Skin
advertisement

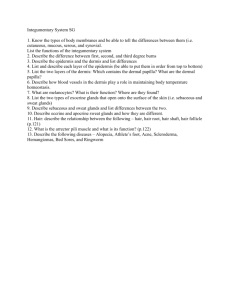
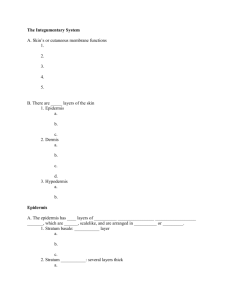
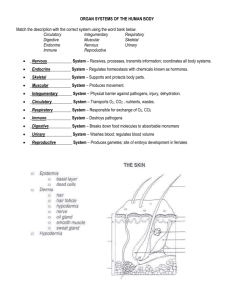
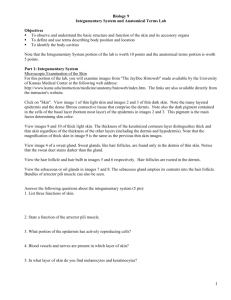
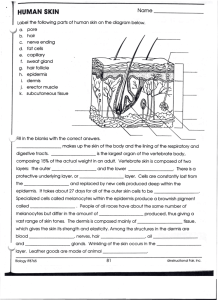
Membranes -many body structures and surfaces are covered with membranes -superficial sheet of epithelial cells + underlying connective layer -cover & protect -four types: 1. serous 2. mucous 3. cutaneous 4. synovial 1. Serous membranes -line the subdivisions of the abdominopelvic cavity and thoracic cavity -covers, protects and moistens/lubricates -comprised of an epithelial layer (simple squamous epithelium) called a mesothelium + underlying loose areolar connective tissue -the mesothelium secretes a watery fluid = serous fluid (separates and lubricates the movement of organs) -divided into two separate layers: 1)outer parietal layer - lines the cavity 2) inner visceral layer - covers organs -serous membrane lining the pleural cavity (lungs) = pleura - serous membrane lining the pericardial cavity (heart) = pericardium - serous membrane lining the peritoneal cavity (abdomen) = peritoneum 2. Mucous membranes -line cavities that directly communicate with the exterior environment e.g. respiratory, urinary, reproductive, digestive -covers, protects and moistens/lubricates -epithelial layer (simple squamous, simple cuboidal, simple columnar) is kept moist through production of mucus by glands, other glandular secretions or exposure to fluids (e.g. urine) -in areas of physical stress = stratified epithelial tissue rather than simple -connective tissue layer is loose areolar tissue = lamina propria --supports embedded blood vessels and nerves 3. Synovial membranes -extensive areas of areolar connective tissue covered by incomplete layers of simple squamous or cuboidal epithelial cells -lines & lubricates the synovial joint cavity - to permit easy movement of bones -the epithelium differs from others: 1) there is no basal lamina 2) incomplete cellular layer - gaps between cells 3) derived from macrophages and from the surrounding connective tissue -some cells within this membrane are phagocytic to remove pathogens -others are secretory - secrete a watery synovial fluid for lubrication 4. Cutaneous membrane (skin) -covers the surface of the body -epithelial layer (keratinized stratified squamous) -underlying areolar tissue reinforced with dense connective tissue Integumentary System (Skin) •skin covers the entire body surface -including the anterior surface of the eye! -covers ~ 22 square feet -about 16% of total body weight •skin turns in at the mouth, nasal cavity, anus and urethral and vaginal openings – meets the mucous membranes lining these cavities •comprised of all four tissues: 1. epithelium – lines the surface 2. connective – provides strength & resiliency 3. muscle – smooth muscle controls blood vessel diameter and controls movement of hairs 4. nervous – provides sensation and controls SM functions: 1. physical protection: protection from microbes, abrasion, heat 2. chemical protection – keratin - dryness of the epidermis; salt of sweat 3. regulation of water exchange: by sweating 4. regulation of body temperature: thermoregulation -by sweating & adjusting blood flow through the dermis 5. excretion of wastes -by sweating 6. nutrition – synthesis of vitamin D precursor -activated in skin, converted to calcitrol in liver 7. sensation: touch, pressure, vibration, pain & thermal 8. immune defense: Langerhans cells of the epidermis -two major components: 1. cutaneous membrane = skin (epidermis, dermis) 2. accessory structures = hair, nails, exocrine glands Epidermis -stratified squamous epithelium - 5 layers maximum -four types of cells: 1. keratinocytes – make up the majority of the epidermis -epithelial cells that synthesize the protein keratin 2. melanocytes – cells for the synthesis of the light absorbing pigment melanin 3. Merkel cells – neurons that detect pressure 4. Langerhans cells – immune responses Epidermis: layers - stratum germinativum: -inner most/deepest layer of the epidermis -also called stratum basale because it attaches firmly to the basal lamina or basement membrane found between the epithelium and connective tissues of the dermis - contain basal stem cells