Current Issues in Disaster Mental Health
advertisement

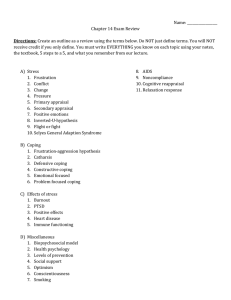
Current Issues in Disaster Mental Health: Clinical Applications Betty Pfefferbaum, M.D., J.D. University of Oklahoma Health Sciences Center May 2007 1 Learning Objectives • Appreciate the importance of child disaster mental health • Identify children’s reactions to disasters and the factors that influence their reactions • Comprehend the rationale in intervention approaches • Recognize the limitations in children’s disaster interventions 2 Through Children’s Eyes, WHO 3 Disaster • Definition – A severe disruption, ecological and psychosocial, which greatly exceeds the coping capacity of the altered community World Health Organization, 1992 4 Are Disasters Increasing? 5 Reasons for Increase in Disasters • Poverty and Vulnerability • Climate Change • Urbanization • Poor Building and Land Use 6 Children’s Reactions and the Factors that Influence Their Reactions 7 Hurricanes 2004 • Charley (August 13) – Category 4 Florida’s Southwest coast – $15 billion • Frances (September 5) – Category 2 Florida’s East coast – $9 billion • Ivan (September 16) – Category 3 Alabama near Florida border – $14 billion • Jeanne (September 26) http://www.nhc.noaa.gov/2004atlan.shtml – Category 3 Florida’s East coast – $7 billion Blake et al. NOAA/NWS/NCEP/TPC/NHC April, 2007; Sallenger et al. 2006 8 Hurricane Katrina August 29, 2005 • Category 3 • 80 mph winds • >90 mph gusts • $81 billion http://www.nhc.noaa.gov/2005atlan.shtml Knabb et al & National Hurricane Center, 2005;NOAA’s Technical Report, 2005 9 Hurricane Andrew 1992 • August 1992 • Category 5 (Winds > 160 mph) • 61 deaths • 135,000 single family and mobile homes destroyed or damaged • $26 billion dollars http://scijinks.jpl.nasa.gov/weather/people/disaster/hurricane_andrew_large.jpg http://www.nhc.noaa.gov/1992andrew.html 10 Model • Primary predictors of posttraumatic stress – Exposure – Perceived life threat – Life-threatening experiences – Loss and disruption – Child characteristics – Sex – Age – Ethnicity – Social environment – Access to social support – Child coping Vernberg et al. 1996 11 % PTSD Symptom Severity 35 Overall mean in moderate range 30 30 26 25 25 Few or no symptoms 20 15 Mild 14 Moderate Severe 10 5 Very severe 5 0 568 school children grades 3 to 5 3 months after Hurricane Andrew Vernberg et al. 1996 12 Predictors of PTSD Symptoms: 3 Months 40 62% variance explained by: Exposure Child characteristics Access to social support Coping 35 35 30 25 21 Exposure 20 Support 15 10 5 5 0 % variance Coping Perceptions of support from Parents Classmates Teachers Close friends Vernberg et al. 1996 13 Access to Social Support Support from teachers and classmates accounted for small but significant variance in PTSD symptoms 1.6 1.4 1.4 * 1.2 1 ** 1 0.8 Parents 0.6 Classmates 0.4 Teachers 0.2 0.2 0.1 Close friends 0 PTSD symptoms Model with exposure, demographics, access to social support, and coping explained > 60% Vernberg et al. 1996 14 Exposure at 7 Months 50 44 45 442 3rd to 5th graders 3 schools Southern Dade County 40 35 30 27 23 25 20 15 10 10 5 0 Home damage Alternate housing 1-2 other 3 or more other La Greca et al. 1996 15 Posttraumatic Stress: Hurricane Andrew Children with moderate to very severe reactions early were at risk for persistent stress reactions 35 30 30 25 27 25 24 23 21 21 20 3 months 15 15 11 7 months 10 months 10 4 5 3 No grade or sex differences 2 0 Mean Symptom Score % Moderate PTSD % Severe PTSD % Very severe PTSD La Greca et al. 1996 16 Posttraumatic Stress: 7 and 10 Months 16 15 Model accounted for 39.1% variance at 7 months 24% variance at 10 months 14 12 10 9 8 7 6 6 5 4 4 4 3 33 3 2 2 Life threat Loss and disruption Demographics Life events Social support Coping 0 7 months 10 months La Greca et al. 1996 17 Posttraumatic Stress 60 54 50 40 40 35 30 20 20 3 months 7 months 27 20 18 13 8 10 3 n = 92 Grades 4-6 0 Posttraumatic Stress Mean RI Score Severe/Very Severe Moderate Mild Doubtful % Level PTSD La Greca et al. 1998 18 Predictors of Posttraumatic Stress 35 32 30 25 20 20 15 14 1112 12 Exposure Pre anxiety Pre attention Pre academic 10 5 0 3 months 7 months La Greca et al. 1998 19 Emotional/Behavioral Outcome • Predictors – Exposure – Child characteristics –Demographics –Pre-existing