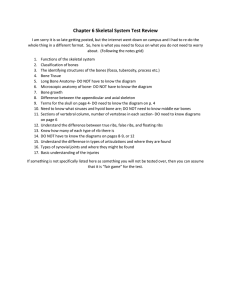
The Skeletal System
advertisement

The Skeletal System Three Types of Skeletons • Three Types of Skeletons • 1. Hydrostatic (water) 2. Exoskeleton (arthropods) 3. Endoskeleton (vertebrates) • The Skeleton of Humans is composed of a special connective tissue called BONE • There are 206 bones in the human body THE HUMAN SKELETON HAS TWO DIVISIONS • THE AXIAL SKELETON - CONSIST OF THE SKULL, VERTEBRATE COLUMN, AND THE RIB CAGE – The Skull consists of 8 CRANIAL BONES and 13 FACIAL BONES – The Ears consists 6 BONES – FLOATING IN THE THROAT 1 BONE THE HYOID – Ribcage - 12 pairs of ribs – Sternum (breastbone) – The Vertebral Column (Spinal Column or Backbone) 7 CERVICAL (NECK) VERTEBRAE, 12 THORACIC 5 LUMBAR, 5 FUSED VERTEBRAE INTO 1 SACRUM, 4 TO 5 SMALL FUSED VERTEBRAE INTO 1 COCCYX (YOUR TAIL BONE) • THE APPENDICULAR SKELETON - CONSIST OF THE BONES OF THE ARMS AND LEGS, SHOULDER, AND THE PELVIC GIRDLE. – THE PECTORAL GIRDLE CONSISTS OF 4 BONES, AND UPPER LIMBS CONSISTS OF 60 BONES (the hands and wrist contain 54 separate bones). – THE PELVIC GIRDLE CONSISTS OF 2 BONES AND THE LOWER LIMB CONSISTS OF 60 BONES (the ankles and feet contain 54 separate bones) Types of Skeletal Cartilages Skeletal Cartilage: – – – – Made of variety of cartilage tissue, consists primarily of water Has resilience: the ability to spring back to original shape Contains no nerves or blood vessels, surrounded by perichondrium that acts as a girdle Three Basic types of Cartilage • • • Hyaline Cartilage Elastic Cartilage Fibrocartilages Hyaline Cartilage • The cells, chondrocytes, appear spherical and are made of collagen fibers • Provide support and flexibility (resilience) • Most abundant type – – – – – Articular cartilage (cover end of bone) Costal cartilage (connect rib to sternum) Laryngeal cartilage (voicebox) Tracheal and Bronchial cartilage (reinforce respiratory system) Nasal (support the external nose) Elastic Cartilage • Looks very much like hyaline cartilage • Contains more elastic fibers, stands up to repeated bending • Only found in 2 places – The external ear – The epiglottis (flap that covers the larynx when swallowing) Fibrocartilage • Chondrocytes allign in parallel rows with thick collagen fibers • High tensile strength (bend ability without breaking) • In sites of heavy pressure and stretch – Knee – Vertebral disks Growth of Cartilage • Appositional Growth – “growth from outside” – The perichondrium secrete new matrix against the surface, expanding the tissue • Interstitial Growth – “growth from within” – Chondrocytes inside cartilage divide and secrete matrix, expanding tissue Functions of Bones • • • • • Support and Structure Protection of Vital Organs Movement—attachment site for muscles Mineral Storage: inorganic salts Blood Cell Formation (hematopoiesis): contains red marrow and produces red blood cells (erythrocytes) and some White Blood Cells (Leukocytes) Classification of Bones • Long Bones – Longer than wide – Consists of shaft and two ends – Constructed of primarily of compact bone, but may contain spongy (cancellous) bone – Examples: humerus, femur • Short Bones – Roughly cubelike – Made mostly of spongy (cancellous) bone – Examples: carpals and tarsals, sesamoid (patella) Classification of Bones • Flat Bones – Thin, flattened, and usually curved – Two layers of compact bone with a spongy (cancellous) layer in between – Examples: sternum, ribs, skull bones • Irregular Bones – Bones that do not fit the preceding classifications are placed in this category – Examples: vertebrae, and pelvic bones Chemical Composition of Bone • Organic Components – Cells: osteoblasts, osteoclasts, and osteocytes • Osteoblasts: bone forming cells • Osteoclasts: large cells that resorb or break down bone matrix • Osteocytes: mature bone cell – Osteoid: • Makes up 1/3 of the matrix, includes proteoglycans, glycoproteins, and collagen fibers • Contribute to a bone’s structure and are responsible for flexibility and tensile strength Chemical Composition of Bone • Inorganic Components – Make up 65% by mass – Hydroxyapatites (mineral salts) • Largely calcium phosphates • Allow for exceptional hardness ½ as strong as steel in resisting compression, and