Unit One * Key Concepts
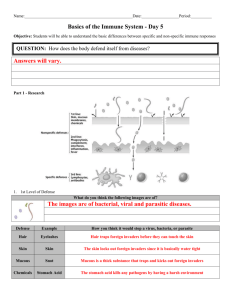
advertisement
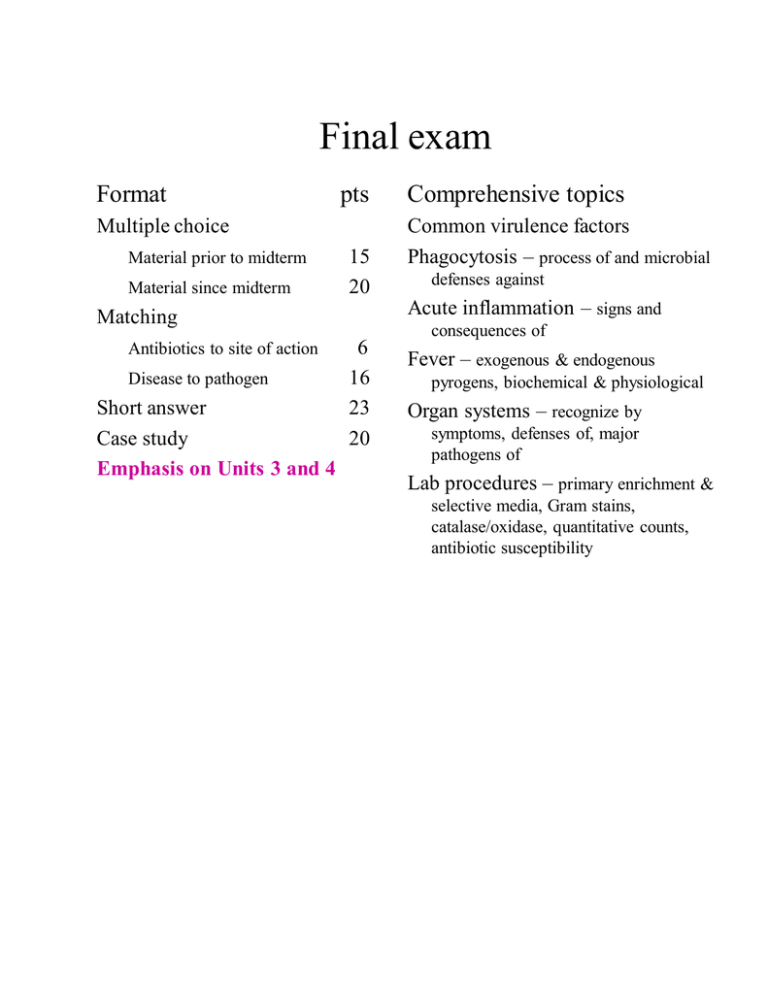
Final exam Format pts Multiple choice Material prior to midterm Material since midterm 15 20 Matching Antibiotics to site of action Disease to pathogen Short answer Case study Emphasis on Units 3 and 4 6 16 23 20 Comprehensive topics Common virulence factors Phagocytosis – process of and microbial defenses against Acute inflammation – signs and consequences of Fever – exogenous & endogenous pyrogens, biochemical & physiological Organ systems – recognize by symptoms, defenses of, major pathogens of Lab procedures – primary enrichment & selective media, Gram stains, catalase/oxidase, quantitative counts, antibiotic susceptibility Unit One – Key Concepts Review of the microbial pathogens Viruses • Not living, not cells • Obligate intracellular pathogens • Enveloped vs naked • Interact with target cells via highly specific virus surface protein to host target cell receptor interactions • Enter the target cell by one of 3 mechanisms (depending on type of virus) RME, fusion, translocation • Infections are often “silent”, not alerting the immune system or producing signs (such as acute inflammation) until host cells are damaged (lysis) or altered (viral antigen + MHC I). Bacteria • Prokaryotic • For purposes of diagnostic bacteriology – 2 staining types: Gram neg vs Gram pos – staining properties based on differences in cell wall structure • Gram pos – thick peptidoglycan (multiple layers); Gram neg. – thin peptidoglycan (single layer), outer lipid membrane. • *Signs and symptoms of disease often attributed to bacterial cell wall peptidoglycan, teichoic acids (GP), and LPS (GN) that induce acute inflammation, fever; Secretion of enzymes (like coagulase); Secretion of toxins (exotoxins – lots of, very important) • Role of capsules in delaying phagocytosis • Attachment mechanisms, either general like sticky capsules, or specific like fimbriaereceptor interactions. Fungi and Protozoa • Eukaryotic organisms, like the host – will limit treatment options • Spores (asexual reproduction in fungi), cysts (an environmentally stable, infectious life cycle stage of protozoa) • Deep, systemic infections often indicate an immunocompromised host (especially deep fungal infections) Normal Microbiota Important biological defense against pathogen occupation of a site – densities greatest in the colon, least in stomach and on epithelium of the skin. May cause opportunistic infections if get into the wrong site (like E. coli in peritoneal cavity) or if host becomes compromised (by viral infection for example). Review of host defenses 3 lines of host defenses o exterior defenses against entry into and establishment at the site (chemical, mechanical, biological – site specific - think about for each system we covered) o interior non-specific defenses o interior specific defenses (antigen-specific) Host non-specific interior defenses o INFLAMMATION!! – a complex, dynamic process, the cornerstone of the nonspecific interior defenses - swelling (edema), redness (erythema), tenderness, heat – increased WBC, and particularly increased PMNs o Complement activation o Acute phase proteins o Phagocytosis by macrophages and neutrophiles (=PMNs) o Cytolytic cells – NK, eosinophils Cellular communication/coordination