Composition of Blood
advertisement

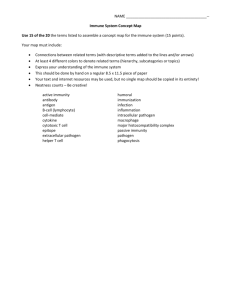
Blood • Blood accounts for approximately 8% of body weight • The pH of blood is 7.35–7.45 • Temperature is 38C, slightly higher than “normal” body temperature • Average volume of blood is 5–6 L for males, and 4–5 L for females • RBC circulate for approximately 4 months. Functions of Circulatory System • Transport – O2, CO2, nutrients, wastes, hormones, and heat • Protection – WBCs, antibodies, and platelets • Regulation fluid volume in the circulatory system • When the blood has a high osmolarity water will leave the tissues and go into blood. – This is why excessive consumption of certain electrolytes raises BP – low osmolarity • When blood has a low osmolarity excessive fluid follows an osmotic gradient into the tissues which may result in edema Erythrocytes (RBCs) • Biconcave discs, anucleate, essentially no organelles • Filled with hemoglobin (Hb) – a protein that functions in gas transport • Contain the plasma membrane protein spectrin and other proteins that: – Give erythrocytes their flexibility – Allow them to change shape as necessary Production of Erythrocytes • Hematopoiesis – blood cell formation • Hematopoiesis occurs in the red bone marrow of the: – Axial skeleton and girdles – Epiphyses of the humerus and femur • Hemocytoblasts give rise to all formed elements Bone Marrow in an Adult Hemopoiesis Hormonal Control of Erythropoiesis • Chemoreceptors in the kidneys detect a decrease in P02 – They respond by secreting the hormone Erythropoietin. (EPO) • (EPO) is triggered by: – Hypoxia( low oxygen levels) due to decreased RBCs • anemia – Decreased oxygen availability • High altitude, pulmonary infections – Increased tissue demand for oxygen • exercise • Erythropoesis increases the: – RBC count in circulating blood – Oxygen carrying ability of the blood Erythropoietin Mechanism Start Normal blood oxygen levels Increases O2-carrying ability of blood Stimulus: Hypoxia due to decreased RBC count, decreased availability of O2 to blood, or increased tissue demands for O2 Reduces O2 levels in blood Enhanced erythropoiesis increases RBC count Erythropoietin stimulates red bone marrow Kidney (and liver to a smaller extent) releases erythropoietin Erythrocyte Disorders • Polycythemia - an excess of RBCs – primary polycythemia (Polycythemia Vera ) • cancers of erythropoietic cell line in red bone marrow – secondary polycythemia (ENVIORMENTAL) • from dehydration, emphysema, high altitude, or physical conditioning and blood doping • Dangers of polycythemia – increased RBC’s will result in increases in: • blood volume (water following their osmotic gradient) • Viscosity (stickiness ,thicker) heart works harder greater resistance • Blood pressure (Both increases in vessel resistance and volume will increase the pressure in the vessel. – can lead to embolism, stroke or heart failure Diagnostic Value In Examining RBCs • Diabetes: Chronically elevated BGLs will increase glycosylated hemoglobin ( A1c). – This reflects average BGL over the several months. • Essential fatty acid composition: Looks at composition of fatty acids that make up cell membranes. – Low omega 3 and high omega 6 and saturated fatty acids predispose you to inflammation and disease. • Magnesium levels: measures mag levels inside the RBCs opposed to just looking at serum levels. – Signs and symptoms of magnesium deficiency include fatigue, weakness, heart disturbances, mental confusion, muscle cramps, loss of appetite, and insomnia. Leukocytes (WBCs) • Leukocytes, the only blood cells that are considered complete cells: – Are less numerous than RBCs and only make up 1% of the total blood volume • 1/750 ratio to RBC • ( Buffy white coat) – Can leave capillaries via diapedesis and move through tissue spaces in response to bacterial or viral invasion Leukopoiesis Fig. 18.18 Platelets • Small fragments of megakaryocyte cytoplasm – Normal Count - 130,000 to 400,000 platelets/L • Functions – secrete clotting factors and growth factors for vessel repair – initiate formation of clot-dissolving enzyme – phagocytize bacteria – chemically attract neutrophils and monocytes to sites of inflammation Genesis of Platelets • The stem cell for platelets is the hemocytoblast • The sequential developmental pathway from hemocytoblast to megakaryocytes. • These cells produce platelets by – Pieces of cytoplasm splits off (cell fragments) that enter bloodstream as platelets (live for 10 days) – some stored in spleen Hemostasis • Normally blood will flow smoothly though an intact artery. If there is a disruption in the endothelium; hemorrhaging may result. The artery will protect itself through