Learning Objectives
advertisement

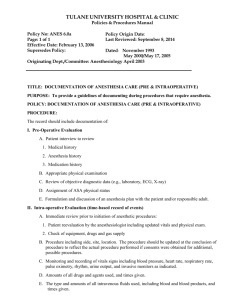
The Role of Short-acting Opioids in Current Anesthesia Practice Sponsored by Integrity Continuing Education, Inc. Supported by an educational grant from Mylan. Bernadette Henrichs, PhD, CRNA Professor & Director Nurse Anesthesia Program Goldfarb School of Nursing Barnes-Jewish College St. Louis, Missouri 2 Overview of General Anesthesia • Goals of general anesthesia – Rapid induction and maintenance of optimal operating conditions – Reduction of side effects – Rapid emergence and recovery • A combination of agents is used to induce and maintain general anesthesia in current practice – IV hypnotics and sedatives – Volatile inhalational agents – Opioids – Muscle relaxants Mandel, J. E. J Clin Anesth. 2014;26(1 Suppl):S1-7. 3 Volatile Inhalation Agents for the Maintenance of General Anesthesia • Common agents include sevoflurane (SEVO), desflurane (DES), and nitrous oxide (N2O) • N2O with SEVO or DES provides fast, reliable recovery and lowers risk of myocardial depression • Associated adverse events: SEVO/DES N 2O *May • Isolated cases of hepatotoxicity • • • • • Nausea and vomiting Diffusional hypoxemia Pulmonary bleb rupture Pneumothorax expansion Inactivation of vitamin B12* have deleterious effects in critically ill and pediatric patients; Mandel, J. E. J Clin Anesth. 2014;26(1 Suppl):S1-7. 4 Total Intravenous Anesthesia (TIVA) • An alternative to the use of volatile agents for maintenance of anesthesia • Anesthesia is produced entirely using IV anesthetics administered by target-controlled infusion or manual injection • Short-acting opioids play a central role (though not always required for minimally stimulating procedures) • Short-acting agents enable rapid recovery even after long infusions Cole CD, et al. Neurosurgery. 2007;61(5 Suppl 2):369-377. DeConde AS, et al. Int Forum Allergy Rhinol. 2013;3(10):848-854. Lerman J, et al. Paediatr Anaesth. 2009;19(5):521-534. Mandel JE. J Clin Anesth. 2014;26(1):S1-S7. Mani V, et al. Paediatr Anaesth. 2010;20(3):211-222. 5 IV Agents for the Induction and Maintenance of General Anesthesia IV AGENT Propofol Etomidate Ketamine POTENTIAL ADVANTAGES POTENTIAL DISADVANTAGES – Good recovery profile – Short half-life – Low PONV incidence – Bradycardia – Hypotension – Burning sensation – Preferred if vasodilation and cardiac depression are contraindicated – Adrenal insufficiency – Higher PONV incidence – Burning sensation – Preferred for reactive airway patients (bronchodilatory) – Cardiovascular stimulation – Hallucinations, vivid dreams, delirium – Benzodiazepines can improve but may slow emergence and recovery Mandel, J. E. J Clin Anesth. 2014;26(1 Suppl):S1-7. 6 Clinical Comparisons of Anesthesia Techniques • TIVA compared to inhalation anesthesia (IA) in vertebral disk surgery: – Shorter recovery times (spontaneous ventilation, extubation, eye opening, and ability to give name and date of birth)* – Less PONV – Greater analgesic demand • TIVA compared to IA in pediatric ENT surgery: – Lower perioperative heart rate – Less postoperative agitation • TIVA and balanced volatile anesthesia in intracranial surgery were found to be comparable *P<.05 Gozdemir M, et al. Adv Ther. 2007;24(3):622-631. Grundmann U, et al. Acta Anaesthesiol Scand. 1998;42(7):845-850. Magni G, et al. J Neurosurg Anesthesiol. 2005;17(3):134-138. 7 Monitoring of Vital Signs to Assess Depth of Anesthesia • Potential signs of intraoperative awareness/stress: – Tachycardia (rapid heart rate) – Hypertension – Sweating – Lacrimation (tear production) – Movement/grimacing – Tachypnea (rapid breathing) • New technologies for monitoring (EEG, BIS) – Helps to indicate the level of unconsciousness – Does not guarantee against intraoperative awareness Shepherd J. Health Technology Assessment 2013;17:34. 