Trauma ITE Review - Emergency Medicine
advertisement

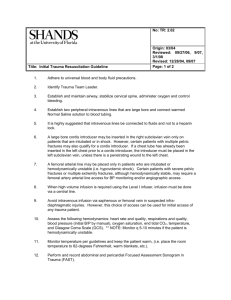
Trauma ITE Review Michelle Slezak Henry Ford Hospital Department of Emergency Medicine Basic Principles of Trauma Three peaks for trauma deaths • First (immediate death) • Massive head injury, high C-spine injury, cardiac laceration, aortic rupture, laceration of other great vessels, airway obstruction • Second (minutes to few hours) “Golden hour” • Subdural/epidural hematoma, ruptured spleen, lacerated liver, multiple injuries with hypovolemic shock, fracture of pelvis or multiple long bones, hemopneumothorax, tension pneumothorax, cardiac tamponade, massive hemothorax, aortic dissection/rupture • Third (days to weeks) • Multisystem organ failure, systemic inflammatory response syndrome Primary Survey (ABCDE) • Airway (and C-spine) • • • • If patient can speak, airway is intact Noisy respirations– partial obstruction Gag reflex depressed/absent or secretions pooling– airway poorly protected Intubate with collar loosened and inline precautions; collar restricts mouth opening to 20 mm or less • Breathing • Rate, depth, pattern of respiration; supplemental O2, pulse ox • Tension pneumo– needle thoracostomy followed by tube • Sucking chest wound– sterile occlusive dressing taped on three sides Primary Survey (ABCDE) • Circulation and hemorrhage control • • • • • • Pulse quality, rate, regularity; skin color, capillary refill, LOC Large bore IVs, warmed crystalloid, cardiac monitor Direct pressure for external bleeding Wrap unstable pelvic fractures with sheet Pericardiocentesis for tamponade ED thoracotomy Primary Survey (ABCDE) • Disability • Pupil size, reactivity, symmetry • Level of consciousness • AVPU (qualitative)– Alert, responds to vocal stimuli, responds to painful stimuli, unresponsive • GCS (quantitative)– eye opening, verbal response, motor response • Intubate for GCS <=8 • Exposure • Undress, warm blankets Hemorrhagic Shock Head Injuries Head injury • Leading cause of death and disability in trauma patients • Assume cervical spine injury exists • Suspect in intoxicated, headache, sensory changes, LOC, persistent amnesia, skull fx, lateralized weakness, abnormal pupillary function • Classification based on GCS • Mild (14-15) • Moderate (9-13) • Severe (3-8) Head injury • Concussion • Brief loss of neurologic function, headache, +/- vomiting, amnesia, no focal findings • CT negative • Post-concussive syndrome • Headache, irritability, dizziness, depression, loss of memory, inability to concentrate • Outpatient workup • Diffuse axonal injury • Prolonged coma, +/- posturing, +/autonomic dysfunction • No mass lesion on CT (may see punctate hemorrhages) • Mortality 33% Head injury • Cerebral contusion • Confusion, obtundation, coma, +/focal deficits • Visible on CT (frontal and temporal lobes) • Coup vs contrecoup • Delayed complications– cerebral edema, intracerebral hematoma • Skull fractures • • • • Linear, non-depressed– no tx Depressed– may be operative Open skull fx– operative “egg shell”– evaluate for child abuse Epidural hematoma • InjuryLOClucid interval (30%)coma (fixed, dilated ipsilateral pupil, contra hemiparesis) • Transtentorial herniation compresses CN III and corticospinal tract • Arterial bleed (middle meningeal artery) • Lens-like, biconvex lesion does not cross cranial sutures • Associated parietal or temporal fx (80%) • Mortality 0-20% Subdural hematoma • More common than epidural • Significant intrinsic brain damage • Mild headache, confusion, lethargy, coma • Bleeding from bridging veins • Pts with brain atrophy more susceptible • Crescent shaped lesion can extend beyond cranial sutures • Mortality for acute 30-60% Basilar skull fracture • Battle’s sign • Raccoon eyes • Hemotympanum • CSF rhinorrhea • “ring sign” • Can compress CN (esp VII) Increased intracranial pressure • Headache, N/V, decreasing LOC, progressive deficit, Cushing reflex (hypertension, bradycardia), sixth nerve paresis, papilledema, herniation • Most rapid mechanism for lowering ICP– hyperventilation (to 30-35 mm Hg) • Causes vasoconstriction of cerebral vasculature ENT Trauma ENT trauma • Auricular hematoma • Drain; compressive dressing to prevent “cauliflower ear” • Reassess in 24 hours • TM perforation • Penetrating object, loud noise, infection, lightning strike, rapid changes in pressure • Exam shows tear; immobility of TM on bulb insufflation • Tx– heal spontaneously, keep dry • Can have hearing loss, N/V, vertigo, facial palsy (suggests injury to ossicles, labyrinth, temporal bone) ENT trauma • Nasal bone fractures • Most common facial fx • Imaging not necessary • ENT for reduction once swelling improves • Gross angulation reduced in ED • Nasal septal hematoma • Bluish-purple, grapelike swelling of septum • Need vertical I&D to prevent “saddle nose” deformity due to avascular necrosis • Pack, anti-staph abx, ENT LeFort fractures • Usually occur in combination • Beware of cervical spine and airway • Diagnose by grasping upper alveolar ridge and note which part of the midface moves • Avoid NG tube LeFort fractures • I– horizontal fx of maxilla at level of nasal floor • Allows movement of alveolar ridge and hard palate • II– pyramidal fx with apex just above bridge of nose and extends laterally and inferiorly through infraorbital rims • Allows movement of maxilla, nose, infraorbital rims • III– complete craniofacial disruption • Involves zygoma, infraorbital rims, maxilla; dishpan face Mandible fracture • Second most common facial fracture • Ringlike structure– two or more fractures in 50% • Most common fracture sites– condyle, body, angle • Tenderness, deformity, sublingual hematoma, asymmetry, deviation TOWARD side of fx • Tongue blade test • Panorex (most useful), CT Mandible dislocation • Trauma, yawning, laughing • Bilateral– anterior open bite • Unilateral– jaw displaced AWAY from side of dislocation • Reduction– thumbs on posterior molars and push mandible downward and posterior Tripod fracture • Fracture of zygomatic arch, zygomaticofrontal suture, and infraorbital foramen • Also, lateral wall of maxillary sinus and orbital floor • Flattening of cheek, periorbital swelling, ecchymosis, diplopia, palpable step-off of inferior orbital rim, anesthesia of cheek/upper teeth/lip/gum Dental fractures • Ellis I– enamel fx; no pain, no hot/cold sensitivity; elective followup • Ellis II- enamel fx and dentin exposed; hot/cold sensitivity; followup within 24 hrs • Ellis III– enamel fx, both dentin and pulp exposed; pink dot; severe pain; immediate dental referral • Alveolar fracture– considered open fx; need antibiotics Avulsed teeth • Permanent tooth • • • • Rinse with saline and replace ASAP Do not brush; will remove periodontal ligament Viability decreased 1% for every minute out of socket Can also transport in Hank’s solution or milk • Primary tooth • 6 months to 5 years • Do not replace Ocular Trauma UV keratitis • Prolonged UV exposure– arc welding, reflected sunlight (snow blindness), artificial sunlight (tanning bed) • Symptoms 6-12 hours after exposure • Severe pain, photophobia, FB sensation, tearing, blepharospasm, decreased visual acuity • Multiple pinpoint epithelial surface irregularities on fluorescein staining • Treat with topical cycloplegic, ointment, oral pain meds • No topical anesthetic b/c increases risk of corneal ulceration Traumatic iritis • Symptoms 1-4 days post trauma • Tearing, photophobia, decreased visual acuity • Consensual photophobia, ciliary flush, miotic pupil, cells and flare • Treat with topical cycloplegic (paralyzes ciliary body, dilates pupil, prevents formation of posterior synechiae), topical steroid Orbital floor fracture (blow-out fracture) • Pain and diplopia on upward gaze (entrapment of inferior rectus and inferior oblique), enophthalmos, hypesthesia of infraorbital nerve, subcutaneous orbital emphysema • Best seen on Water’s view • Air-fluid level in maxillary sinus, “tear-drop” sign (prolapse of orbital tissue into maxillary antrum), clouding of maxillary sinus, orbital emphysema Medial orbital wall fracture • Epistaxis, emphysema of