THE BLOOD: key words and concepts
advertisement

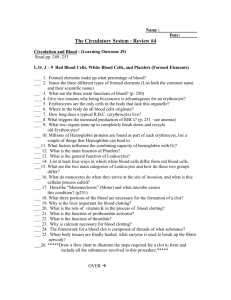
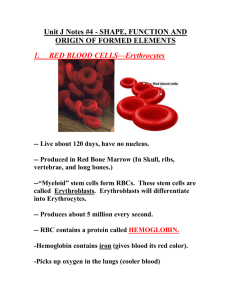
THE BLOOD: key words and concepts Plasma Formed elements Erythrocytes (RBC) Leukocytes (WBC) Lymphocytes Monocytes Granulocytes neutrophils eosinophils basophils Platelets Hemoglobin o2 CO2 Hematocrit Anemia Carbonic anhydrase Bicarbonate H CO3Hematopoietic stem cells HEMATOCYTOBLAST Proerythroblast, Myeloblast, Lymphoblast, Monoblast, Megakaryoblast Erythropoiesis, Erythropoietin Blood - more key words Hemostasis Coagulation Plasma: Antibodies H2O, solutes, Proteins: Albumins, Globulins, Clotting factors: Fibrinogen fibrin Prothrombin thrombin Extrinsic, intrinsic clotting pathways ‘Clotting cascade’ Fibrinolysis: clot dissolution Plasminogen Plasmin Antigens ABO, RH blood types Agglutination Type and cross-match Transfusion Hemolysis COMPOSITION OF BLOOD Blood Composed of plasma and formed elements (55%) (45%) Complex transport medium --performs vital pickup and delivery services for the body WORKING WITH THE MUSCLES AND SKIN -Blood is the key to the heat-regulating mechanism of the body Blood volume Young adult male has approximately 5-6 L of blood, female 4-5 Liters occupying the CARDIOVASCULAR SYSTEM (IN THE INTRAVASCULAR SPACE) A UNIT of donated whole blood = .5 liter Composition of Whole Blood FORMED ELEMENTS OF BLOOD Red blood cells (RBCs), also called ERYTHROCYTES Most numerous of the formed elements no nucleus -- shaped like tiny biconcave disks also do not contain ribosomes, mitochondria, et al. PRIMARY COMPONENT IS HEMOGLOBIN Function of RBCs TRANSPORT OF OXYGEN AND CARBON DIOXIDE depends on hemoglobin Carbonic anhydrase: enzyme in RBCs that catalyzes a reaction that joins carbon dioxide and water to form carbonic acid Carbonic acid: dissociates and GENERATES BICARBONATE IONS, which diffuse out of the RBC and TRANSPORT CARBON DIOXIDE IN THE BLOOD PLASMA (as H2CO3-) Hemoglobin Within each RBC are approximately 200 to 300 million molecules of hemoglobin HEMOGLOBIN IS COMPOSED OF FOUR GLOBIN CHAINS, EACH ATTACHED TO A HEME (iron) GROUP Hemoglobin is able to unite with four oxygen molecules to form oxyhemoglobin to allow RBCs to transport oxygen where it is needed ANEMIA: a decrease in the number or volume of functional RBCs in a given unit of whole blood, (which means there is a decreased level of HEMOGLOBIN) Formation of RBCs, cells & other blood ERYTHROPOIESIS: the process of RBC formation Formation begins in the red bone marrow as HEMATOPOIETIC STEM CELLS and goes through several stages of development to become erythrocytes; entire maturation process requires approximately 4 days. Once in the bloodstream, RBC lifespan is around 120 days (4 months) Anemia, Erythropoietin, AN-EMIA literally, ‘no blood’ -- actually means ‘too little blood’ either decreased numbers of RBC’s, or RBC’s with decreased levels of HGB in them nml male: Hgb is 14-16 gm/dl nml female Hgb is 12-14 gm/dl there are many possible causes for anemia If Erythropoiesis is the formation of Blood, then what does the Hormone Erythropoietin do? Stimulates RBC production ERYTHROPOIETIN (EPO) is a hormone that is produced in the kidneys. Produced by the kidneys when specialized cells in the kidneys sense oxygen level in the body's tissues is low. THIS HORMONE STIMULATES THE PRODUCTION OF RED BLOOD CELLS IN THE BONE MARROW. When introduced synthetically by injection, erythropoietin can help treat anemia by boosting the number of red blood cells in the body. Injections might be required because the kidneys are not producing enough erythropoietin on their own or when a patient is experiencing severe anemia. The hematopoietic STEM cell, the Hemocytoblast White blood cells (WBCs), also called leukocytes Granulocytes: NEUTROPHILS: approx. 65% of total WBC count in a normal blood sample; highly mobile and active PHAGOCYTIC CELLS; capable of diapedesis ;cytoplasmic granules contain lysosomes. ELEVATED #’s during ACUTE MICROBIAL INFECTIONS EOSINOPHILS: 2% to 5% of circulating WBCs; numerous in lining of respiratory and digestive tracts;; provide protection against infections caused by parasitic worms and are increased in ALLERGIC REACTIONS Basophils: only 0.5% to 1% of circulating WBCs; motile and capable of diapedesis; cytoplasmic granules contain histamine and heparin (mediators of INFLAMMATION) Neutrophil, (PMN) Eosinophil Basophil) Agranulocytes –Lymphocytes, Monocytes LYMPHOCYTES: the smallest leukocytes T lymphocytes and B lymphocytes have an important role in immunity: T LYMPHOCYTES directly attack an infected or cancerous cell, B LYMPHOCYTES produce antibodies against specific antigens MONOCYTES: largest leukocytes; mobile and highly phagocytic cells WBC numbers: 1 mm3 of normal blood usually contains 5000 to 9000 leukocytes, with diffnt % for each type; WBC numbers have clinical significance because they change with certain abnormal conditions. *** In general, WBC goes up in : INFECTION and INFLAMMATION *** White Blood Cell Count: WBC numbers: 1 mm3 of normal blood usually