Imaging in Acute Facial Nerve Paralysis
advertisement
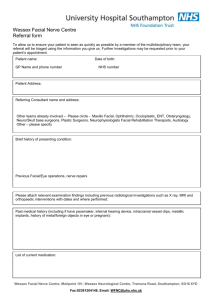
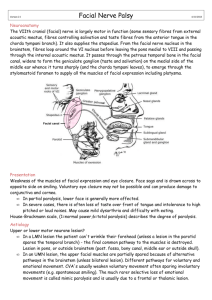
Imaging in Acute Facial Nerve Paralysis M Castillo, MD, FACR Department of Radiology University of North Carolina, Chapel Hill Overview of Presentation • Introduction • Review of facial nerve anatomy • Clinical and Imaging features of Bell’s palsy – Typical – Atypical • Other causes of acute facial paralysis Introduction • Bell’s palsy accounts for 75% of cases of acute facial nerve (7th cranial nerve) paralysis • Imaging is not needed in majority of patients unless they have atypical features • W/atypical features, MR & CT may demonstrate potentially treatable lesions affecting facial nerves • Facial nerves can be affected anywhere along their course Anatomy Review • Facial nerve nuclei lie in reticular formation of brainstem, ventral to floor (tegmentum) of 4th ventricle(4) • Motor Nuclei: – Efferent fibers surround nuclei of CN VI & form small mounds on floor of 4th ventricle (facial colliculi) • Non-Motor Nuclei: – Salivatory – Solitary Facial colliculus • Efferent fibers surround 6th CN nucleus & exit at cerebellopontine angle (CPA) • 7th nerve courses into internal auditory canal (IAC) – Within superior anterior quadrant(6) Ant Post Fallopian Canal • Exits IAC via Fallopian canal – Narrowest point throughout entire course – Felt to be culprit in facial nerve compression in Bell’s palsy & other causes of nerve swelling Geniculate ganglion • Progress to geniculate ganglion – Gives rise to greater superficial petrosal nerve • Contains taste axons from tongue & somatic fibers • Fibers then course posteriorly under lateral semicircular canal in middle ear (tympanic portion) • Fibers angle back & inferiorly at “second genu” diving the descending canal – Here last somatic & parasympathetic fibers separate from facial nerve via the chorda tympani nerve Mastoid segment Tympanic Portion • Facial nerve exits skull base at stylomastoid foramen • Facial nerve angles superiorly & anteriorly behind posterior margin of vertical mandibular ramus – Just before entering parotid gland, inferior branches originate • Posterior auricular, digastric & stylohyoid – Within substance of parotid gland, superior branches arise • Temporal, zygomatic, buccal, orbicularis oris, mandibular & cervical Clinical Signs Suggesting Site of Facial Nerve Lesion • Upper facial territory is supplied by bilateral motor cortices • Lower facial territory is supplied only by contralateral motor cortex • Therefore, unilateral central lesions spare upper face • Lesions distal to geniculate ganglion – Mostly motor abnormalities • Lesions proximal to geniculate ganglion – Motor, gustatory & autonomic abnormalities Typical Bell’s Palsy • Incidence – 15–30 per 100,000 – Usually during winter • Etiology not entirely understood – Possibly viral (Herpes Simplex Virus) or idiopathic • Viral infection of facial nerve results in demyelination, inflammation & swelling – Traps nerve in narrow confines of fallopian canal • Diagnosis of exclusion – Made only when clinical & imaging (if necessary) findings are supportive Typical Bell’s Palsy • Usually a clinical diagnosis – Acute onset unilateral (lower or upper) facial paralysis, posterior auricular pain, decreased tearing, hyperacusis (30%) & disturbances of taste – By physical examination, Bell’s palsy divided according to classification by House and Brackman • Grades 1 & 2 have better outcomes with worse outcome as grade increases. • 80-90% recover completely – Over age 60, only 40% recover completely Imaging in Typical Bell’s Palsy • Imaging in typical Bell’s palsy is not usually necessary – When necessary, MRI is best • Normal facial nerve distal to geniculate ganglion may enhance – Facial nerve proximal to geniculate ganglion does not normally enhance • In patients with Bell’s palsy, enhancement of facial nerve in fallopian & ICA is typical C/o Dr. M. Michel, Wisconsin Atypical Bell’s Palsy • Clinical features – Slower onset of symptoms – Bilateral – Recurrence • Numbness is not unusual • Progression beyond seven days suggests another cause Imaging in Atypical Bell’s Palsy C/o