lids/conjunctiva, limited lateral gaze (entrapment of medial rectus) • Clouding of ethmoid sinus, orbital emphysema • Treatment of orbital fractures • Exclude associated ocular injuries (globe rupture) • Decongestants, antibiotics, avoid Valsalva, ophtho Ocular chemical burns • Alkali (liquefaction necrosis)-- worse • Acid (coagulation necrosis) • Immediate, copious irrigation until pH neutral • Topical cycloplegic, antibiotic ointment, oral analgesics, ophtho Lid lacerations • Superficial can be repaired with 6-0 or 7-0 nonabsorbable • Refer to ophtho • • • • • Lacrimal canaliculi Levator muscle/tendon (ptosis) Canthal tendons Orbital septum (fat protrusion) Lid margins Corneal abrasion • Pain, FB sensation, tearing, photophobia, conjunctival injection • Evert lids to look for FB • Treat with cycloplegic, topical antibiotic, oral analgesics • Avoid eye patch (esp if vegetable matter or contacts) Corneal rust ring • Can remove FB after topical anesthetic • Use 25 g needle • Refer for removal of rust ring the next day Globe perforation • Bell’s phenomenon– eyeball rolls upward and outward in response to eye closure • Perforations often located in inferior aspect of globe • Teardrop/irregular pupil, flattening of anterior chamber, black iris pigment at wound edges, decreased visual acuity • Seidel test– fluorescein stain flows from lac in “riverlike” pattern b/c aqueous humor leakage • DO NOT check IOP! • Metal eye shield, NPO, tetanus, IV abx, analgesics Hyphema • Bleeding into anterior chamber from blood vessels of ciliary body or iris • Eye pain, photophobia, blurred vision • Examine in sitting position so blood layers in anterior chamber • Keep HOB 45⁰, metal eye shield, avoid eye movement, no ASA or NSAIDs • B-blockers, alpha-agonists, carbonic anhydrase inhibitors (avoid in sickle cell) • Complications– rebleeding 2-5 days later, secondary glaucoma, corneal staining Retrobulbar hematoma • Extreme blunt or deep penetrating trauma • Proptosis, decreased vision, pain, limited mobility, increased IOP, afferent pupillary defect • Lateral canthotomy Neck Injuries Neck injuries • Most common cause of death is exsanguination • Vascular injury occurs in 25% of penetrating neck wounds (IJ, carotid) • Historically, all injuries that penetrate platysma explored surgically Zones of the neck • Zone I: base of neck to cricoid cartilage • Structures– subclavian vessels, brachiocephalic veins, common carotid arteries, aortic arch, jugular veins, trachea, esophagus, lung apices, cervical spine, spinal cord, cervical nerve roots • Angiography needed to determine integrity of thoracic outlet vessels • Positive angio may necessitate thoracotomy Zones of the neck • Zone II: cricoid cartilage to angle of mandible • Structures– carotid and vertebral arteries, jugular veins, pharynx, larynx, trachea, esophagus, cervical spine, spinal cord • Most common location for penetrating trauma • Easily accessible surgically • Some recommend CT angio or carotid duplex Zones of the neck • Zone III: angle of mandible to base of skull • Structures– salivary and parotid glands, esophagus, trachea, vertebral bodies, carotid arteries, jugular veins, major nerves (CN IX-XII) • Difficult to expos surgically • Angio to assess internal carotid and intracerebral circulation Spine Injuries Spine injuries • Spinal cord ends at L2 • Cross-table lateral must visualize all 7 cervical vertebrae and C7-T1 interspace • NEXUS criteria • • • • • No midline tenderness No focal neurologic deficit Normal alertness No intoxication No painful distracting injury Jefferson fracture • C1 ring blowout • Axial load injury • Seen on open-mouth odontoid view Odontoid fractures • Swelling anterior to C2 on lateral film • Abnormalities on open-mouth odontoid • Type I– tip of the dens • Type II– traverses dens at junction of body of C2 • Type III– involves vertebral body of C2 Cervical spine fractures • Hangman’s fracture • Bipeduncular fx of C2 • Extension injury • Clay shoveler’s fracture • Flexion avulsion fx of spinous process of C6-T3 (C7 most common) • Flexion