8 Maintaining Appropriate Depth of Anesthesia • Excessive level of anesthesia – Increases risk of postoperative nausea, vomiting, and cognitive dysfunction • Insufficient level of anesthesia – Places patient at risk for intraoperative awareness – Although relatively rare, intraoperative awareness can cause depression, anxiety, and post-traumatic stress disorder Shepherd J. Health Technology Assessment. 2013;17:34. 9 Hemodynamic Stability During Surgery • Hemodynamic instability can result in complications • Hemodynamic measures are important indicators of the following: – Sufficient cardiac output – Adequate SV; Volume status – Organ perfusion – Adequacy of pain control – Depth of anesthesia Lendvay V, et al. J Anesthe Clinic Res. 2010;1:103. Cove ME, Pinsky MR. Best Pract Res Clin Anaesthesiol. 2012;26(4):453-462. 10 Rationale for the Use of Short-acting Opioids in General Anesthesia 11 Opioid Receptors and Response to Stimulation Receptor Response Mu-1 • Supraspinal analgesia Mu-2 • • • • Depression of ventilation Cardiovascular effects Physical dependence Euphoria Delta • Modulate mu receptors Kappa • • • Spinal analgesia Sedation Miosis Sigma • • Dysphoria Hypertonia 12 Advantages of the Use of Opioids for General Anesthesia • Analgesia – Blunts neuroendocrine activation • Hemodynamic stability – No direct myocardial depression – Blunts catecholamine response to noxious stimuli • Decreased stress response – Attenuates stress response during surgery • Decreased need for hypnotic anesthetics – Less propofol needed Brown EN., et al. Annu Rev Neurosci. 2011;34:601-628. Fukuda K (2010). Opioids. In RD Miller et al., eds., Miller's Anesthesia, 7th ed., pp. 2519-2700. Wilmore DW. Ann Surg. 2002;236(5):643-648. Specific Benefits Associated with the Use of Short-acting Opioids • Minimal effects of drug accumulation • Predictable and rapid onset and offset • Rapid patient response to titration allows close management of intraoperative status • Potential for faster recovery time and reduced PONV • Benefits are not generally affected by gender, age, weight, or renal/hepatic function Wilhelm W, et al. Crit Care. 2008;12 (Suppl 3):S5. Egan TD. Curr Opin Anaesthesiol. 2000;13(4):449-455. Egan TD, et al. Anesthesiology. 1996;84(4):821-833. Minto CF, et al. Anesthesiology. 1997;86(1):10-23. Desirable Characteristics of the µ-Opioids Characteristic Alfentanil Fentanyl Remifentanil Sufentanil µ-Opioid receptor selectivity X X X X No histamine release X X X X Rapid response to titration X Rapid, predictable offset of opioid effects (5-10 min) X Elimination independent of renal or hepatic function X 15 Remifentanil Hydrolysis by Non-specific Esterases in the Blood and Tissues Remifentanil O CH3-O-C-CH2-CH2N O C-OCH3 O N-C-CH2CH3 >95% Major Metabolite O (Inactive) O C-O-CH3 O H-O-C-CH2-CH2N H-N N-C-CH2CH3 O N-C-CH2CH3 GR90291 Egan TD. Clin Pharmacokinet. 1995;29(2):80-94. C-OCH3 O GR94219 Pharmacokinetic Properties of µ-Opioids Pharmacokinetics Alfentanil Fentanyl Remifentanil Sufentanil Onset: blood-effect site equilibration, mean 0.96 min 6.6 min 1.6 min 6.2 min Organ-independent elimination No No Yes No Nonspecific esterase metabolism No No Yes No 50-55 min† >100 min† 3-6 min 30 min† Offset: context-sensitive half-time, mean* *The time required for drug concentrations in blood or at effect site to decrease by 50%. Based on a 3-hour infusion. † Increases with increasing infusion duration due to accumulation. Data derived from manufacturers’ labeling and Egan TD, et al. Anesthesiology. 1993;79:881-892. Egan TD, et al. Anesthesiology. 