The Immune System Power Point Lecture Click Here
advertisement

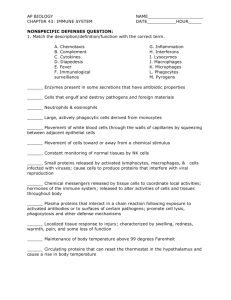
The Immune System An organisms’ protection from Pathogens Video Pathogen Any infectious agent that causes disease • Bacteria •Viruses •Fungi •Protists/parasites 2 Divisions of Immunity in Humans and Other Mammals I. Innate Immunity – “Non-Specific” This defense is not concerned with ‘what’ the pathogen is. This system merely prevents the pathogen from entering the body or destroys it before identifying it. It shoots first and asks questions later Innate Immunity involves several layers of defense: A. Barrier Defenses B. Inflammatory Response C. Cellular Defenses D. Natural Killer Cells E. Antimicrobial Defenses A. Barrier Defenses 1. 2. 3. 4. 5. Epidermis – impenetrable barrier Oil and Sweat have low pH Resident Flora – your own bacteria Mucous Membrane – mucus and cilia Lysozyme Skin Epidermis an impenetrable barrier to pathogens Oil and Sweat have a low pH that reduces pathogen growth Resident Flora your own colonies of bacteria that live on your skin out-competes with harmful bacteria for space Mucous Membranes Un-keritonized skin of the mocous membranes have a different layer of defense MUCUS and CILIA Lysozyme B. Cellular Defenses Microbes/antigens PHAGOCYTIC CELL Leukocytes – phagocytic white blood cells have surface Vacuole receptors that detect typical pathogen compounds called antigens. Lysosome containing enzymes EXTRACELLULAR Lipopolysaccharide FLUID Helper protein Groups of pathogens are recognized by TLR, Toll-like receptors TLR4 WHITE BLOOD CELL Flagellin TLR5 VESICLE CpG DNA TLR9 TLR3 Inflammatory responses A white blood cell engulfs a microbe, then fuses with a lysosome to destroy the microbe There are different types of phagocytic cells: Neutrophils engulf and destroy microbes Macrophages are part of the lymphatic system and are found throughout the body Eosinophils discharge destructive enzymes Dendritic cells stimulate development of acquired immunity Fig. 43-7 Interstitial fluid Adenoid Adenoid Tonsil Tonsil Blood Blood capillary capillary Lymph Lymph nodes nodes Spleen Spleen Peyer’s patches Peyer’s patches (small intestine) (small intestine) Appendix Appendix Lymphatic vessels Tissue Tissue cells cells Lymph Lymph node node Lymphatic Lymphatic vessel vessel Masses of Masses of defensive cells defensive cells C. Antimicrobial Proteins Peptides and proteins function in innate defense by attacking microbes directly or impeding their reproduction Interferon proteins provide innate defense against viruses and help activate macrophages About 30 proteins make up the complement system, which causes lysis of invading cells and helps trigger inflammation D. Inflammatory Responses Following an injury, mast cells release histamine, which promotes changes in blood vessels; this is part of the inflammatory response These changes increase local blood supply and allow more phagocytes and antimicrobial proteins to enter tissues Pus, a fluid rich in white blood cells, dead microbes, and cell debris, accumulates at the site of inflammation Fig. 43-8-3 D. Inflammatory Responses Pathogen Mast cell Splinter Chemical Macrophage Signals (Ligand) Capillary Red blood cells Phagocytic cell Fluid Phagocytosis Fever is a systemic inflammatory response triggered by pyrogens released by macrophages, and toxins from pathogens Septic shock is a life-threatening condition caused by an overwhelming inflammatory response II. Acquired immunity lymphocyte receptors provide pathogen-specific recognition Lymphocytes- are white blood cells that recognize and respond to antigens, foreign molecules. Lymphocytes that mature in the thymus above the heart are called T cells, and those that mature in bone marrow are called B cells Lymphocytes have immunological memory. Fig. 43-9 B cells and T cells have receptor proteins that can recognize and bind to antigens Antigenbinding site Antigenbinding site Antigenbinding site Plasma membrane B cell (a) B cell receptor Cytoplasm of B cell Cytoplasm of T cell (b) T cell receptor T cell Antibody Genes V V Heavy chain V D D J J J J C Gene components scattered through one chromosome Light chain V D J C Rearranged gene components encoding a heavy chain Antigenbinding region Constant region Assembled antibody molecule Markers of Self: Major Histocompatibility Complex Viral infection Antigenic peptide Antigenic peptide Antigenic peptide MHC Class I MHC Class I MHC Class II Antigen-presenting cell uses MHC Class I or II Infected cell Cell membrane Body Cell with “Self-Markers called MHC B Cells Antigen-specific B cell receptor Class II MHC and processed antigen are displayed Antigen B cell bacteria Antibodies (Immunoglobins) Cytokines (Lymphokines) Plasma cell LIGAND Activated helper T cell T Cells Resting helper T cell Resting cytotoxic T cell Activated when they encounter infected cells that are presenting antigens Cytokines Released by Helper T-Cells Granule w/ destructive enzymes Activated helper T cell Activated killer cell Killer Cells: Cytotoxic Ts Killer cell Surface contact Target cell Target-oriented granules T cells bind to antigen fragments presented on a host cell These antigen fragments are bound to cell-surface proteins called MHC molecules MHC molecules are so named because they are encoded by a family of genes called the major histocompatibility complex The Role of the MHC In infected cells, MHC molecules bind and transport antigen fragments to the cell surface, a process called antigen presentation A nearby T cell can then detect the antigen fragment displayed on the cell’s surface Depending on their source, peptide antigens are handled by different classes of MHC molecules Fig. 43-12 Infected cell Microbe Antigenpresenting cell 1 Antigen associates with MHC molecule Antigen fragment Antigen fragment 1 1 Class I MHC molecule T cell receptor (a) 2 2 Cytotoxic T cell Class II MHC molecule T cell receptor 2 T cell recognizes combination (b) Helper T cell Activation of B Cells to Make Antibody Circulating antibody Antigen Antigen-specific B cell receptor Antigen Class II MHC B cell Antigenpresenting cell Antigen is processed Class II MHC Antigen-presenting cell and processed antigen are displayed Cytokines (LIGAND) Activated helper T cell Antibodies Plasma cell Fig. 43-14 Antigen molecules B cells that differ in antigen specificity Antigen receptor Animation: Role of B Cells Antibody molecules Clone of memory B cells Clone of plasma cells Fig. 43-16 Humoral (antibody-mediated) immune response Cell-mediated immune response Key Antigen (1st exposure) + Engulfed by Gives rise to Antigenpresenting cell + Stimulates + + B cell Helper T cell + Cytotoxic T cell + Memory Helper T cells + + + Antigen (2nd exposure) Plasma cells Memory B cells + Memory Cytotoxic T cells Active Cytotoxic T cells Secreted antibodies Defend against extracellular pathogens by binding to antigens, thereby neutralizing pathogens or making them better targets for phagocytes and complement proteins. Defend against intracellular pathogens and cancer by binding to and lysing the infected cells or cancer cells. Fig. 43-17 Antigenpresenting cell Peptide antigen Bacterium Class II MHC molecule CD4 TCR (T cell receptor) Cytokines Helper T cell Humoral immunity (secretion of antibodies by plasma cells) + + + B cell + Cytokines Cytotoxic T cell Animation: Helper T Cells Cell-mediated immunity (attack on infected cells) Cytotoxic T Cells: A Response to Infected Cells Cytotoxic T cells are the effector cells in cell-mediated immune response The activated cytotoxic T cell secretes proteins that destroy the infected target cell Animation: Cytotoxic T Cells Fig. 43-18-3 Released cytotoxic T cell Cytotoxic T cell Perforin Granzymes CD8 TCR Class I MHC molecule Target cell perforin granzymes Pore Peptide antigen Dying target cell B Cells: A Response to Extracellular Pathogens The humoral response is characterized by secretion of antibodies by B cells Activation of B cells is aided by cytokines and antigen binding to helper T cells Clonal selection of B cells generates antibody-secreting plasma cells, the effector cells of humoral immunity Fig. 43-19 Antigen-presenting cell Bacterium Peptide antigen Class II MHC molecule TCR CD4 B cell + Cytokines Clone of plasma cells Secreted antibody molecules Endoplasmic reticulum of plasma cell Helper T cell Activated helper T cell Clone of memory B cells 2 µm The Role of Antibodies in Immunity Neutralization occurs when a pathogen can no longer infect a host because it is bound to an antibody Opsonization occurs when antibodies bound to antigens increase phagocytosis Antibodies together with proteins of the complement system generate a membrane attack complex and cell lysis Animation: Antibodies Fig. 43-21 Viral neutralization Virus Opsonization Activation of complement system and pore formation Bacterium Antibodies bound to antigens on viruses can neutralize the virus Complement proteins Macrophage Binding of antibodies toFormation bacteria of membrane Promotes phagocytosisattack of the complex Bactria by Macrophages Flow of water and ions Pore Foreign cell Following activation the attack complex forms poresof in antibodies the foreigntocell’s Binding antigens on the membrane water and ions to surface ,ofallowing a foreign cell activates a rushcomplex in. system. The Cell swells and eventually lyses. Evolution and Immunity VIDEO 1 VIDEO 2