injury • Direct blow to spinous process Vertebral injuries • Facet dislocation • Unilateral (flexion-rotation) • Bilateral (flexion) • Anterior displacement of superior vertebral body relative to adjoining inferior vertebral body • Flexion teardrop fracture • Significant disruption of posterior ligaments • Anterior cord syndrome Vertebral fractures • Chance fracture • Transverse fx through vertebral body from flexion about axis anterior to vertebral column • MVC when only lap belt worn • Associated with retroperitoneal and abdominal visceral injuries • Fracture-dislocations • Extreme flexion or severe blunt trauma • Disruption of posterior elements (pedicles, facets, laminae) • Often complete neuro deficit Spinal Cord Syndromes Anterior cord syndrome • Flexion injury • Loss of function of anterior 2/3 of cord • Complete loss of motor, pain, temperature below level • Preservation of posterior column functions of vibration and position Central cord syndrome • Hyperextension injury in patients with degenerative spurring or congenital narrowing • Weakness greater in arms than legs • Good prognosis Brown-Sequard syndrome • Penetrating injury hemisects cord • Ipsi motor paralysis, loss of proprioception and vibration • Contra loss of pain and temperature • Good prognosis Cauda equina syndrome • Injury to lumbar, sacral, coccygeal nerve roots causing peripheral nerve injury • Motor/sensory loss in lower extremities • Bladder dysfunction (most consistent) • Bowel dysfunction • Saddle anesthesia • Decreased rectal tone • Weakness in dorsiflexion of great toe Neurogenic shock • Loss of neurologic function and accompanying autonomic tone • Flaccid paralysis • Loss of reflexes • Loss of urinary and rectal tone • Bradycardia (may need atropine, pacemaker) • Hypotension (IVF, +/- dopamine or phenylephrine) • Hypothermia • Ileus SCIWORA • Spinal Cord Injury Without Radiographic Abnormalities • Kids more susceptible b/c greater elasticity of cervical structures • Brief episode of upper extremity weakness or paresthesias • Delayed development of neuro deficits • Must obtain MRI Thoracic Trauma Tension pneumothorax • Respiratory distress • Hypotension • Tachycardia • PEA • Tracheal deviation away • Absent breath sounds • Hyperresonance • Needle thoracostomy followed by tube thoracostomy Simple pneumothorax • Decreased breath sounds • Hyperresonance • Dyspnea • Diagnosed best on expiratory CXR • May observe up to 25% • Always chest tube if transport by air Flail chest • Contiguous rib fx in multiple places • Paradoxical movement of chest wall • Do not wrap chest Pulmonary contusion • Most common potentially lethal chest injury • Direct chest wall trauma • Dyspnea, tachypnea, tachycardia, chest wall tenderness/ecchymosis, rib fractures • CXR findings localized to site of injury • Usually present on arrival and always within 6 hours • Treat with O2, pulmonary hygiene, pain control • May need intubation and ventilation with good lung down • Pneumonia is most common complication Hemothorax • • • • • • • CXR requires 200-300 ml Blunting of costophrenic angle on upright Diminished breath sounds Dullness to percussion Decreased tactile fremitus Most need chest tube Thoracotomy • • • • • Blood loss >1500 initial drainage Persistent bleeding requiring continuous transfusion Hypotension or decompensation Blood loss >200 ml/hr for 2-4 hours 50% hemorrhage Myocardial contusion • High-speed deceleration • Heart (usually RV) strikes sternum • ECG neither sensitive or specific • Sinus tachycardia, multiple PVCs, atrial fib, bundle branch block (RBBB), ST-T wave changes • Echo • Impaired regional systolic function, increased enddiastolic wall thickness Traumatic myocardial infarction • Coronary artery occlusion by arterial spasm, intimal tear, thrombosis, compression from adjacent hemorrhage/edema • Pre-existing CAD at greatest risk • Thrombolytics contraindicated Pericardial tamponade • Penetrating trauma most common • Rapid deceleration of blood filled ventricles during early systole or late diastolerents/tears/lacs of