a process called hemostasis. – It involves 3 major phases Hemostasis - Vascular Spasm • The initial response of the damaged blood vessel is to constrict preventing additional blood lose. • This is accomplished through activation of: • pain receptors : directly innervate constrictors. • • smooth muscle injury results in reflexive spasm platelets release serotonin (vasoconstrictor) Hemostasis -Platelet Plug Formation • Platelet plug formation: • broken vessel exposes collagen which attracts platelets • Platelets form pseudopods enabling them stick to damaged vessel. Platelets produce releasing a variety of substances • serotonin is a vasoconstrictor • ADP attracts more platelets (positive feedback) Hemostasis - Coagulation • Clotting - most effective defense against bleeding – Procoagulants (clotting factors) are present in plasma undergo series of biochemical reactions. – activate one factor and it will activate the next to form a reaction cascade. • Extrinsic pathway : initiated by damaged tissues • Intrinsic pathway: platelet plug produces clotting factors. • Both pathways lead to the production of factor X – The final result is conversion of fibrinogen into fibrin Coagulation Pathways • Extrinsic pathway – initiated by tissue thromboplastin • Intrinsic pathway – initiated by factor XII – Both produce factor X which leads to: • Prothrombin activator: converts of fibrinogen to Fibrin • Clotting requires many steps to ensure clots don’t happen without cause. Hemostasis Disorders: Bleeding Disorders • Thrombocytopenia – condition where the number of circulating platelets is deficient. – Patients show petechiae (small purple blotches on the skin) due to spontaneous, widespread hemorrhage. – Caused by suppression or destruction of bone marrow (e.g., malignancy, radiation) – Platelet counts less than 50,000/mm3 is diagnostic for this condition. – Treated with whole blood transfusions. • Hemophilia – Genetic lack of any clotting factor affects coagulation Coagulation Disorders • What effect does stress have on platelet aggregation? – Epinephrine increases likely of forming clots by making the platelets more sticky. • Thrombosis - abnormal clotting in unbroken vessel which will narrow the lumen for blood to flow . – most likely to occur in leg veins of inactive people because stagnant blood tends to form clots. – The formation of a dangerous thrombi can block circulation resulting in tissue death – Coronary thrombosis – thrombus in blood vessel of the heart • Embolism – The thrombus over time can break of and travel throughout the in a vessel until it gets stuck. – Infarction may occur if clot blocks blood supply to an organ (MI or stroke) – pulmonary embolism - clot may break free, travel from veins to lungs – Cerebral emboli results in CVA (cerebral vascular accidents) stroke. Lymphatic System • Immunity – fluids from all capillary beds are filtered – immune cells stand ready to respond to foreign cells or chemicals encountered • Lipid absorption – Lacteals in small intestine absorb dietary lipids • Fluid recovery – absorbs plasma proteins and fluid (2 to 4 L/day) from tissues and returns it to the bloodstream • interference with lymphatic drainage leads to severe edema Lymphatic System Immunity: Two Intrinsic Defense Systems • • • The function of the immune system is to protect the body from pathogens. It is composed of 2 major divisions Innate (nonspecific) 1. • The body’s first line of defense system consists of: • intact skin and mucosa 2. The inflammation process 3. Macrophages such as monocytes which phagocytose foreign invaders. 4. NK cells. The bodies nonspecific assassins Acquired (specific) system – Following ingestion of a pathogen by a macrophage lymphocytes become sensitive to that specific pathogens • • – – B-lymphocytes function in the body fluid such as blood T lymphocytes work in infected cells. takes longer to react than the innate system this system has memory Mechanism of Phagocytosis Innate Immunity Inflammation: Tissue Response to Injury • The inflammatory response is triggered whenever body tissues are injured – Prevents the spread of damaging agents to nearby tissues – Disposes of cell debris and pathogens – Sets the stage for repair processes • The four cardinal signs of acute inflammation are redness, heat, swelling, and pain Inflammatory Response: Phagocytic Mobilization 4 Positive chemotaxis 1 Neutrophils enter blood from bone marrow Capillary wall Inflammatory chemicals diffusing from the inflamed site act as chemotactic agents 3 Diapedesis 2 Margination Endothelium Basal lamina Natural Killer (NK) Cells • They are considered part of the non specific immune system • Natural killer