strong as steel in resisting tension--stretching • Allow bones to persist after death Osteogenesis • Intramembranous Ossification – – – – Defn.: when bone forms from fibrous membrane Most of the bones in skull and clavicles are examples Usually flat bones Mesenchymal cells form the initial structure and ossification begins at about the 8th week of development – The four steps in formation • • • • Ossification center of fibrous membrane forms Formation of bone matrix w/in fibrous membrane Formation of woven bone and periosteum Formation of compact bone plates and red marrow Osteogenesis • Endochondral ossification – – – – Defn.: bone formed by replacing hyaline cartilage structures Process begins late in second month of development More complex than intramembranous ossification Steps of ossification: • A bone collar forms around the diaphysis (shaft) of the hyaline cartilage model • Cartilage in the center of diaphysis calcifies • The periosteal bud invades the internal cavities and spongy bone forms • The medullary (marrow) cavity forms • The epiphysis (bone ends) ossify • See pg 174 Postnatal Bone Growth • Grows appositionally, usually stops in late adolescence or early adulthood • Some facial bones continue to grow throughout life—Nose and Lower jaw Growth of Long Bones • Mimics endochondral ossification – Cartilage on epiphyseal plate form tall column, ones on top divide quickly, pushing epiphysis away from diaphysis—entire bone lengthens – Older chondrocytes closer to shaft enlarge, and the surrounding cartilage matrix calcifies. The chondrocytes die, leaving spicules of calcified cartilage at the epiphysis-diaphysis junction. Cartilage spicules are covered with bone matrix by osteoblasts, forms spongy bone. Spongy bone is digested by osteoclasts, thus medullary cavity grows longer as well. Growth in Width • Done by process of appositional growth – Osteoblasts beneath periosteum secrete bone matrix on externl bone surface, osteoclasts on te endosteal surface of the diaphysis remove bone. – There is slightly less breakdown than building, thus produces thicker and stronger bone Hormones and Bone Growth • During infancy and childhood controlled by the growth hormone produced by pituitary gland • Thyroid produces T3 and T4 to ensure proper proportions • At puberty, testosterone and estrogen cause growth spurt, masculinization or feminization of specific parts of skeleton • Testosterone and estrogen causes the closure of the epiphyseal plate and end the longitudinal growth---stop increasing in height Bone Homeostasis • Bone Remodeling – Consists of bone deposit and bone resorption (removal) – In healthy adults total bone mass remains constant – BONE DEPOSIT • Occurs when bone is injured or additional bone strength is needed • Need diet rich in proteins, vitamin C (collagen synthesis), Vitamin A, B12, and minerals ( Ca, P, Mg, Mn, etc.) • New deposit has osteoid seam surrounding a calcification front • Requires the enzyme alkaline phosphatase for mineralization Bone Homeostasis – BONE RESORPTION • Must eliminate old bone matrix and release minerals as needed • Accomplished by osteoclasts – Osteoclasts secrete lysosomal enzymes that digest organic matrix and metabolic acids that convert calcium salts into soluble forms – The dissolved mineral salts are sent into the interstitial fluid and then the blood Hormonal Mechanism that Controls Remodeling of Bone • Occurs due to interaction of parathyroid hormone (PTH—produced by parathyroid glands) and calcitonin (produced by the thyroid gland) – When ionic Ca level drops in blood, PTH released to stimulate osteoclasts to resorb bone – Calcitonin is released when Ca levels in blood rise, stops resorption of bone and increases deposition of calcium salt in bone – HOMEOSTASIS ##Ca needed for nerve impulse transmission, muscle contractions, blood coagulation (clotting), gland and nerve cell secretions, and cell division **Hypercalcemia (disease of high blood Ca) leads to deposits of calcium salt deposit in blood vessels, kidneys and soft organs, hampering functionability Mechanical Stress and Remodeling of Bone • Caused by Muscle Pull and Gravity – Wolff’s Law: Bone grows or remodels in response to the forces