1996;84:821-833. Scott JC, et al. Anesthesiology. 1991;74:34-42. 17 Practical Considerations: Rapid Onset ADVANTAGES • Rapid response to titration and bolus DISADVANTAGES • Increased risk for: – Bradycardia • Control of anesthetic depth – Hypotension • Hemodynamic stability – Apnea • Predictable plasma & receptor level – Chest wall rigidity Proportion of Steady-State Ce (%) Opioid Infusion Front-end Kinetics: Quick to Steady State 100 Remifentanil 80 Morphine Alfentanil Sufentanil 60 Fentanyl 40 20 Infusion begins at time zero 0 0 100 200 300 400 500 600 Infusion Duration (min) Egan TD (in Miller & Pardo). Elsevier;2011. 19 Time to 50% Decrement in Ce (%) Opioid Infusion Back-end Kinetics: Rapid Offset After Infusion 400 Fentanyl 350 Morphine 300 250 200 150 100 Alfentanil 50 Sufentanil Remifentanil 0 0 100 200 30 400 500 600 Infusion Duration (min) Egan TD (in Miller & Pardo). Elsevier;2011. 20 Mean Concentration Over Time With Short-acting Opioids Discontinuation of infusion Mean Concentration (ng/mL) 100 (n=5) 0.5 mcg/kg/min Alfentanil Remifentanil 10 1 (n=6) 0.05 mcg/kg/min 0.1 0 60 120 180 240 300 360 420 480 Time (min) ULTIVA [Mylan Inc.] Available at: http://www.ultiva.com/files/Ultiva-Prescribing-Info.pdf 21 Practical Considerations: Rapid Offset ADVANTAGES • Rapid response to titration • Predictable emergence • High-dose opioid technique without need for post-op ventilation • Ideal for TIVA DISADVANTAGES • No residual analgesia – Hemodynamic instability Procedure-associated Variability in Opioid Pharmacodynamics Probability of No Response (%) (n=37) 100 Intubation 50 Skin Incision Skin Closure 0 0 200 400 600 Plasma Alfentanil (ng/mL) Ausems ME, et al. Anesthesiology. 1986;65:362-373. 800 1000 Opioid Pharmacodynamic Variability Probability of No Response to Surgical Incision (%) 100 50 0 200 400 Plasma Alfentanil (ng/mL) Ausems ME, et al. Anesthesiology. 1988;68:851-861. 600 Risks Associated with the Use of Opioids in General Anesthesia • Respiratory depression • Bradycardia • Chest wall/laryngeal muscle rigidity • PONV • Pruritus • Delayed emergence • Dependency • Potential hyperalgesia Bowdle TA. Drug Saf. 1998;19(3):173-189. Egan TD. Clin Pharmacokinet. 1995;29(2):80-94. Fletcher D, et al. Br J Anaesth. 2014;112(6):991-1004. Komatsu R, et al. Anaesthesia. 2007;62(12):1266-1280. Choosing an Anesthetic Technique 26 Discussion Questions: Technique Considerations • How do you determine which technique is most appropriate for a given patient? • What are the primary concerns associated with each technique? Impact of Inhalation vs Intravenous (IV) Administration of Agents • Less PONV and greater patient satisfaction has been observed with the following: – IV induction compared to inhalation induction* – TIVA compared to an inhalation component • Emergence and discharge for outpatients is essentially identical • Inhalational anesthesia may be economically advantageous over TIVA *Both followed by inhalation maintenance. Kumar, G., et al. Anaesthesia. 2014. [Epub ahead of print] Joshi GP. Anesthesiol Clin North Am. 2003;21(2):263-272. 28 The Anesthesia Technique You Use Should Be Based on Your Goals • Balanced anesthesia with opioid and volatile agent – Safe – Practiced for decades • TIVA – Safe – Relative newcomer to the OR – Outpatient > inpatient – May impact patient satisfaction OR, Operating Room Goals of Neuroanesthesia • Hemodynamic stability without vasodilators • Improved ability to rapidly change anesthetic depth • Rapid recovery with early ability to assess neurologic function • Improved SSEP monitoring with TIVA SSEP, somatosensory evoked potential. Goals of ENT • Hemodynamic stability without vasodilators • Decreased bleeding, improved operative conditions during