Dr. M. Michel, Wisconsin Alternative Causes of Acute Facial Nerve Paralysis • Atypical signs & symptoms which suggest etiology other than Bell’s palsy require imaging • Clinical history is crucial in distinguishing etiologies • Choice of imaging technique depends on clinical suspicion Lyme Disease • Lyme disease (borreliosis) – Endemic areas (Northeast USA, central Europe, Scandinavia, Canada) – Consider in children w/atypical facial palsy • Imaging: small white matter lesions similar to multiple sclerosis, enhancement of facial & other cranial nerves • Bilateral facial paralysis: 25% • Important to make diagnosis early because it is curable early w/antibiotics Ramsay Hunt Syndrome • Caused by reactivation varicella zoster virus (herpes virus type 3) • Facial paralysis + hearing loss +/- vertigo – Herpes zoster oticus • Two-thirds of patients have rash around ear • Other cranial nerves, particularly trigeminal nerves (5th CN) often involved • Worse prognosis than Bell’s (complete recovery: 50%) • Important cause of facial paralysis in children 6-15 years old C/o Dr. M. Michel, Wisconsin Infectious causes • Acute facial paralysis may result from bacterial or tuberculous infection of middle ear, mastoid & necrotizing otitis externa • Incidence of facial paralysis with otitis media: 0.16% – Infection extends via bone dehiscences to nerve in fallopian canal leading to swelling, compression & eventually vascular compromise & ischemia • Immune compromised patients are at risk for pseudomona infection • Poor prognosis (complete recovery is < 50%) Tuberculosis Parotid & peri-parotid disease HIV Infection Bezold’s abscess & coalescent mastoiditis Trauma • Most acute post traumatic facial palsies are due to t-bone fractures • Historically fractures classified as longitudinal or transverse with transverse carrying risk of permanent paralysis – Longitudinal fracture usually leads to temporary paralysis from concussion & swelling of nerve – Transverse fracture can lead to transection of nerve • In all types of paralysis due to fracture, usually the region of geniculate ganglion is involved Neoplasms • 27% of patients with tumors involving the facial nerve develop acute facial paralysis • Most common causes: schwannomas, hemangiomas (usually near geniculate ganglion) & perineural spread such as with head and neck carcinoma, lymphoma & leukemia • Other neoplasms can also involve the facial nerve – Adults: metatstatic disease, glomus tumors, vestibular schwannomas & meningiomas – Children: eosinophilic granuloma & sarcomas Hemangioma Hemangioma Facial Nerve Schwannoma Perineural Tumor Spread Glomus Tumor • Glomus tumors arising from jugular bulb (jugulare) and/or middle ear (tympanicum) may involve the facial nerve Other tumors Rhabdomyosarcoma & squamous cell carcinoma of the EAC Vestibular Schwannoma • Common tumor • However, facial nerve is resistant to compression – Therefore, tends to produce facial paralysis mostly when they attain a large size Vestibular Schwannoma Common tumor -However, facial nerve is resistant to compression, thus, tends to produce facial paralysis mostly when they attain a large size - Meningioma • Second most common primary tumor of cerebellopontine angle • Rarely results in facial paralysis Rhabdomyosarcoma Miscellaneous Causes Hypertrophic Polyneuropathy • Hypertrophic polyneuropathies occasionally lead to facial paralysis Wegener’s Granulomatosis Other Causes • Guillain-Barre Syndrome – Ascending paralysis • Iatrogenic – Temporal bone surgery • Excision of vestibular schwannoma has <10% chance of paralysis • Middle ear surgeries – Babies who required forceps delivery • >90% recovery Melkersson-Rosenthal Syndrome • Acute episodes of facial paralysis – Facial swelling – Fissured tongue • “Scrotal” tongue • Very rare • Familial but sporadic – Usually begins in adolescence • Leads to facial disfigurement • No definite therapy Conclusion • While Bell’s palsy does not typically require imaging for diagnosis, imaging evaluation is important in the work-up of patients with atypical or unusual presentations of acute facial nerve paralysis, identification of discreet lesions may lead to a change in management of these patients.