conditions –Coping – Recovery environment 20 http://www.publicaffairs.noaa.gov/photos/1992andrew2.gif21 Posttraumatic Stress at 2 Months 60 56 Children in Hi-Impact school were more likely to have severe posttraumatic stress 50 41 40 39 N = 144 57% Hi-Impact 43% Lo-Impact Mean = 8.2 yrs 31 30 21 20 doubtful to mild 13 moderate 10 severe to very severe 0 High Impact Low Impact Shaw et al. 1995 22 Posttraumatic Stress in Hi-Impact School Severe posttraumatic stress decreased 70% with moderate to severe posttraumatic stress at 21 months 60 55 51 50 38 40 38 33 30 29 30 no to mild moderate 20 severe 15 11 10 N = 30 0 2 months 8 months 21 months Shaw et al. 1996 23 Disruptive Behavior at 8 Months • There was a marked decrease in disruptive behavior in the Hi-Impact school initially followed by a return to the level of the previous year • Disruptive behavior in the Lo-Impact school remained at much higher levels for longer returning to the level of the previous year at the end of the academic year Shaw et al. 1995 24 Hi-Impact Disruptive Behaviors The initial decrease in disruptive behaviors in Hi-Impact school was followed by A rebound (3-5 months) and A relatively quick return to normalcy (9 months) The effects may be associated with Increased mental health professionals, mobile crisis teams, and crisis intervention Shaw et al. 1995 25 Lo-Impact Disruptive Behaviors The increase in disruptive behaviors in LoImpact school Remained higher for longer Returned to level of the previous year at the end of the academic year This may be related to Relocation of students from more directly affected schools and Increased demand for and shift of resources to directly affected schools Shaw et al. 1995 26 Interventions Early Interventions Assessment General Therapeutic Principles Evidence Base for Interventions 27 Goals of Early Intervention Restore a sense of safety and security Protect from excessive exposure to reminders Validate experiences and feelings Restore equilibrium and routine Open and enhance communication Provide support 28 Recognize Hierarchy of Needs • Survival, safety, security • Food, shelter • Health (physical and mental) • Triage • Orient to immediate service needs • Communicate with family, friends, and community NIMH 2002 29 Assumptions and Principles • In the immediate post-event phase, expect normal recovery • Presuming clinically significant disorder in the early post-event phase is inappropriate except in those with a pre-existing condition NIMH 2002 30 Psychological First Aid • First aid is “the first aid received by a person in trouble” www.oklahomacitybombing.com American Psychiatric Association 1954 31 Psychological First Aid • Protect survivors from further harm • Reduce physiological arousal • Mobilize support for those who are most distressed • Keep families together and facilitate reunion of loved ones • Provide information and foster communication and education • Use effective risk communication techniques NIMH 2002 32 Psychological First Aid • Manuals to guide the delivery of PFA – National Child Traumatic Stress Network and National Center for PTSD – American Red Cross – International Federation of Red Cross and Red Crescent Societies 33 34 Core Actions and Goals - 1 • Make contact and engage – Respond to contacts initiated by survivors – Initiate contacts in a non-intrusive, compassionate, and helpful manner • Provide safety and comfort – Enhance immediate and ongoing safety – Provide physical and emotional comfort NCTSN & NCPTSD 2006 35 Core Actions and Goals - 2 • Stabilize – Calm and orient emotionally overwhelmed or disoriented survivors • Gather information – Identify immediate needs and concerns – Gather additional information NCTSN & NCPTSD 2006 36 Core Actions and Goals - 3 • Offer practical assistance – Help survivors with immediate needs and concerns • Connect with social supports – Help establish brief or ongoing contacts with primary support persons or other sources of support, including family members, friends, and community helping resources NCTSN & NCPTSD 2006 37 Core Actions and Goals - 4 • Provide information on coping – Provide information about stress reactions and coping to promote adaptive functioning • Link with collaborative services – Link survivors with available services needed at the time or in the future