rigid myocardial wallimpending myocardial rupture • 60-100 ml in pericardium • Beck’s triad– hypotension, JVD, muffled heart tones • Decreased pulse pressure, rising CVP, Kussmaul’s sign, pulsus paradoxus • Electrical alternans, PEA, pericardial fluid on US • Pericardiocentesis, open thoracotomy Traumatic aortic rupture • Sudden deceleration • Most occur at ligamentum arteriosum (point of greatest aortic fixation) just distal to left subclavian • Retrosternal pain • Dyspnea • Harsh systolic murmur • Upper extremity hypertension • Decreased/absent femoral pulses • Ischemic pain of extremities • paraplegia Traumatic aortic rupture findings • • • • • • • • • • Widening of superior mediastinum Obliterated/indistinct aortic knob (most reliable) Deviation of trachea and/or esophagus to right Depression of left mainstem bronchus >40⁰ below horizontal Obliteration of space between pulmonary artery and aorta Left apical pleural cap Multiple rib fractures Widening and/or displacement of paratracheal stripe to right Widening of left or right paraspinous stripe Fractures of first or second ribs or scapula Abdominal Trauma Abdominal trauma • Blunt trauma-- spleen most commonly injured organ; followed by liver • Penetrating trauma– liver most commonly injured organ; followed by small bowel • GSW– high incidence of peritoneal cavity penetration and intraperitoneal injury • Most require laparotomy • Stab wounds– low incidence of intraperitoneal injuries • Exploration, diagnostic laparoscopy • Most common location is LUQ • Solitary lap belt– jejunal injuries and mesenteric lacerations Ultrasound • Initial diagnostic modality for hemodynamically stable and unstable patients with blunt trauma • Advantages • • • • • Noninvasive Detects intraabdominal/pericardial/pleural fluid Rapid, safe, portable, doesn’t interfere with resuscitation No contrast Sensitive • Disadvantages • • • • Can miss bowel and retroperitoneal injuries Cannot differentiate fluids Impaired in obese Operator dependent Ultrasound • Unstable patient + positive US laparotomy • Stable patient + positive US CT • Unstable patient + negative US repeat US or DPL • Stable patient + negative US observation CT • Study of choice for hemodynamically stable patients with blunt trauma, GU trauma, suspected retroperitoneal injuries • Advantages • Noninvasive • Gives information on specific organ injury • Diagnoses retroperitoneal and pelvic injuries • Disadvantages • • • • Contrast More time than DPL Expert interpretation Can miss diaphragm, pancreas, bladder, bowel injuries • Normal VS + normal US CT can be deferred • Normal VS + positive US CT DPL • Identify intraabdominal bleeding or bowel injury that requires immediate laparotomy in unstable patient if FAST not available or inconclusive • Advantages • Rapid • Readily available • Sensitive • Disadvantages • Invasive • Misses retroperitoneal/diaphragm/isolated hollow viscus injuries • Less specific • Only contraindication to DPL is an existing indication for laparotomy Genitourinary Trauma Renal injury • Flank ecchymosis • Lateral abdominal tenderness/mass • Hematuria • Fracture of lower posterior ribs or lumbar vertebrae • Deceleration injury can cause pedicle injuryuncontrolled hemorrhage, renal ischemia, exsanguination • Diagnose with IVP, CT Urethral injury • Most common mechanism is straddle injury • Perineal pain • Inability to void • Gross hematuria • Blood at urethral meatus • Perineal swelling/ecchymosis • Absent/high-riding/boggy prostate • Diagnose with retrograde urethrogram • Do not place foley catheter! Bladder injury • Extraperitoneal • Full bladder poked by pelvic fx • Nonsurgical tx • Foley for 1-2 weeks • Intraperitoneal • Full bladder ruptures with urine spillage into peritoneum • Surgical tx • Diagnose with CT cystography, retrograde cystography Other GU injuries • Asymptomatic microscopic hematuria • Not good predictor of GU injury • Amount of blood does not correlate with severity of injury • Close follow-up and repeat UA • Penile fracture • Sudden tear in tunica albuginea with rupture