via cytokines o What cells secrete cytokines, what cytokines do they secrete, what cells do those cytokines act upon. TH – function is to “turn on” or to enhance the activation/effectiveness of other host defense cells. Does this via IL2 (acts on other lymphocytes) and gamma interferon (acts on macrophages) Tc – functions to lyse and thereby destroy host cells infected with intracellular pathogens, bacteria and esp. viruses. (Recognizes infected cells via TC receptor to foreign antigen complexed with host MHC1 interactions. Secretes perforin, TNF, granzyme membrane pores, triggers apoptosis) Plasma cells (effector B lymphocytes) secrete antibodies Functions of antibodies o Neutralizing (virus attachment, bacterial attachment, bacterial toxin attachment) – secretory IgA (=sIgA), found in body fluids, esp. mucus. o Opsonizing (an attachment for phagocyte receptors, enhances phagocytosis) – IgG o Agglutination (enhances phagocytosis, but not as an opsonin) – IgM Memory B and T lymphocytes – secondary response may be so swift that there are few or no symptoms of infection. Unit Two – Key Concepts Entry, exit, transmission – review for each major system (RT, UT, GI, NS, skin). Microbial strategies to avoid host non-specific interior defenses o Anti-complement, and esp. anti-phagocytic defenses Surface infections (non-specific defenses at the surface impt., generally shorter incubation periods) vs systemic infections (T and B lymphocytes become more impt., generally longer incubations periods) Microbial strategies to avoid specific defenses o Preventing or delaying recog. of antigens and antigenic variation of most importance. Pathological consequences of infection – emphasized also in the clinical cases o Pathology caused directly by the microbe Exotoxins Endotoxins (=LPS) o *Fever - how is it induced at both chemical/cellular levels and physiological levels. o Pathology as a result of the immune response to the microbe Complement-mediated damage Damage resulting from acute inflammation * o Pathology as a result of specific defenses – hypersensitivities, also TH secreted cytokines (overabundance of IL-2 for example) Unit Three – Key Concepts We covered these systems via clinical cases Lower respiratory tract Urinary tract Gastrointestinal tract Nervous system Infections of wounds We covered these pathogens Gram positive Gram negative Cocci Rods Catalase + Staphylococcus aureus Oxidase - Streptococcus agalactiae + - Pseudomonas aeruginosa Enterobacteriaceae Lactose fermenter Escherichia coli Lactose non-fermenter Shigella sonnei Be able to work through a novel clinical case (with guidance) That includes lab work such as the primary plating media we used (BA, CA, MAC, CCNA), Gram stains, catalase/oxidase tests. Newly introduced techniques, such as how to do quantitative counts (urinary tract lab, also antimicrobial susceptibility testing). Unit Four – Key Concepts General considerations for using antimicrobials to treat infectious disease Know the characteristics of the antibiotics that we used in the last lab exercise. What drug family do they belong to, what is their site of action in a bacterial cell, etc. Know how to perform, read, and interpret a disk diffusion susceptibility assay and an MIC/MBC assay. Know the point of immunization. Know the pros and cons of live attenuated and inactivated vaccines.