NCTSN & NCPTSD 2006 38 Assessment Parent report provides objective information in some areas It is essential to assess children directly as parents may under-estimate their distress Parents may be focused on other issues Parents may be overwhelmed themselves Parents may use denial Children may be especially compliant 39 World Trade Center 1993 • • • • February 26, 1993 6 killed > 1,000 injured Thousands trapped http://www.talkingproud.us/ImagesEagle/AttacksonUS/WTC1993.jpg CNN (1997) & The Joint Terrorism Task Force 40 Children’s Symptoms at 3 and 9 Months • Exposure – 9 trapped in elevator – 13 on observation deck – 27 controls • Measures – Child and parent report http://www.cnn.com/US/9609/05/terror.plot/trade.center.large.jpg Koplewicz et al. 2002 41 Posttraumatic Stress and Fear Parent report: significant decrease Child report: no decrease 35 30 29.6 26.3 25 28 27.7 29.2 26.4 25.5 21.8 20 3 months 15 9 months 10 5 0 Child Parent Posttraumatic Stress Child Parent Incident Fear Koplewicz et al. 2002 42 General Therapeutic Principles Therapy must provide a safe environment to process painful and overwhelming experiences Treatment involves transforming the child’s self concept from victim to survivor Avoidance is a core feature of posttraumatic stress and may impede treatment Treatment may lead to heightened arousal and distress 43 Treatment Approaches Supportive psychodynamic approaches Play therapy Cognitive-behavioral approaches Family therapy Group therapy Medication Rarely needed Adjunctive if used 44 Family Interventions Identify and address parental reactions and needs Educate parents about the effects of their own reactions on their children Inform parents about children’s disaster reactions in general and about their own child’s experiences and reactions Assist families with secondary stresses Help families anticipate the needs of children 45 Small Group Interventions Promote sense of order, control, and security Accommodate more children Provide opportunities for children to - Share with and reassure each other - Practice new skills Educate children about trauma responses Assess coping and its effectiveness Identify those needing more intense interventions 46 School-based Interventions - 1 • Disaster reactions may emerge in the context of school • School settings provide access to children and the potential for enhanced compliance • Schools are a natural support system where stigma associated with treatment is diminished • Services in schools help normalize children’s experiences and reactions Wolmer et al. 2003; Wolmer et al. 2005 47 School-based Interventions - 2 • School personnel are familiar with, and deal with, situational and developmental crises • School curricula already address prevention in other mental health areas • School personnel have opportunities to observe children • Supervision, feedback, and follow-up are possible Wolmer et al. 2003; Wolmer et al. 2005 48 School-based Interventions - 3 • Classroom settings are developmentally-appropriate • Classroom settings provide – – – – – Predictable routines Consistent rules Clear expectations Immediate feedback Stimulus for curiosity and engaging learning skills • School-based interventions facilitate peer interactions and support which may prevent withdrawal and isolation Wolmer et al. 2003; Wolmer et al. 2005 49 Content of Interventions • Trauma • • • • • • • • • – Emotional distress – Arousal – Reminders Loss and grief Anxiety Depression Safety Anger Conduct problems Concentration problems Coping Social support 50 Intervention Techniques • Interventions use – – – – – – – – – Psycho-education Emotional processing Projective techniques Cognitive-behavioral approaches Anxiety-reduction and management techniques Exposure Coping skills enhancement Social support Resilience building • Interventions use individual, group, or mixed format 51 Limitations in General • Convenience samples of modest size – Not able to generalize to – Other groups of children – Other types of disaster – Other settings (geographic or clinical/community) • Lack comparison groups including comparison to natural recovery – Not able to determine – If the intervention was better than another intervention or even natural recovery – What aspect of the intervention was effective • Lack long term follow up 52 QUESTIONS 53