
information system and the response to automated
feedback in an academic practice. Anesth Analg
103, 131-6, table of contents (2006).
AIMS and Risk/Liability
• Automated information management system
produced paper record with 15 minute
resolution
• During case, there was drop in EtCO2
associated with significant blood loss, but this
was only apparent at resolution of 1 minute, not
on printed summary.
• Which is “official medical record?”
1. Green, J. A., Arancibia, C. U. & Colquhoun, A.
D. Failure to display a significant change in etCO2
on printed automated anesthesia record: case
report and medicolegal implications. Society for
Technology in Anesthesia (2007).
AIMS and Risk/Liability
• Review of evidence as related to anesthetic
records1
– E-discovery
– Computer forensics
– Audit Trails
1. Szalados, J. E. The legal implications of anesthesia record
shortcomings. Anesthesiology News 33, (2007).
AIMS and Risk/Liability
• Discussion of U. of Miami Case1
– If anesthesiologist signed off on case, then there may
have been a reasonable duty to review the record
(since reviewing a record in PICIS is not
burdensome)
– Spoliation – intentional destruction, alteration, or
hiding of evidence
• May sometimes be presumed that party
that lost the evidence did so intentionally
to prevent harm to their side.
1. Szalados, J. E. The legal implications of anesthesia record
shortcomings. Anesthesiology News 33, (2007).
AIMS and Risk/Liability
• Discussion of U. of Miami Case1
– Recommendations
“medical records are expected to be
accurate, legible and complete; the signing
physician is expected to authenticate the
record and vouch for its truthfulness; and
the use of [an AIMS] does not necessarily
absolve the signing physician of liability.”
1. Szalados, J. E. The legal implications of anesthesia record
shortcomings. Anesthesiology News 33, (2007).
AIMS and Risk/Liability
• Discussion of STA abstract case1,2
– Official anesthetic record
• Original data – where originally stored
• Copies and Printouts – secondary data
– If addendum, may cast doubt on record if multiple
versions of records exist
– Court may require original data
1. Green, J. A., Arancibia, C. U. & Colquhoun, A. D. Failure to display a significant
change in etCO2 on printed automated anesthesia record: case report and
medicolegal implications. Society for Technology in Anesthesia (2007). {cited in
#2}
2. Szalados, J. E. The legal implications of anesthesia record shortcomings.
Anesthesiology News 33, (2007).
AIMS and Risk/Liability
Reviewer’s advice re: STA Case1,2 [emphasis added]
1.“the official record is the data collected by the computer;
the printed record is a legally acceptable summary that
remains suspect pending analysis of the full electronic
record”
2.The AIMS database contains the original data – it may have
components that are not on the summary record, but they are
still discoverable. Know what’s there
3.Corrections, deletions, addenda, etc. leave a digital trail that
may undermine the credibility of your record
1. Green, J. A., Arancibia, C. U. & Colquhoun, A. D. Failure to display a significant
change in etCO2 on printed automated anesthesia record: case report and
medicolegal implications. Society for Technology in Anesthesia (2007). {cited in
#2}
2. Szalados, J. E. The legal implications of anesthesia record shortcomings.
Anesthesiology News 33, (2007).
In Closing…
1. Design Matters – ensure
missing data are obvious and can be corrected easily
2.Workload Matters – ensure
amount of time needed to “feed” the system is at least less than time
system saves clinicians
(see #1)
3.A Major Benefit of an AIMS is using the information it generates
to improve systems of care – ensure
compliance groups have access to AIMS data
“You can never have enough report writers!”
4.To use the system appropriately, providers must have adequate
training, including a thorough understanding of the digital trail
they leave behind.