Infectious Disease Epidemiology
advertisement

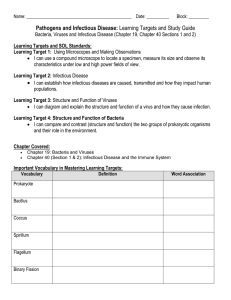
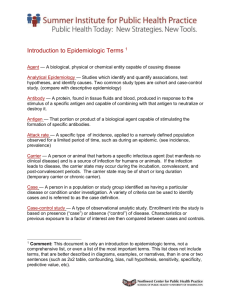
Infectious Disease Epidemiology Casey E. Barton, M.S. July 26, 2001 REMINDERS!!!!!!!!!! TODAY by 5pm – Submit all outstanding homeworks and redos July 31st – Teaching-Learning Exam – Course Evaluations – Tutorial after class August 2nd – FINAL EXAM – Last day of class!!!!!!! Top 10 Reported Infectious Diseases 1999 USA Chlamydia Gonorrhea AIDS Salmonellosis Hepatitis A Shigellosis Tuberculosis Lyme Disease Hepatitis B Syphilis TEXAS Chlamydia Gonorrhea Chickenpox HIV AIDS Hepatitis A Shigellosis Salmonellosis Tuberculosis Campylobacteriosis Epidemiologic Triangle HOST AGENT ENVIRONMENT AGENTS An Agent MUST be present for an infectious disease to develop Epidemiologists describe: – Frequency of disease – Mechanisms of transmission – The causal agent AGENTS Bacteria Viruses and rickettsia Mycoses (fungi) Parasites – Protozoa – Helminths Arthropods AGENTS: Bacteria Leading killers in 19th century Examples: – Tuberculosis – Salmonellosis – Streptococcal infections Problem: emerging bacteria strains resistant to current antibiotics AGENTS: Viruses and Rickettsia Viral infection include: – Hepatitis A – Herpes simplex – Influenza – HIV Rickettsial infections include: – Q fever – Rocky Mountain Spotted Fever Mycoses (Fungi) Examples: – Ringworm – Aspergillosis – Candidiasis AGENTS: Parasites Protozoa – – – – Malaria Cyclosporiasis Giardiosis Chagas’ Disease Helminths (worms) – Tapeworms – Roundworms – Schistosomiasis AGENTS: Arthropods Insect vectors including: – – – – – Mosquitoes Ticks Flies Mites Other insects Arthropod-borne diseases include: – – – – RMSF Malaria Encephalitis Lyme Disease Modes of Transmission Airborne or Contact Food- and Water-borne Blood-borne Sexually Transmitted Arthropod-borne Zoonotic Means of Transmission Portal of Exit Mode of transmission Portal of Entry Example of Disease Respiratory secretions Airborne droplets Respiratory tract Common cold, measles Feces Water, food, flies Alimentary tract Parasites, Typhoid Lesions, exudate Direct contact, sexual contact Skin, genital membranes Chlamydia, gonorrhea Conjunctival exudate Fomites, flies Ocular mucous membranes Trachoma (blindness) Blood Blood-sucking arthropods, transfusions skin Malaria, Encephalitis Means of Transmission Direct: person to person Indirect: through intermediate sources such as vehicles, fomites or vectors Horizontal: transmission from one person to another (direct or indirect) Vertical: mother to fetus either genetic or across placenta Characteristics of Infectious Disease Agents Infectivity Pathogenicity Virulence Toxigenicity Resistance Antigenicity Infectivity Capacity of the agent to enter and multiply in a susceptible host and thus produce infection or disease Examples: measles and polio Measure of Infectivity: Secondary Attack Rate (SAR%) Pathogenicity Capacity of the agent to cause disease in the infected host Example: measles Measure of pathogenicity: proportion of individuals with clinically apparent disease Virulence Severity of the disease – i.e. whether clinical manifestations are produced Example: Rabies Measure of Virulence: Case Fatality Rate (CFR) Toxigenicity Capacity of the agent to product a toxin or poison Examples: botulism and shellfish poisoning Disease is caused by toxins produced by the agent, rather than by the actual agent Resistance Ability of the agent to survive adverse environmental conditions Examples: parasite with spores or cysts, Hepatitis virus Resistance is also applied to the HOST Antigenicity Ability of the agent to induce antibody production in the host Agents may or may not induce longterm immunity – Examples: Measles re-infection is rare Immunogenicity – Related term – refers to an infection’s ability to produce specific immunity Host Subclinical infection Active Disease Host’s ability to fight off infectious agent – Nonspecific defense mechanisms – Disease-specific defense mechanisms HOST: Non-specific defense mechanisms Age, Sex, Race, Genetics Religion, Customs, Occupation, Nutritional status Skin, Mucosal surfaces, Saliva, High pH of gastric juices Immune system (phagocytes and macrophages) HOST: Disease-specific defense mechanisms Immunity: resistance of host to an agent Active: all or part of organism invokes an immunologic response – Natural: results from an infection – Artificial: results from immunization Passive: preformed antibody invokes short term immunity – Natural: antibodies cross the placenta – Artificial: immuneglobulin after certain exposures ENVIRONMENT Physical: weather, temperature, humidity, geologic formations, habitat Biological: population density, flora, fauna, reservoirs Socioeconomical: behavioral, personality, attitudinal, and