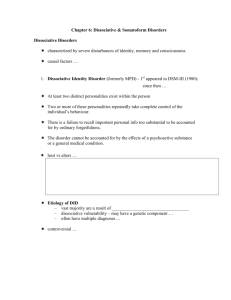
Mass Psychogenic Illness
advertisement

Somatoform Disorders Mass Psychogenic Illness Malingering & Factitious Disorders Dissociative Disorders Abnormal Psychology Chapter 8 Sep 22-29, 2009 Classes #9-11 Somatoform Disorders Physical symptoms with an absence of physical reasons for the symptoms No physical damage results from the disorder These individuals believe that their illnesses are real Psychosomatic Disorders Tension headaches, cardiovascular problems, etc. which cause physical damage State of mind appears to be causing the illness Somatoform Disorders Somatization Disorder (Briquet’s) Pain Disorder Hypochondriasis Body Dysmorphic Disorder Conversion Disorder Somatization Disorder Diagnostic Criteria To be diagnosed a person must have reported at least the following: Gastrointestinal symptoms (2) Sexual symptoms (1) Neurological symptoms (1) Pain (4 locations) These symptoms cannot be explained by a physical disorder Somatization Disorder Sex difference Onset F>M Primarily a female disorder with about 1% suffering from this disorder Usually by age 30 but its seen from childhood on up Familial tendencies 5 to 10 times more common in female first-degree relatives Genetic links to antisocial personality and alcoholism A typical scenario… Typically, patients are dramatic and emotional when recounting their symptoms They are often described as exhibitionistic and seductive and self-centered In an attempt to manipulate others, they may threaten or attempt suicide These patients “doctor-shop”… Often dissatisfied with their medical care, they go from one physician to another… What would be a recommended route for these patients to choose insofar a medical/mental health care is concerned??? They usually don’t go and further than their General Practitioner… Bottom line: Psychologists and psychiatrists rarely manage the majority of patients with somatoform disorders -- this difficult undertaking falls predominantly on general practitioners Somatization Disorder Explanations Psychodynamic Explanation Behavioral (Learning) Explanation Physiological (Biological) Explanation Cognitive Explanation Psychodynamic Explanation They have an unconscious conflict, wish, or need which is converted to a somatic symptom Pent-up emotional energy is converted to a physical symptom They may have identification with an important figure who suffered from the symptom They may have the need for punishment because of an unacceptable impulse directed against a loved one There may be an unconscious somatized plea for attention and care from these individuals Learning Explanation A child with an injury quickly learns the benefits of playing the sick role Reinforced by increased parental attention and avoidance of unpleasant responsibilities Physiological Explanation Genes Cognitive Explanation They do not accept doctors advice Therefore treatment is difficult Treatments Really haven’t been successful because patient usually won’t consider their problem as psychological In rare cases when individual is receptive to treatment, both psychoanalysis and cognitive treatments have brought improvement Drug treatments (anti-depressants and antianxiety meds) are often used to treat some of the residual symptoms but are not effective in helping with the somatization problems Complications There are several major complications to this disorder… Etiology Unknown We know it tends to run in families but the cause is unknown at this time More research is needed for this one Prognosis Poor Its usually a lifelong disorder Complete relief of symptoms for any extended period is rare Pain Disorder The patient complains of pain without an identifiable physical cause to explain the symptoms the person is complaining about Basically, the same as somatization disorder except that pain is the only symptom Body Dysmorphic Disorder Preoccupation with an imagined or minor defect in one's physical appearance It is distinguished from normal concerns about appearance because it is timeconsuming, causes significant distress, and impairs functioning Depression, phobias, and OCD may accompany this disorder Sex difference: Females > Males Females: breasts, legs Males: genitals, height, and body hair Symptoms Major concerns involving especially the face or head but may involve any body part and often shifts from one to another Examples: hair thinning, acne, wrinkles, scars, eyes, mouth, breasts, buttocks, etc. “Elise” from First Wives Club Treatments Cognitive-Behavioral Exposure is used to treat phobia-like symptoms Therapy will focus on improving the distorted body image that these people possess Treatments Physiological Preliminary evidence that selective serotonin reuptake inhibitors may be helpful but data on drug treatment is limited Treatments Family behavioral treatments can be useful Support groups if available can also help Prognosis Poor Since these individuals are reluctant to reveal their symptoms, it usually goes unnoticed for years Very difficult to treat as they usually insist on a physical cause More research is needed to determine any effective treatment for this disorder Hypochondrasis Unrealistic belief that a minor symptom reflects a serious disease Excessive anxiety about one or two symptoms Examination and reassurance by a physician does not relieve the concerns of the patient They believe the doctor has missed the real reason Hypochondrasis Symptoms adversely affect social and occupational functioning Diagnosis is suggested by the history and examination and confirmed if symptoms persist for at least 6 months and cannot be attributed to another psychiatric disorder (such as depression) Hypochondrasis Gender difference More common in women than men (I couldn’t find any stats though) Onset Usually in 30’s But seen in all age groups Treatments Much research suggests a cognitive-behavioral combo is best with therapist extremely gentle in his/her questioning the patient’s incorrect beliefs Prognosis Its not good (perhaps 5% recover) for the following reasons: Major Differences between Somatization Disorder and Hypochondrasis Focus of Complaint Style of Complaint Interaction with Clinician Age Physical Appearance Personality Style Conversion Disorder Sensory/motor dysfunction in the absence of a physical basis… Symptoms develop unconsciously and are limited to those that suggest a neurological disorder Examples: numbness of limbs, paralysis, speech problems, blindness and hearing loss, difficulty swallowing, sensation of a lump in your throat, difficulty speaking, difficulty walking, etc. Symptoms are not feigned (as in factitious disorder or malingering) Individual is often highly dramatic Conversion Disorder History Was first studied