Nonspecific Defenses
advertisement

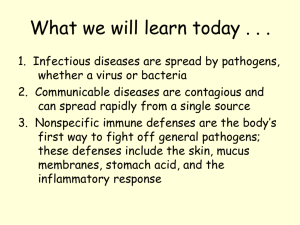
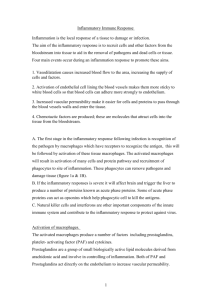
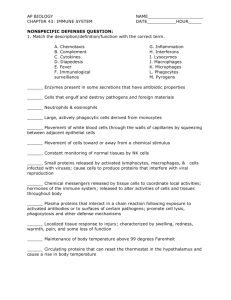
Nonspecific Defenses Adriana Perta Marisa Pawlowski Paige Simko Rachel Ragone Jill Ross Nonspecific Defenses • Occur automatically because they are innate • No memory is involved- no recognition that this same intruder has been attacked before • Barriers to entry, the inflammatory response, phagocytes and natural killer cells, and protective proteins are types of nonspecific defenses Immunity • The body’s capability to remove foreign substances and to kill pathogens and cancer cells • Involves both nonspecific defenses and specific defenses Barriers to Entry • Include nonchemical barriers such as the skin and the mucous membranes lining the respiratory, digestive, and urinary tracts; serve as mechanical barriers to entry by pathogens • Also include antimicrobial molecules (ex: oil gland secretions contain chemicals that weaken or kill certain bacteria on the skin) • The stomach has an acidic pH, which inhibits the growth of or kills many types of bacteria Inflammatory Response (refer to page 637 figure 35.3) • When tissue is damaged by physical or chemical agents or by pathogens, a series of events occur • An inflamed area has four outward signs: redness, heat, swelling, and pain • These signs are due to capillary changes in the damaged area • Histamine: a chemical signal, released by damaged tissue cells and mast cells • Mast cells: a type of white blood cell in tissues, cause capillaries to dilate and become more permeable • Some inflammatory responses trigger fever, the onset being controlled by the brain • The fever serves to inhibit the growth of some microorganisms, promotes accelerated tissue repair, stimulates immune cells to divide and increases the production of viral-fighting interferon Chronic Inflammation • One that persists for weeks or longer • Often treated by administering anti-inflammatory agents, such as aspirin, ibuprofen, or cortisone • These medications act against the chemical signals, such as histamines, that bring about an inflammation • Chronic inflammation is thought to play a role in many human illnesses • May lead to heart attacks, may destroy nerve cells in the brains of Alzheimer patients, can also be involved in the development of diabetes in obese individuals • Autoimmune diseases involve inflammation, but in these cases specific immunity seems to be the leading cause • A healthy diet, exercise, and good dental hygiene can reduce the occurrence of inflammation and help keep us well by reducing the occurrence of chronic inflammation Macrophages and Cytokines • Macrophages: in tissues, that devour many pathogens and survive • Have receptors that allow them to recognize the presence of pathogens • Release cytokines • Cytokines: chemical signals that stimulate other white cells such as neutrophils and monocytes, that then mature into macrophages Natural Killer Cells • Large, granular lymphocytes that kill virus-infected cells and cancer cells by cell-to-cell contact • Produce cytokines that stimulate these cells • Congregate in the tonsils, lymph nodes, and spleen • Look for a self protein on the body’s cell • Not specific; have no memory; and their numbers do not increase after stimulation occurs Protective Proteins (refer to page 638 figure 35.4) • Complement: composed of a number of blood plasma proteins • “complement” certain immune responses • Involved in the inflammatory response because certain complement proteins can bind to mast cells and trigger histamine release • Some combine to form a membrane attack complex that produces holes in the surface of bacteria and viruses • Interferons: proteins produced by virus-infected cells as a warning to noninfected cells in the area • Binds to receptors of noninfected cells, causing them to prepare for a possible attack • Used as treatment in certain viral infections like hepatitis C