of corpora cavernosum • Snapping noise and immediate detumescence • Testicular disruption • Fall or kick to scrotum • Swollen, ecchymotic scrotum • Absent testis Trauma in Pregnancy Trauma in pregnancy • Most common cause of non-obstetric maternal death during pregnancy • MVC, interpersonal violence, falls • Fetal survival depends on maternal survival • Management directed at resuscitation of mother • Review normal physiologic changes of pregnancy • Increased HR, decreased BP, increased plasma volume, physiologic anemia, increased wbc, hyperventilation, uterine flow comprises 20% cardiac output • LR better than NS for resuscitation Trauma in pregnancy • Position patients tilted to left to relieve compression of IVC from gravid uterus • >20 weeks should undergo continuous cardiotocographic monitoring • Chest tubes– never below 4th ICS • DPL– open, supraumbilical technique • Rhogam • Mini dose (50 mcg) if <12 weeks • Standard dose (300 mcg) if >12 weeks Trauma in pregnancy • Uterine rupture • Free intraperitoneal air • Extended fetal extremities • Abnormal fetal position • Placental abruption • • • • • • • • Vaginal bleeding Abdominal pain Uterine tenderness Expanding fundal height Maternal shock Fetal distress DIC Only 50% detected by US Perimortem C-section • Fetal prognosis improves with advanced gestational age • Maternal improvement may be from relief of aortocaval compression by fetus • Best if done within 5 minutes of maternal loss of vitals Miscellaneous Traumatic Conditions Compartment syndrome • Six Ps • • • • • • • • • • Pain out of proportion to injury (earliest) Paresthesias Paralysis Pallor Palpable tenseness/tenderness Pulselessness (latest) Most consistent exam finding– loss of two-point discrimination ∆P <30 is indication for fasciotomy (∆P=DBP-CP) Keep extremity level or slightly elevated Most commonly seen with tibial fractures Drowning • 10-15% are dry • No aspiration • Laryngospasm with closed glottis • Co-morbidities– hypothermia, hypotension, C-spine injuries • Death usually due to hypoxia • CXR normal, generalized pulmonary edema, perihilar pulmonary edema • Most common cause of dysrhythmia is hypoxia • Most reliable prognostic indicators– duration of submersion and resuscitation Electrical shock • Conduction system changes • Cardiac– asystole, Vfib (most common cause of death in acute phase) • CNS– respiratory, apnea, seizures (nerves have highest conductive capacity • Thermal tissue damage • Cutaneous burns and muscle injury • Muscle injuryrhabdomyolysisrenal failure • Blunt trauma • Shock can throw victim • Tetanic contractions– scapular fx, shoulder dislocations Electrical shock • • • • • Most common entrance sites are hand and skull Most common exit site is heel Cleanse, tetanus, check for compartment syndrome, don’t debride Beware of traumatic cataracts Hospitalize • High-voltage (>1000 V) burns • Low-voltage (<1000 V) burns with sx (dysrhythmias, chest pain, cutaneous findings, abnormal urine) • Discharge • Asx patients with low-voltage injuries after period of obs and cardiac monitoring • Extent of cutaneous injury in no way correlates with amount of underlying tissue damage Lip burns • Can have delayed bleeding from labial artery 3-14 days later when eschar separates Rhabdomyolysis • Muscle pain, weakness, tenderness, hypotension, AKI, shock • Elevated CPK • Hypocalcemia (63%) • Hyperkalemia (40%); get an EKG • Myoglobinuria (+blood but no rbc on microscopy) • Maintain urine output 1.5-2.0 ml/kg/hr • IVF, Lasix, mannitol, alkalinization of urine with sodium bicarbonate Thermal burns • Inhalation injury • • • • • • • • Facial burns Singed facial and nasal hair Oropharyngeal inflammation Carbon deposits in oropharynx Carbonaceous sputum Fire exposure in confined space Circumferential burns of neck Early intubation!! Thermal burns • Rule of Nines; Rule of Palms • Parkland formula • Fluid in 24 hours = 4 x weight (kg) x % BSA • First half in 8 hours; second half next 16 hours • Guide resuscitation based on urine output • Adults 0.5-1.0 ml/kg/hr • Kids 1-2 ml/kg/hr