by the Nancy School of Hypnosis (Nancy, France) and Freud in examinations of hysteria (1880’s) Onset Tends to be adolescence to adulthood but may occur at any age Sex Difference Appears to be "somewhat" more common in women No stats Prevalence 1% - 3% of general population Tends to occur in less educated, lower socioeconomic groups Conversion Disorder: Important Characteristics Glove anesthesia Conversion Disorder: Important Characteristics Doctor Shop They visit many physicians hoping to find one who will propose a physical treatment for their non-physical problems La Belle Indifference The tendency of these people to be relatively unconcerned about their physical problem Explanations Pure speculation at this point Treatment Hypnotherapy Narcoanalysis The patient is hypnotized and potentially etiologic psychological issues are identified and examined Similar to hypnotherapy except the patient is also given a sedative to induce a state of semi-sleep Relaxation training Often combined with cognitive therapy Prognosis No treatment is considered very effective Mass Psychogenic Illness Also referred to as Mass Hysteria Epidemic of a particular manifestation of a somatoform disorder Mass Psychogenic Illness Sex difference: F > M Age Difference: Adolescents and children seem to be particularly at risk Mass Psychogenic Illness Physicians might consider a group sickness as being caused by mass psychogenic illness if: Physical exams and tests are normal Doctors can't find anything wrong with the group's classroom or office (for example, some kind of poison in the air) Many people get sick Mass Psychogenic Illness Symptoms Include the following: headache, dizziness, nausea, cramps, coughing, fatigue, drowsiness, sore or burning throat, diarrhea, rash, itching, trouble with vision, anxiety, loss of consciousness, etc. Treatment Removing patients from the place where the illness started Separate patients Understand that the illness is real Reassure patients that they will be okay Complications Do you see any complications here??? Are somatoform disorders real or faked? Malingering Factitious Disorders Munchausen Syndrome Munchausen Syndrome by Proxy Malingering Faking physical illnesses to avoid responsibility or for economic gain Seek medical care or hospitalization under false pretenses Once they get what they want they usually stop all complaining about their alleged problems Factitious Disorders Here, a person is faking symptoms to receive the attention and/or sympathy that comes with being sick… Munchausen Syndrome Munchausen Syndrome by Proxy Munchausen Syndrome (Factitious Disorder By Proxy) Condition characterized by the feigning of the symptoms of the disease in order to undergo diagnostic tests, hospitalization, or medical or surgical treatment These people (almost always women) fake serious symptoms in someone close to them (usually a child) to gain attention and sympathy ( a form of child abuse) Munchausen Syndrome by Proxy Signs and tests Munchausen Syndrome by Proxy Treatment Offer parent help rather than accuse them Psychiatric counseling will likely be recommended Family therapy is often helpful if the husband is willing Prognosis This is often a difficult disorder to treat and often requires years of psychiatric support Dissociative Disorders Dissociative Amnesia Dissociative Fugue Depersonalization Disorder Dissociative Identity Disorder Dissociative Amnesia Formerly termed Psychogenic Amnesia. Name of illness also changed in DSM IV The sudden inability to remember important personal information or events Usually begins as a response to intolerable psychological stress Very rare (less than 1%) Types of Dissociative Amnesia Localized amnesia The person fails to recall events that occurred during a particular period of time Selective amnesia The person can recall some but not all of the events during a certain time frame Generalized amnesia This lasts throughout a person’s entire life – very rare Continuous amnesia The inability to recall events subsequent to a specific time including the present Systemized amnesia The loss of memory for certain categories of information Dissociative Amnesia Treatment Therapy can be useful to help with coping but is not always needed Often, they become disoriented and may forget who they are but usually the amnesia vanishes as abruptly as it began Dissociative Fugue Formerly termed Psychogenic Fugue Name of illness also changed in DSM IV An episode during which an individual leaves his usual surroundings unexpectedly and forgets essential details about himself and his lives It is very rare, with a prevalence rate of about 0.2% in the general population Symptoms Sudden and unplanned travel away from home together with an inability to recall past events about one's life Cause Is usually triggered by traumatic and stressful events, such as wartime battle, abuse, rape, accidents, natural disasters, and extreme violence, although fugue states may not occur immediately Treatment Psychoanalysis Cognitive therapy ("creative therapies") Hypnotherapy Medications Family therapy Depersonalization Disorder These individuals report feeling detached from their mental processes or body Occurs in as many as 30% of normal individuals at some time Only constitutes a disorder if it interferes with a person’s functioning Cause As with other disorders in this category, an acute stressor is often the precursor to onset Symptoms This disorder is characterized by feelings of unreality, that your body does not belong to you, or that you are constantly in a dreamlike state Symptoms are most common between 25-44 Treatment The disorder will typically dissipate on its own after a period of time Therapy can be helpful to strengthen coping skills Prognosis Prognosis is very good Dissociative Identity Disorder Commonly referred to as Multiple Personality Disorder Very rare: Less than 1%. A person alternates between two or more distinct personality systems Usually there is a main or basic personality Sex difference: F > M (9 to 1 ratio) Symptoms The individual may change from one personality to another in a matter of a few minutes to several years (shorter time frames are more common) The personalities are often dramatically different Complications Sleep disorders Night terrors and/or sleep walking Alcohol and drug abuse OCD-like rituals Eating disorders Depression High suicide rate Probably the #1 “Hollywood Disorder” Important Note Until 1970's extremely rare with few reported cases (about 100) but since then its prevalence has increased dramatically. Why this dramatic increase??? Dissociative Identity Disorder Treatment Psychoanalysis -- try to give therapy to the main personality who "knows" the others Prognosis Not good