cultural characteristics of a group of people Endemic vs.Epidemic Endemic: constant presence of a disease or agent in a defined geographical area Epidemic: excessive occurrence of disease (above endemic level) in a defined geographical area – 2 Types: • Common Source • Propogated Source Epidemic Common Source Epidemic: event or exposure comes from a single source that all persons in the group had a chance to encounter Propogated Epidemic: caused by either direct or indirect transmission of infectious disease from one individual to another and can have multiple sources from which disease can be transmitted Endemic versus Epidemic ENDEMIC Point EPIDEMIC Propagating EPIDEMIC NOTE: X axis = Time; Y axis = # new cases Reservoir (Niche) Fosters survival of infectious disease agent Types of reservoirs – Human – Plant – Animal – Arthropod – Physical environment Inapparent infection Subclinical infection: absence of clinically obvious signs and symptoms Asymptomatic individuals can transmit disease Carrier status Serologic evidence of infection Incubation Period Time interval between exposure to an infectious agent and the appearance of the first signs of disease During this time, the infectious agent replicates within the host Can be hours, days, weeks, or years Applies only to clinically apparent cases of disease Generation Time Time between lodgment of an infectious agent in a host and the maximal communicability of the host May or may not be equivalent to incubation period Applies to both clinically apparent and inapparent cases of disease Utilized for describing the spread of infectious agents that have a large proportion of subclinical cases Herd Immunity A population may become immune to an infectious agent after a large proportion of individuals have become immune – i.e. through past infections or vaccination Can occur when immune persons prevent the spread of disease to unimmunized individuals and confers protection to the population even though not every single individual has been immunized Effect of Herd Immunity on Spread of Infection (from Jekel et al. 1996, p. 12) - + + - + + + + + + - - - + + + + + + + + + - - - - Absence of Herd Immunity Presence of 50% Herd Immunity + Iceberg Concept of Disease Death Visible Cases Invisible Cases Clinical illness Asymptomatic cases Carriers Zoonoses World Health Organization (WHO): – diseases and infections which are naturally transmitted between vertebrate animals and man – Examples: Rabies, roundworms, Lyme disease, Brucellosis, Cryptosporidiosis Epizootic and enzootic but refers to diseases in animals Emerging Infectious Diseases Changes in climate – global warming Human activities – farming, reforestation Technologic changes – air travel, organ transplantation Demographic changes – migration to cities Host Prevention Immunity – immunizations Behavioral change Treatment of contact and carriers screening Control Environmental – Personal hygiene – Food protection and safety – Water supplies – Sanitation, regulation Vectors – Mosquitoes, insecticides – Animal population control Measures of Disease Outbreaks Attack Rate Secondary Attack Rate Case Fatality Rate Attack Rate Type of incidence rate AR% = # Ill___ * 100 during a time period # Ill + # Well Can calculate food or exposure specific AR% Secondary Attack Rate Yields an index of the spread of disease within a circumscribed unit, i.e. household, dorm Index case: case that first comes to the attention of public health authorities SAR% = # new cases in group – initial cases * 100 # susceptible persons in group – initial cases Case-Fatality Rate Refers to the number of deaths caused by a specific disease among those who have the disease Provides index of deadliness of a particular disease within a specific population CFR% = # deaths due to disease X * 100 # cases disease X DIFFERENT than crude death rate Centers for Disease Control and Prevention (CDC) National Center for HIV,STD, and TB Prevention National Center for Infectious Diseases – – – – – AIDS, STD and TB Laboratory Research Division of Bacterial and Mycotic Diseases Division of Parasitic Diseases Division of Vector-borne Infectious Diseases Division of Viral and Rickettsial Diseases National Immunization Program Infectious Disease Information Emerging Infectious Diseases Journal – www.cdc.gov/ncidod/eid/ Morbidity and Mortality Weekly Report (MMWR) – www.cdc.gov/mmwr/ Program for monitoring Emerging Diseases (Promed) – www.promedmail.org/pls/promed/promed.home THE END!!! EXAMPLE CALCULATIONS ATE Food DID NOT EAT Ill Well Tot Ill Well Tot Chicken 32 8 40 20 40 60 Shrimp 40 30 70 10 20 30 Ice Cream 48 12 60 2 40 38 Which food item appears to be the most probable vehicle for the food-borne infection assocaited with illness at this picnic?