contains 5,000 to 9,000 leukocytes, with diffnt % for each type; WBC numbers have clinical significance because they change with certain abnormal conditions. *** In general, WBC goes up in : INFECTION and INFLAMMATION *** FORMED ELEMENTS OF BLOOD (cont.) Formation of WBCs Granular and agranular leukocytes mature from the undifferentiated hematopoietic stem cell Neutrophils, eosinophils, basophils, and a few lymphocytes and monocytes originate in red bone marrow; most lymphocytes and monocytes develop from hematopoietic stem cells in lymphatic tissue FORMED ELEMENTS OF BLOOD (cont.) Structure In circulating blood, platelets are small, pale bodies that appear as irregular spindles or oval disks Three important properties are agglutination, adhesiveness, and aggregation Platelet counts in adults average 250,000/mm3 of blood; normal range is 150,000 to 400,000/mm3 FORMED ELEMENTS OF BLOOD (cont.) Functions of platelets Important role in hemostasis and blood coagulation; secondary role in defending against bacterial attacks Hemostasis: refers to stoppage of blood flow; however, if injury is extensive, the blood-clotting mechanism is activated to assist FORMED ELEMENTS OF BLOOD (cont.) Platelet plug formation One to five seconds after injury to vessel wall, platelets adhere to damaged endothelial lining and to each other, forming a platelet plug Temporary platelet plug is an important step in hemostasis Normal platelets (positive charge) adhere to damaged capillary wall and underlying collagen fibers, both of which have a negative charge “Sticky platelets” form physical plug and secrete several chemicals involved in the coagulation process Formation and life span of platelets (7 to 10 days): formed in red bone marrow, lungs, and spleen by fragmentation of megakaryocytes BLOOD TYPES: BLOOD GROUPS The ABO system Every person’s blood belongs to one of four ABO blood groups Named for antigens on RBC membranes Type A: antigen A on RBCs Type B: antigen B on RBCs Type AB: both antigens A and B on RBCs; known as universal recipient Type O: neither antigen A nor B on RBCs; known as universal donor BLOOD TYPES: BLOOD GROUPS (cont.) The Rh system Rh-positive: Rh antigen is present on the RBCs Rh-negative: RBCs have no Rh antigen present Anti-Rh antibodies are not normally present in blood; anti-Rh antibodies can appear in Rh-negative blood if it has come in contact with Rh-positive RBCs BLOOD PLASMA Plasma: liquid part of blood; clear, straw-colored fluid; composed of 90% water and 10% solutes (Figure 17-20) Solutes: 6% to 8% of plasma solutes are proteins, consisting of three main compounds Albumins: help maintain osmotic balance of the blood Globulins: essential component of the immunity mechanism Fibrinogen: key role in blood clotting Plasma proteins have an essential role in maintaining normal blood circulation BLOOD CLOTTING: COAGULATION Mechanism of blood clotting: goal of coagulation is to stop bleeding and prevent loss of vital body fluid in a swift and sure method Classic theory of coagulation advanced in 1905 Identified four components critical to coagulation Prothrombin Thrombin Fibrinogen Fibrin BLOOD CLOTTING: COAGULATION (cont.) Current explanation of coagulation involves three stages Stage 1: production of thromboplastin activator by either of the following: Chemicals released from damaged tissues (extrinsic pathway) Chemicals present in the blood (intrinsic pathway) Stage 2: conversion of prothrombin to thrombin Stage 3: conversion of fibrinogen to fibrin and production of fibrin clot BLOOD CLOTTING: COAGULATION (cont.) Conditions that oppose clotting Clot formation in intact vessels is opposed Several factors oppose clotting Perfectly smooth surface of the normal endothelial lining of blood vessels does not allow platelets to adhere Antithrombins: substances in the blood that oppose or inactivate thrombin; prevent thrombin from converting fibrinogen to fibrin (e.g., heparin) BLOOD CLOTTING: COAGULATION (cont.) Conditions that hasten clotting Rough spot in the endothelium Abnormally slow blood flow Clot dissolution Fibrinolysis: physiological mechanism that dissolves Fibrinolysin: enzyme in the blood that catalyzes the hydrolysis of fibrin, causing it to dissolve Additional factors are presumed to aid clot dissolution (e.g., substances that activate profibrinolysin) THE BIG PICTURE: BLOOD AND THE WHOLE BODY Blood plasma transports substances, including heat, around the body, linking all body tissues together Substances can be transported between almost any two points in the body Blood tissue contains formed elements—blood cells and platelets RBCs assist in the transport of oxygen and carbon dioxide WBCs assist in the defense mechanisms of the whole body Platelets prevent loss of the fluid that constitutes the internal environment No organ or system of the body can maintain proper levels of nutrients, gases, or water without direct or indirect help from blood Other systems assist the blood Blood is useless unless it continues to transport, defend, and maintain balance