nasal/sinus surgery or tonsillectomy • Rapid awakening, rapid ability to protect airway, rapid recovery Case Study #1 32 Case Study #1: 17-year-old Female • Procedure: Septoplasty and sinus endoscopy • History: – Significant history of nasal passage obstruction and difficulty breathing – History of chronic sinusitis beginning at age 3 • Surgical history: – Tonsillectomy at age 7 related to obstructive sleep apnea (OSA); complicated by prolonged paralysis to succinylcholine Case Study #1: 17-year-old Female (cont’d) • Comorbidities: – Asthma – Obesity – OSA with nasal obstruction • Current medications: – Saline nasal irrigation qd – Albuterol prn • Allergies: – Penicillin – No other known allergies Case Study #1: Consideration of Patient Characteristics • How do the patient’s characteristics influence your approach to formulating a plan for anesthesia? – OSA – Obesity – Asthma – Atypical pseudocholinesterase deficiency • Specific concerns with regard to this type of surgical procedure: May be stimulating at times but no incision to close at end of case Emergence & Recovery 36 Short-acting Opioid Improves Time to Orientation Compared With N2O 1.0 Proportion Not Oriented Remifentanil 0.8 Nitrous oxide 0.6 Infusion of remifentanil 0.085 µg/kg/min compared with 66% N2O 0.4 0.2 0.0 0 5 10 15 20 25 Time (min) Mathews DM, et al. Anesth Analg. 2008;106:101-108. 37 Comparison of the Short-acting Opioids: Impact on Patient Recovery • Similar PONV is observed with fentanyl, remifentanil, alfentanil, and sufentanil • Use of remifentanil vs other short-acting opioids is associated with the following: – Faster postoperative recovery – Less respiratory depression – Higher postoperative analgesic requirements – More shivering Reviewed in: Komatsu R, et al. Anaesthesia. 2007;62(12):1266-1280. 38 Case Study #2 39 Case Study #2: 73-year-old Male • Procedure: Right carotid endarterectomy • Comorbid conditions: – – – – Coronary artery disease Type 1 diabetes Hypertension Peripheral vascular disease • Surgical history: – Left femoral popliteal bypass at age 71 – Stent inserted at age 68 Case Study #2: 73-year-old Male (cont’d) • Current medications: – Lisonopril 20 mg qd – Insulin glargine 0.2 units/kg/day • Renal evaluation: – Renal insufficiency determined by glomerular filtration rate (GFR) of 61 mls/min/1.73m2 • Vascular evaluation: – 90% occlusion of right carotid – 50% occlusion of left carotid • Allergies: – No known allergies Case Study #2: Questions for Consideration • What considerations should be given for: – Regional vs general anesthesia? – Tracheal intubation vs laryngeal mask airway (LMA) device? • What monitoring would you employ intraoperatively? • Consider the patient’s medical history (HTN) and renal impairment in the anesthetic plan • Important to consider quick emergence to assess neurological function Case Study #3 43 Case Study #3: 42-year-old Female • Procedure: – Multi-level laminectomy with lumbar fusion – Intraoperative neurophysiologic monitoring (sensory evoked potentials, motor evoked potentials) • Surgical history: – Previous back surgery to repair herniated disc 3 years ago • Medical history: – Current smoker • Current medications: – Naproxen sodium 500 mg bid (discontinued 10 days ago) Case Study #3: Questions for Consideration • What considerations are given for TIVA vs mixed anesthesia in this patient? • Consider intraoperative monitoring of this patient • Consider surgeon request for possible intraoperative wake up for neurologic examination • Consider patient’s history of chronic pain medication Intraoperative Neurophysiological Monitoring • Main modalities: – Somatosensory evoked potentials (SSEPs) – Motor evoked potentials (MEPs) – Electromyography (EMGs); transcranial monitoring • While both inhaled and intravenous agents blunt signal attainment, depression is greater with inhaled agents Deiner S. Semin Cardiothorac Vasc Anesth. 