that differentiate into the keratinocytes and melanocytes of the epidermis -Merkel cells are found in hairless regions -pressure and touch receptors of the skin Epidermis: layers - stratum spinosum: -called the “spiny layer” because of histological appearance following chemical treatment -keratinocytes of the stratum basale migrate into this layer -several layers thick -keratinocyotes interconnected by bundles of protein filaments called tonofibrils – connect neighbouring keratinocytes together -act as cross braces providing strength -cells can divide - division of cells within this layer increases thickness -melanocytes are common -Langerhans cells also found – in the more superficial layers of this layer -initiate immune responses to pathogens and to cancer Epidermis: layers -stratum granulosum: -made up of keratinocytes migrating up from the stratum spinosum -cells synthesize large quantities of proteins (including keratin) – cytoplasm appears granular -the granules = keratohyalin granules -these granules surround the keratin filaments as they develop -as keratin is made – keratinocytes become thinner and flatter -the cells then die and dehydrate -creates layers of interlocking keratin “sandwiches” Epidermis: layers stratum lucidum: -covers the Str. Gran. -flattened, densely packed cells filled with keratin -have a glassy appearance because they do not stain well -present only in the skin of fingertips, palms & soles ONLY FOUND IN THE PALMS OF THE HAND SOLES OF THE FEET Epidermis: layers - stratum corneum: -cornu = horn -makes up surface of both thick and thin skin -15-30 layers of flattened, dead, interlocking cells -large amounts of keratin are present – the tissue is said to be “cornified” -covered in secretions from dermal glands to help moisturize the outer layer -but keratin makes this layer water-resistant - very dry – prevents growth of microorganisms -most of this layer is also hydrophobic -penetration is promoted by attachment to a lipid or dissolution in a lipid-based solution -transdermal drug patches – drugs are in oils or lipid-soluble carriers - moisturizing lotions – only penetrate few first layers of corneum -takes 15-30 days to move from germinativum to corneum -cells will remain in corneum for an additional 2 weeks before being shed Dermis -two major components: 1. papillary layer 2. reticular layer Papillary Layer -about 1/5th thickness of dermis -loose areolar connective tissue + elastic fibers -contains capillaries for blood supply & sensory nerve endings -dermal projections into the epidermis = papillae (papilla – “nipple-shaped mound) -some papillae contain Meissner’s corpuscles for touch -also free nerve endings – project into the epidermis - sensations of pain, warmth, itching Reticular Layer (“little net”) -dense irregular connective – interwoven collagen bundles plus elastic fibers -contains blood vessels, nerves, hair follicles, sweat glands and sebaceous/oil glands -also contains lamellated corpuscles (Pacinian corpuscles) that detect deep touch and pressure Fingerprints: epidermal ridges -formed from the stratum germinativum -extends down into the dermis -formed by the connections between dermal papillae and the epithelium -the contours of the skin follow these ridge patterns = fingerprints -function to increase the SA of the skin and increase friction Skin colour 1. dermal blood supply: - hemoglobin bound to O2 – bright red in color -gives pinkish cast to skin -when hemoglobin lacks O2 – bluish colour -this bluish skin colour = “cyanosis” -the thin skin of the lips and transparency of the nail enables us to see the blood in the peripheral circulation = red lips and pink nails -dermal blood supply comes from the larger blood vessels found in the subcutaneous layer (located under the dermis) -these larger vessels branch to form a cutaneous plexus (plexus = network) - this supplies the reticular layer - vessels continue up and branch further into the papillary plexus - found in the dermal papillae -blood is drained out of the papillae by tiny veins = venules -these drain into the larger veins of the dermis -> which then drain into the SQ layer Skin colour 2. pigmentation – two pigments: carotene and melanin -carotene = orange, yellow colour -derived from vitamin