cells: – Are a small, distinct group of large granular lymphocytes – React nonspecifically and eliminate cancerous and virus-infected cells – Kill their target cells by releasing perforins and other cytolytic (cell- lysing) chemicals – Secrete potent chemicals that enhance the inflammatory response Adaptive Immune Defenses • The adaptive immune system is antigen-specific, systemic and has memory. The adaptive (specific) immune system: – Recognizes specific foreign substances (Antigens) : • Substances that can mobilize the immune system and provoke an immune response – This the body sees as foreign (bad) – Acts to immobilize, neutralize, or destroy these antigens – Amplifies inflammatory response and activates complement • It has two separate but overlapping arms of defense. – Humoral, or antibody-mediated immunity • B lymphocytes – oversee humoral immunity • Extracellular (antigens)pathogens bacteria – Cellular, or cell-mediated immunity • T lymphocytes – non-antibody-producing cells that constitute the cell-mediated arm of immunity • intracellular antigens such viruses and cancer Lymphocytes • Immature lymphocytes released from bone marrow are essentially identical • Whether a lymphocyte matures into a B cell or a T cell depends on where in the body it becomes Immunocompetent (Functional) – B cells mature in the bone marrow • Humoral division – T cells mature in the thymus • Cellular division Major Types of T Cells Cell-Mediated Immune Response • Since antibodies are useless against intracellular antigens, cell-mediated immunity is needed • Two major populations of T cells mediate cellular immunity – CD4 cells (T4 cells) are primarily helper T cells (TH) – CD8 cells (T8 cells) are cytotoxic T cells (TC) that destroy cells harboring foreign antigens • Other types of T cells are: – Suppressor T cells (TS) Turn down immune response once threat is over. – Memory T cells : reduce response time of future attacks. Antigen Presenting Cell • Once a macrophage has eaten an antigen it becomes an Antigen-presenting cells (APCs): – Do not respond to specific antigens – They present antigen to TH-cell which alerts both B and T cells of the specific antigen. Helper T Cells (TH) • Regulatory cells that play a central role in the immune response • Once primed by APC presentation of antigen, they: – Chemically or directly stimulate proliferation of other T cells – Stimulate B cells that have already become bound to antigen • Without TH, there is no immune response – AIDS cripples the immune system by effecting the # of TH cells. Role of Helper T Cells • Secretes interleukins (chemical messages between cells to mobilize the response!) – attract neutrophils, NK cells, macrophages • stimulate phagocytosis – stimulate T and B cell mitosis and maturation • Coordinate humoral and cellular immunity Cytotoxic T Cell (Tc) • TC cells, or killer T cells, are the only T cells that can directly attack and kill other cells • They circulate throughout the body in search of body cells that display the antigen to which they have been sensitized • Their targets include: – – – – Virus-infected cells Cells with intracellular bacteria or parasites Cancer cells Foreign cells from blood transfusions or transplants Mechanisms of Tc Action • TC cells: – Bind to the target cell and release perforins into its membrane • perforin causes cell lysis Humoral Response • The B-cells produce soluble antibodies that interact in extracellular environments such as: – – – – body secretions tissue fluid blood lymph • Antibodies surround and incapacitate the antigens by – Preventing viruses from entering the cell – Neutralize release of endotoxins from bacteria – Surrounds antigens allowing phagocyte time to engulf them. Clonal Selection Humoral Immunity • B-cells are presented with an antigen directly or by Thelper cell • This activated clone B-cells with a specific antigen receptor to identify the specific antigen • The clones produce plasma cells which will produce the antibodies specific for that antigen. • Antigen will become surrounded by antibodies disabling it allowing for a phagocyte to come and finish it off. • Some B-Cells will become memory B-Cells which circulate until the next time the body is presented with that antigen. – This is why the body responds faster the next time you are exposed Summary of the Primary Immune Response Blood And Immunity Screen • • • • • • • • • • • • Skin color changes Shortness of breath Blood pressure changes Dizziness Body weight changes Easy bruising, bleeding Sensory changes in hands and feet Swollen lymph nodes Fever Changes in heart rate Autonomic dysfunction Anemia (sickle cell ) • Leukemia hx of blood transfusions.