2010;14(1):51-53. 46 Case Study #3: Anesthetic Plan • TIVA with propofol and fast-acting opioid infusion • If intraoperative wake up is necessary, it will be possible • Consider patient’s history of chronic pain medication – Give pain medicine before emergence – IV Acetaminophen; IV NSAID; longer-acting narcotic Emergence and Recovery: Considerations • Goal is to prepare for and have a smooth transition to postoperative analgesia • Early planning is essential with an agent with a rapid offset of action (within 5-10 minutes) – Non-cumulative effects are beneficial during surgery, but a disadvantage postoperatively in terms of pain control – Need to be prepared and address pain • Risks for obstruction and for pulmonary aspiration are also important to consider Plasma Propofol Concentration (mcg/mL) Propofol Emergence Data Target plasma concentration Recovery after: 10-day infusion 10-hour infusion 1-hour infusion Awakening 1.00 0.75 0.50 0.25 0.00 0 20 40 60 80 Minutes After End of Infusion DIPRIVAN (propofol) injection, emulsion [APP Pharmaceuticals, LLC]. Available at: http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=ee0c3437-614d-4631-a061-257f5f60c70b. 49 Postoperative Management: Analgesia 50 Postoperative Pain • Postoperative pain is a significant cause of delayed discharge after ambulatory surgery • Good pain control is important for prevention of negative outcomes: – Tachycardia – Hypertension – Myocardial ischemia – Decreased alveolar ventilation – Poor wound healing • Pain control must be individualized Vadivelu N, et al. Yale J Biol Med. 2010;83(1):11-25. 51 Options for Postoperative Pain Management • Choice of analgesia should be a multimodal approach: – Nonsteroidal agent administered IV or IM – IV acetaminophen – Major nerve block – Local anesthetic wound infiltration – Long-acting opioids administered 20 to 30 minutes before discontinuation of certain short-acting opioids – Consider epidural administration of an opioid and/or local anesthetic IM, intramuscular Opioids in Postoperative Analgesia • Give opioids prior to emergence as needed – IV Acetaminophen if not given at induction – Ketorolac 30 mg IV ~30 min or Caldolor IV – Dilaudid 0.2-2.0 mg IV ~ 20-30 min – MSO4 0.1 to 0.2 mg/kg IV ~20 to 30 min – Fentanyl 1 to 1.5 u/kg IV ~5 min • Dose epidural if epidural placed • Surgeon: Infiltrate with long-acting local anesthetic • Consider continuing remifentanil 0.05 to 0.1 mcg/kg/min in PACU Considerations for Special Populations • Age; Elderly more sensitive to narcotics • Body mass effects; Obese more sensitive to narcotics • Comorbid conditions • Current medications Strom C, et al. Anaesthesia. 2014;69(S1):35-44. Lerman J. Eur J Anaesthesiol. 2013;30(11):645-650. Ingrande J, et al. Br J Anaesth. 2010;105 (S1):16-23. Hachenberg T, et al. Curr Opin Anaesthesiol. 2014;27(4):394-402.Licker M, et al. Int J Chron Obstruct Pulmon Dis. 2007;2(4):493-515. 54 Summary • Opioids used in anesthesia play a critical role in minimizing surgical pain and the associated adverse effects on patient outcomes • The pharmacokinetic profiles of newer short-acting opioids are characterized by lower drug accumulation and rapid, predictable onset and offset • The resulting rapid response to titration of short-acting opioids enables close intraoperative management of hemodynamics, patient stress response, and depth of anesthesia • With appropriate use, short-acting opioids have the potential to improve recovery and overall patient experience and satisfaction 55 Thank you!