PO-03 Outline
advertisement

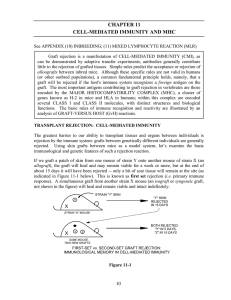
Preservation of the Cornea Graft Aaron Bronner OD Number of CE hours: 2 Course description: Review of sources of graft failure and their respective interventions. PKP, DALK, and DSAEK/DMEK will be discussed Treatment and Management of Anterior Segment Disease Outline: Preservation of the corneal graft I. Intro and Background a. History of Grafting i. Penetrating Keratoplasty ii. Deep Anterior Lamellar Keratoplasty iii. Posterior Lamellar Keratoplasties b. Corneal immunity i. Concept of Immune Privilege ii. Manifestations of Immune privilege 1. Lack of MHC II + APC 2. Lack of vascularization 3. Lack of lymph channels 4. ACAID iii. How this relates to grafts iv. How immune privilege breaks down with inflammation c. Role of OD in care of the grafted eye i. Visual Rehab ii. Graft Preservation d. Causes of Graft Failure i. Specific breakdown of sources of failure in different graft types 1. Early/Primary Failure 2. Rejection 3. Vascularization 4. Infection 5. Scarring 6. Neurotrophic issues 7. Late Endothelial Decompensation 8. Globe Rupture II. Inflammation of the Graft a. Rejection i. Targets ii. Manifestations iii. Differences in the graft types b. Vascularization and lymphangiogenesis i. Relative importance for risk of rejection ii. Emerging importance of lymphangiogensis c. Scarring d. Treatment i. Corticosteroids (oral and topical) ii. Immune modulatory (oral and topical) iii. Anti-VEGF role 1. Anti CNV effects 2. Anti CL effects 3. Anti inflammatory effects (anti chemotractant) iv. Amniotic Membrane 1. Works as a “heat sink” for inflammation 2. Sutured in or prokerra 3. Theoretically tempers healing response which should provide less scarring 4. Some inherent antimicrobial properties III. Infection of the graft a. Factors that enhance risk of infection i. Modulation of corneal immune response inherently increases risk of infection ii. Use of contact lenses iii. Ocular surface disease b. Sources of infection i. Viral ii. Bacterial iii. Atypical organisms c. Prognosis of infection in the context of a grafted eye i. Poor – up to 60% require regraft in the presence of infectious corneal ulcer (excluding herpetic disease) d. Balancing act of graft infection treatment with rejection prevention i. Concomitant need for immune suppression and immune responsiveness ii. SCORE study implications not applicable IV. Neurotrophic features of the graft a. Sources of neurotophy b. Effects on ocular surface and resultant tissue breakdown c. Treatment i. Lubricating therapies (ATS, punctual occlusion, cyclosporine) ii. BSCL iii. Tarrsorhaphy iv. Autologous serum 1. Studies looking at effetivness of autologous serum 2. Sterility not guaranteed…use with caution and in an appropriately consented patient v. Amniotic membrane 1. Provides an artificial basement membrane that aides in wound healing 2. Provision of Growth factors 3. Prokera vs sutured in a. Role of actual or “tape” tarrsorhaphy V. Summary a. Graft preservation is often a balance of treating problems that exist and opening the door for another problem to develop b. Traditional strategies are generally effective c. Newer strategies hold promise as more targeted approaches