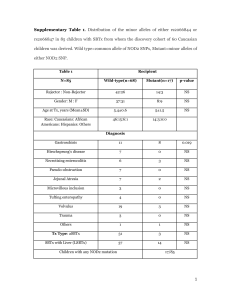
Diagnosis Graft rejection(n= 9)
advertisement
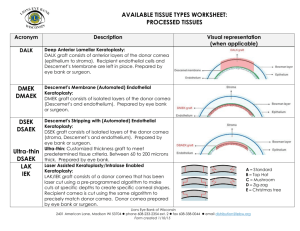
REJECTION IN PEDIATRIC CORNEAL GRAFTS Anita Panda Rakhi Kusumesh Murugesan Vanathi Tushar Agarwal S Khokhar Cornea and Refractive Surgery Services Dr Rajendra Prasad Centre for Ophthalmic Sciences All India Institute of Medical Sciences, New Delhi, India The authors have no financial interest in the subject matter of this poster. INTRODUCTION Congenital corneal opacities are important causes of pediatric corneal blindness. Pediatric keratoplasty 1,2 is technically demanding because of wide range of challenges preoperatively, intraoperatively, and postoperatively. Preoperative •Amblyopia •Ocular pathology •Severity of disease Intraoperative Postoperative •Small-sized globe •Low scleral rigidity •Positive vitreous pressure •Increased fibrin reaction •Increased elasticity of cornea •Repeated examinations under anesthesia (EUA) •Postoperative inflammation •Amblyopia therapy •Secondary glaucoma •Increased risk of rejection 1 Vanathi M, Panda A ,Vengayil S. Pediatric Keratoplasty. Surv Ophthalmol 54:245--271, 2009 2 Huang et al. Primary Pediatric Keratoplasty: Indications and Outcomes. Cornea 2009;28:1003–1008 INTRODUCTION CONTD….. 3. Graft rejection is the most frequent cause for graft failure in pediatric keratoplasty. Pediatric corneal transplantation has an increased rejection rate because of the more active immune system in younger patients.3 In infants with an amplified inflammatory response, graft rejection can occur rapidly and be less responsive to treatment. Early symptoms of graft rejection, reduce visual acuity and ocular discomfort, cannot be communicated resulting in a delay in the diagnosis and treatment Well-established graft rejection in children is usually irreversible. Alldrege C, Krachmer JC. Clinical types of corneal transplant rejection. Arch Ophthalmol. 1981 ;99 : 599--604 PURPOSE To study the incidence of graft rejection in our series of pediatric corneal grafts. METHODS Retrospective analysis of case records of keratoplasty in children < 12 years between 2006 and 2009 with a minimum follow-up of 4 months The parameters analyzed include: demographic profile, indication of surgery, surgical details, donor details, graft outcome, and complications. Ophthalmic evaluation included : visual acuity , slit-lamp biomicroscopic examination (in possible cases), intraocular pressure. Examination under general anesthesia was done whenever required. Ultrasound B scan was used to evaluate the posterior segment. METHODS CONTD…… Penetrating keratoplasty was performed in all cases under general anesthesia by using standard techniques. The mean host cut was 7.33±1.22(SD) mm and mean donor size was 7.80±1.33 (SD)mm . A host–graft disparity of 0.25– 1.0 mm was used. Synechiolysis, anterior vitrectomy, and cataract extraction with or without intraocular lens implantation were done wherever required. Topical steroid and antibiotic eyedrops were used. Topical steroids are given more frequently in the initial postoperative period and gradually tapered and changed to less potent steroids such as fluoromethalone in 3--6 months.Cycloplegics were used whenever required. EUA was performed in early postoperative period and follow up. Peters anomaly RESULT Indication for keratoplasty n (74) % Penetrating keratoplasty had been performed in 74 eyes of 74 children younger than 12 years of age. 45 male and 29 female. Mean age at the time of surgery 5.64 ± 4.24 years (range 2 months – 12 years). Average follow up of 14.05 ± 10.68 months.(4-48 months) Congenital CHED 8 10.6% Non-CHED 9 12% Congenital glaucoma 12 16% Acquired nontraumatic Perforated corneal ulcer 14 18.9% Post keratomalacia corneoiridic scar 5 6.75% Post keratitis corneo-iridic scar 21 28.3% Post traumatic 1 1.35% Regraft 4 5.40% POSTOPERATIVE COMPLICATIONS Complications No of eyes (n=74) n(%) Persistent epithelial defect 7 9.5% Graft rejection 9 12.2% Graft dehiscence 2 2.70% Glaucoma 6 8.10% Cataract 3 4.05% Graft infection 8 10.8% (worsening of glaucoma/post PK glaucoma) In the 74 eyes undergoing keratoplasty, graft rejection (12.2%) was the most common complication followed by graft infection(10.8%) . Incidence of graft rejection Diagnosis Graft rejection(n= 9) % Graft survived Acquired nontraumatic 4 44.4% 2 CHED 3 33.3% 1 Congenital glaucoma 1 11.1% 0 Regraft 1 11.1% 0 The most common reason for graft failure was graft infection(42.1%, n=8) followed by irreversible rejection (31.5%, n=6). Episodes of Graft rejection higher in acquired nontraumatic cases(44.4%), followed by CHED(33.3%). DISCUSSION Corneal grafting in children is different from that in adults because of morphologic and functional aspects, and these differences are reflected in the overall outcome of the surgery. In our study, nearly half of the patients (54.1%) belonged to the acquired nontraumatic group and healed infection was the most common indication for keratoplasty. This is in contrast with the majority of published reports, in which congenital indications contribute a significantly greater proportion.4,5 The reported percentages of graft rejection in pediatric keratroplasty vary between 22%7 and 43.4%4. In this study 12.2% cases of graft rejection found. 4. Aasuri MK, Prashant G, Gokhle N, et al. Penetrating keratoplasty in children. Cornea 2000;19:140–4. 5.Dada T, Sharma N, Vajpayee RB. Indications for pediatric keratoplasty in India. Cornea 1999;18:296–8. DISCUSSION CONTD…… 31.5%(n=6) of graft failure were related to graft rejection whereas Stulting et al6 reported 11% of graft failures to be related to allograft rejections. Rejection was reversible in only 33.3% of episodes, showing a much lower reversal rate in pediatric grafts compared to that of 50--78% in adult grafts3.Reasons are: 1)delay in the diagnosis (can’t communicate) 2) delay in treatment (delay in reaching center) 3) examination required anaesthesia 4) large volume of patients. Successful penetrating keratoplasty in children requires careful preoperative evaluation and selection of patients follow-up by well-motivated parents, an expert corneal transplant surgeon, and a devoted pediatric ophthalmologist. 6.Stulting RD, Sumers KD, Cavanagh HD. Penetrating keratoplasty in children. Ophthalmology. 1984;91:1222—30 7.Vajpayee RB, Ray M, Panda A, et al. Risk factors for pediatric presumed microbial Keratitis: a case control study. Cornea. 1999;18:565--9