or demands placed on it • Supported by weightlifters—have enormous thickenings in bone at muscle attachment sites • Supported by ballet dancers—have thickened bones in feet • Supported by anthropologic studies of human remains and class system • Explains atrophy in bedridden individuals and fetuses Differences in Males and Females • Females are shorter – During puberty, estrogen seals the epiphyseal plates sooner than testosterone in males • Males have larger arm and leg bones • Females have wider pelvic inlet and outlet Fractures of Bone • Simple (closed fracture): bone breaks cleanly, doesn’t penetrate skin • Compound: broken bone protrude through soft tissues and skin— often lead to osteomyelitis • Comminuted: bone fragments into many pieces (most common in elderly) • Compression: bone is crushed—common in osteoporotic bones • Depressed: broken bone portion is pressed inward—typical of skull • Impacted: broken bone ends are forced into each other—hip fractures • Spiral: ragged break caused by twisting forces applied to bone— sport fractures • Greenstick: bone break incompletely—most common in children Healing a Fracture • Hematoma forms – A mass of clotted blood forms at the fracture site – Bone cells are deprived of nutrition and die, area becomes swollen, painful, and obviously inflammed • Fibrocartilagionous callus forms – Capillaries grow in hematoma and phagocytic cells clean up debris – Fibroblasts and osteoblasts migrate to fracture site and begin reconstructing bone – Fibroblasts release collagen fibers that connect bone ends and will also secrete cartilage matrix – Osteoblasts begin formation of spongy bone that will eventually harden – “Splints the bone” Healing A Fracture Continued • Bony Callus Forms – Osteoblasts and osteoclasts migrate inward and multiply rapidly in the fibrocartilaginous callus. This will be converted to the bony callus of spongy bone – Occurs 3-4 weeks after injury and continues up to 2-3 months later • Remodeling – During bony callus formation and continuing for several months, bony callus remodeled – Excess building material on shaft of bone and within the meduliary cavity removed and compact bone reconstructed Disease of Bone • Osteoporosis – A group of diseases in which bone resorption outpaces deposit – Composition of bone remains same, mass reduced—bones become porous and lighter – Occurs most frequently in postmenopausal women, but cessation of sex hormone synthesis can cause disorder on both sexes – Other causes: insufficient exercise, calcium and protein poor diet, abnormal vitamin D receptors, smoking, and hormone related conditions – Treatments—Is preventable • • • • Calcium and vitamin D increase in diet Weight bearing exercise Hormone replacement therapy Drinking fluorinated water Bone disease continued • Osteomalacia – “Soft Bones” – Includes a number of disorders that cause bones to inadequately mineralize – Weight bearing bones fracture, bend, and deform – Symptom: pain when weight is put on affected bone – Cause: insufficient calcium in diet and Vit D deficiency • Rickets – Analogous disease in children – Causes bowed legs, deformities of pelvis, skull, and ribcage – Epiphyseal plates can’t be calcified so they continue to widen and ends of long bones are enlarged – Cause: insufficient calcium in diet or Vit D deficiency Bone Disease Continued • Paget’s Disease – – – – – Excessive bone breakdown and abnormal bone formation Can occur anywhere, most common in spine, pelvis, femur, and skull Rarely seen before age 40 Cause unknown—maybe virus? Treatment: drug therapy • Osteomyelitis – Inflammation of bone caused by puss forming bacteria – Commonly affects long bone – Acute pain, fever, joint stiffness, bone destruction, shortening of limb common symptoms – Treatment: antibiotic therapy, drainage of abscesses, removal of bone fragments Bone Diseases Continued • Osteosarcoma – – – – – – – Form of Bone cancer Typically in long bones of limbs and most often in 10-25 age group Grows aggressively Painful eroding of bone Metastasizes (moves to) lungs Treatment: amputation of affected bone or limb, chemotherapy Survival rate of 50% (if caught early) Paget’s Disease Rickets osteomyelitis osteosarcoma Osteomalacia