A -can be converted back to vitamin A in the skin - required for epithelial maintenance & the synthesis of visual pigment (rhodopsin) -carotene accumulates in keratinocytes -yellow color is very evident in the stratum corneum -melanin = dark brown, black colour -synthesized from the amino acid tyrosine -melanin absorbs UV light and prevents damage to the keratinocytes of skin -melanin production stimulated by UV light -produced by the melanocytes of the epithelium -forms in intracellular vesicles = melanosomes -melanosomes are secreted out of the cells = melanin is transferred into keratinocytes -Caucasians: transfer occurs to keratinocytes only in the Str. germ. and spinosum -Blacks: larger melanosomes -transfer also occurs in the Str. granulosum -darker pigmentation results -more active melanocytes – NOT more in number! Wrinkles: reduction in the thickness of the dermis -loss of collagen in the dermal reticular layer -loss in dermal flexibility = wrinkles and sagging SOME FUN STUFF TO KNOW ABOUT SKIN Scars: from greek word schara (place of fire) -damaged dermis is replaced with tissue of inferior quality and rich in collagen -scars do not have sweat or oil glands and do not have hair -redness of the scar is due to inflammation and is not permanent - two common types: 1. hypertropic (red and raised, do not grow beyond boundaries of original wound 2. keloid – permanently growing scars – can lead to benign tumors - more common in darker skin, common on chest and shoulders Stretch marks: extensive and quick distortion of the dermis damages it -no recoil of skin after stretching -leads to breaking of elastic and collagen fibers in the dermis - replaced with new, poorly organized collagen Retin-A (tretinoin) : increases blood flow to the dermis -promotes dermal repair -decreases wrinkles and stretch marks Subcutaneous layer -also referred to as the hypodermis or superficial fascia -connects the skin to underlying muscles or other organs -made up of: 1. loose connective tissue 2. adipose tissue - “baby fat” - also contains elastic fibers for flexibility -fat content helps reduce heat loss -fat distribution changes with age and gender: -males – neck, upper arms, abdomen and lower back -females – breasts, abdomen, buttocks, hips and thighs -contains large arteries and veins – helps give the skin its color -the superficial layers of the hypodermis are the sites for drug injections - hypodermic Accessory Structures Hair follicles Sweat glands Sebaceous/Oil glands Nails Hair & Hair follicles •over all epidermal surfaces except soles of feet, palms of hand, sides of fingers and toes and portions of external genitalia •approx. 5 million hairs on the body •formed in hair follicles •Comprised of three major regions: 1. Hair bulb – contains the living, hair papilla 2. Hair root – site of connection with arrector pili (smooth muscle) and a sebaceous gland 3. Hair shaft – portion of the hair above the sebaceous gland -manority of it is exposed above the skin Hair structure -hair papilla – found at the base of the hair within the hair bulb -contains the stem cells of the hair = hair matrix -also contains capillaries and sensory nerves for touch -epithelial tissue surrounding the matrix make up the hair bulb -hair root: projects up from the hair bulb -surrounded and protected by a hair follicle -site of attachment of arrector pili smooth muscle (pulls hair upright for better sensation) -continues above the sebaceous gland as the hair shaft – also exposed above the surface of the skin Hair Production -hair production = specialized keratinization -hair is produced from the hair matrix – epithelial layer similar to stratum basale (contains living cells of the hair - many are stem cells) -keratinocytes differentiate within the matrix – cells immediately produce the keratin of hair -keratin forms into an outer cortex and inner medulla -cortex – hard keratin - stiffness -medulla – soft keratin – flexible -single layer of dead cells encloses the cortex of the hair = cuticle -within the dermis – hair is enclosed in a protective follicle (made also by the hair matrix Follicle -found in the dermis surrounding the hair -often rooted in SQ layer -wall is comprised of four layers: 1. internal root sheath: surrounds the root & deeper portion of shaft -produced by the cells of the hair matrix 2. external root sheath: runs continuously from the hair bulb to the skin surface to enclose the hair 3. glassy membrane: thickened basement membrane between external root sheath and the connective tissue sheath 4. connective tissue sheath Exocrine Glands •secretions are discharged out onto the surface of the epithelium that lines body cavities or out onto the skin •many exocrine glands secrete to the exterior via tubes called ducts •exocrine secretions: 1. perspiration 2. digestive enzymes 3. milk 4. mucous 5. oil Exocrine glands • you can classify exocrine glands many ways • one way – by the consistency of what they secrete – e.g. serous • another way – by their structure – e.g. multicellular • last way – by the mode of secretion – e.g. holocrine •exocrine gland types – consistency of secretion: 1. serous - watery fluid that contains enzymes e.g. saliva – parotid salivary gland 2. mucous - glycoproteins called mucins that absorb water to form a slippery mucus e.g. sublingual salivary gland 3. mixed - more than one type of gland cell -produces different types of secretions - mucus and serous e.g. submandibular salivary gland •exocrine gland structure: • Unicellular are single-celled glands e.g. goblet cells •Multicellular glands -two characteristics to classify: •shape of the secretory portion •branching pattern of the duct -simplest multi-cellular gland is a secretory sheet •secrete into a compartment •e.g. gastric epithelium Modes of Secretion: Exocrine glands 1. merocrine: -contents are released through exocytosis 2. apocrine: loss of cytoplasm from the apical portion of the cell together with secretory product e.g. milk secretion 3. holocrine: results in death of gland cell -entire cell fills with secretory product and then bursts e.g. sebaceous glands associated with hair follicles Skin glands 1. Sweat/Sudoriferous – of the serous type 2. Oil/Sebaceous – of the mucus type 3. Wax/ Ceruminous Sebaceous glands/Holocrine glands -”sebace” = greasy -secreting portion is within the dermis -most open onto hair follicles (some do not) -glands located at the lips, glans penis, labia minora and eyelids - open directly to the skin surface -absent on palms and soles -large in size and numbers on breast, face, neck and upper chest • sebaceous glands secrete an oily substance = sebum • acne = inflammation of a sebaceous gland due to the presence of bacteria – may cause a cyst or sac of connective tissue to form which destroys epithelial cells – known as cystic acne Sudoriferous Glands •3 to 4 million glands in the body •sudori = sweat, ferous = bearing •released by exocytosis into hair follicles or onto the skin surface •two main types: • 1. Eccrine sweat glands (merocrine) •simple, coiled tubular glands - serous •secretion through exocytosis •found throughout the skin, PLUS margins of lips, nail beds, glans penis and clitoris •most numerous in forehead, palms and soles •secretory portion is located in the reticular layer of dermis •ends as a pore in the skin •main function is to regulate body temperature through evaporation •also functions in waste elimination •thin, watery perspiration - about 600 ml per day -water, sodium, chloride, urea, uric acid, ammonia, glucose, amino acids -perspiration can be: a. insensible - evaporates before being perceived b. sensible - larger amounts, can be seen and felt • Apocrine sweat glands • makes odorous secretion - secretions are slightly more viscous than merocrine • simple, coiled tubular glands – secretory portion in hypodermis • skin of axilla (armpit), groin, areolae, bearded region of face in males • released by a portion of the cell breaking off and disintegrating • secretory portion located in SQ layer - opens onto a hair follicle • same components as sweat + lipids and proteins • do not function until after puberty Sudoriferous gland – merocrine/apocrine • Mammary glands – Large, complex apocrine sweat glands •Ceruminous glands •modified sweat glands •in ear canal •secretory portion is in the SQ layer, deep to sebaceous glands •secrete either directly into the ear canal or into the ducts of the sebaceous glands •produce waxy cerumin - together with the hairs of the canal provides protection