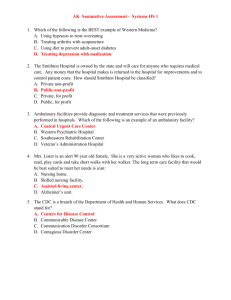
Guillain-Barré Syndrome, Myasthenia Gravis,The syndrome was
advertisement

Guillain-Barré Syndrome, Myasthenia Gravis, Dr. Abdul-Monim Batiha Guillain-Barré Syndrome • is an acute inflammatory demyelinating polyneuropathy (AIDP), a disorder affecting the peripheral nervous system. It is usually triggered by an acute infectious process. The syndrome was named after the French physicians Guillain, Barré and Strohl, who were the first to describe it in 1916. It is sometimes called Landry's paralysis, after the French physician who first described a variant of it in 1859. It is included in the wider group of peripheral neuropathies. ETIOLOGY • The etiology of Guillain-Barré syndrome is unclear, but an autoimmune response is strongly suspected. • There is a preceding event or trigger that is often an infection. • Occasionally, vaccinations have been known to trigger Guillain-Barré syndrome. • Approximately half of the people who develop Guillain- Barré syndrome have a mild febrile illness 2 to 3 weeks before the onset of symptoms. • The febrile infection is usually respiratory or gastrointestinal. • Approximately 25% of patients with this disease have antibodies to either cytomegalovirus or Epstein-Barr virus. PATHOPHYSIOLOGY • In Guillain-Barré syndrome, the myelin sheath surrounding the axon is lost. • Demyelination is a common response of neural tissue to many agents and conditions, including physical trauma, hypoxemia, toxic chemicals, vascular insufficiency, and immunological reactions. • Loss of the myelin sheath in Guillain-Barré syndrome makes nerve impulse transmission is aborted. CLINICAL MANIFESTATIONS • The syndrome may develop rapidly over the course of hours or days, or may take up to 3 to 4 weeks to develop. • Most patients demonstrate the greatest weakness in the first weeks of the disorder. • Patients are at their weakest point by the third week of the illness. • In the beginning, a flaccid, ascending paralysis develops quickly. • The patient is most commonly affected in a symmetrical pattern. • The patient may first notice weakness in the lower extremities that may quickly extend to include weakness and abnormal sensations in the arms. • Deep tendon reflexes are usually lost, even in the earliest stages. • The trunk and cranial nerves may become involved. • Respiratory muscles can become affected, resulting in respiratory compromise. CLINICAL MANIFESTATIONS • Autonomic disturbances such as urinary retention and orthostatic hypotension may also occur. • Superficial and deep tendon reflexes may be lost. • Some patients experience tenderness and pain on deep pressure or movement of some muscles. • Sensory symptoms of paresthesias, including numbness and tingling, may occur. • Pain is a complaint in a large number of patients. • It is aching in nature and often compared with the feeling of muscles that have been overexerted. CLINICAL MANIFESTATIONS • If there is cranial nerve involvement, cranial nerve VII, the facial nerve, is most often affected. • Guillain-Barré syndrome does not affect level of consciousness, pupillary function, or cerebral function. • Symptoms may progress for several weeks. The level of paralysis may stop at any point. • Motor function returns in a descending fashion. • Demyelination occurs rapidly, but the rate of remyelination is approximately 1 to 2 mm per day. DIAGNOSIS • The history of the onset of symptoms can be revealing because symptoms of Guillain-Barré syndrome usually begin with weakness or paresthesias of the lower extremities and ascend in a symmetrical pattern. • A lumbar puncture may be performed and reveal increased protein. • Also, nerve conduction studies record impulse transmission along the nerve fiber. • Pulmonary function tests are done when Guillain-Barré syndrome is suspected to establish a baseline for comparison as the disease progresses. • Declining pulmonary function capacity may indicate the need for mechanical ventilation and management in an ICU. CLINICAL MANAGEMENT • preventive measures need to be established to prevnt DVT and pulmonary embolism do not develop. • Heparin 5000 units subcutaneously may be given along with antiembolism stockings and sequential compression devices • The first therapy proven to benefit patients with Guillain-Barré syndrome is plasmapheresis. • This procedure mechanically removes humoral factors. • Intravenous immunoglobulin (IVIG) is also useful in managing Guillain-Barré syndrome. Myasthenia Gravis • Myasthenia gravis (from Greek "muscle", "weakness", and Latin gravis "serious"; abbreviated MG) is an autoimmune neuromuscular disease leading to fluctuating muscle weakness and fatigability. It is an autoimmune disorder, in which weakness is caused by circulating antibodies that block acetylcholine receptors at the post-synaptic neuromuscular junction, inhibiting the stimulative effect of the neurotransmitter acetylcholine. ETIOLOGY • Myasthenia gravis is an autoimmune disorder. • The factors that trigger the autoimmune process are not known, but the thymus gland is involved. • The thymus lies behind the sternum and may extend down to the diaphragm or up to the neck. • This gland plays a role in the responsiveness of T cells to foreign antigens. • The thymus gland is large in children and small in adults. • By adulthood, the gland has shrunken and has nearly been replaced by fat. • Abnormalities in the thymus gland frequently occur in patients with myasthenia gravis. • Eighty percent of patients with myasthenia gravis have thymal hyperplasia. PATHOPHYSIOLOGY • Myasthenia gravis is a result of circulating antibodies directed toward the skeletal muscle acetylcholine receptors. • This leads to a decrease in end plate depolarization, which may be insufficient to generate an action potential. • This results in a failure of the muscle to contract. CLINICAL MANIFESTATIONS • The hallmark of myasthenia gravis is fatigability. Muscles become progressively weaker during periods of activity and improve after periods of rest. Muscles that control eye and eyelid movement, facial expressions, chewing, talking, and swallowing are especially susceptible. • The muscles that control breathing and neck and limb movements can also be affected. • Symptoms, which vary in type and severity, may include asymmetrical ptosis (a drooping of one or both eyelids), diplopia (double vision) due to weakness of the muscles that control eye movements, an unstable or waddling gait, weakness in arms, hands, fingers, legs, and neck, a change in facial expression, dysphagia (difficulty in swallowing), shortness of breath and dysarthria (impaired speech). • In myasthenic crisis a paralysis of the respiratory muscles occurs, necessitating assisted ventilation to sustain life. In patients whose respiratory muscles are already weak, crises may be triggered by infection, fever, an adverse reaction to medication, or emotional stress. Since the heart muscle is only regulated by the autonomic nervous system, it is generally unaffected by MG. DIAGNOSIS • patient’s history • Patients may present with complaints of double vision or drooping eyelids. • Also, myasthenia gravis causes weakness of the shoulder girdle muscles. • The cranial nerve examination may reveal ptosis and diplopia • Motor weakness may be exhibited • Blood is drawn for acetylcholine receptor antibodies • Electromyography (EMG) CLINICAL MANAGEMENT • The clinical management of myasthenia gravis includes the following strategies: 1. use of medications to enhance neuromuscular transmission; such as anticholinesterases (Pyridostigmine (Mestinon), and steroids (Prednisone) • long-term immunosuppression with corticosteroids, azathioprine (Imuran), cyclophosphamide (Cytoxan), or cyclosporine; • short-term immunomodulation with plasmapheresis or IVIG; or thymectomy.