Short Stay Form - Emory Johns Creek Hospital
advertisement
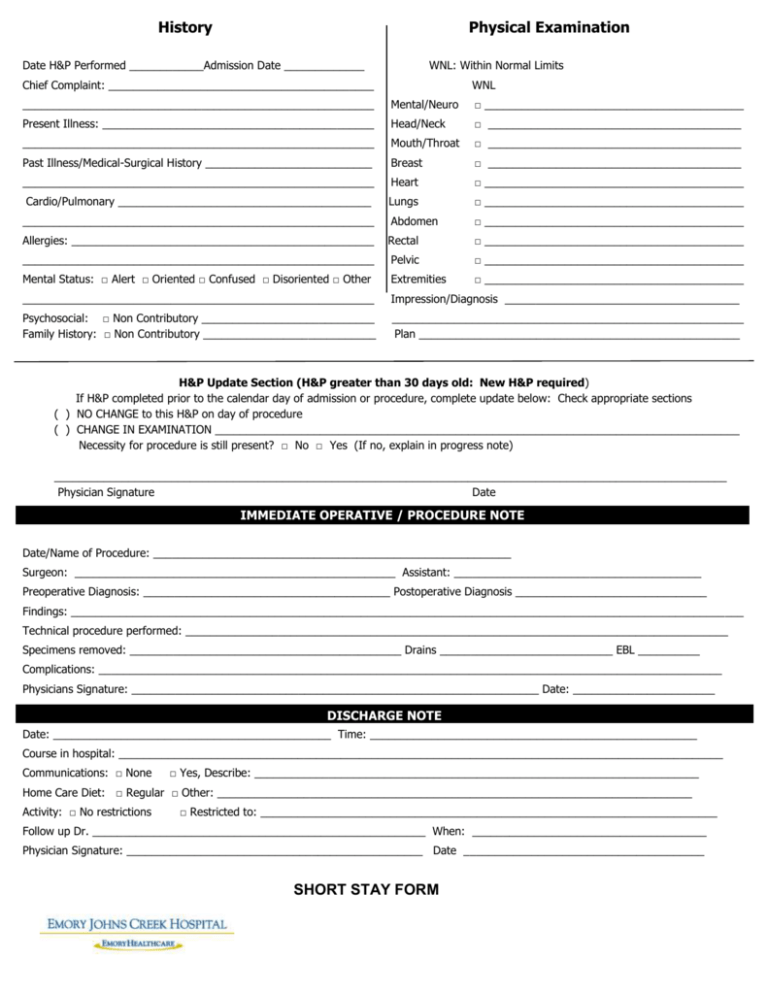
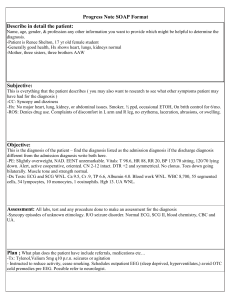
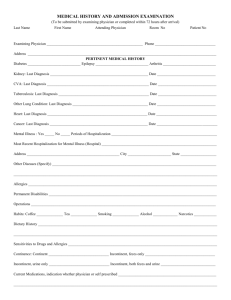
History Physical Examination Date H&P Performed ____________Admission Date _____________ WNL: Within Normal Limits Chief Complaint: ___________________________________________ WNL _________________________________________________________ Mental/Neuro □ __________________________________________ Present Illness: ____________________________________________ Head/Neck □ _________________________________________ _________________________________________________________ Mouth/Throat □ _________________________________________ Past Illness/Medical-Surgical History ___________________________ Breast □ _________________________________________ _________________________________________________________ Heart □ __________________________________________ Cardio/Pulmonary _________________________________________ Lungs □ __________________________________________ _________________________________________________________ Abdomen □ __________________________________________ Allergies: _________________________________________________ Rectal □ __________________________________________ _________________________________________________________ Pelvic □ __________________________________________ Mental Status: □ Alert □ Oriented □ Confused □ Disoriented □ Other Extremities □ __________________________________________ _________________________________________________________ Impression/Diagnosis ______________________________________ Psychosocial: □ Non Contributory ____________________________ Family History: □ Non Contributory ____________________________ _________________________________________________________ Plan ____________________________________________________ H&P Update Section (H&P greater than 30 days old: New H&P required) If H&P completed prior to the calendar day of admission or procedure, complete update below: Check appropriate sections ( ) NO CHANGE to this H&P on day of procedure ( ) CHANGE IN EXAMINATION _____________________________________________________________________________________ Necessity for procedure is still present? □ No □ Yes (If no, explain in progress note) _____________________________________________________________________________________________________________ Physician Signature Date IMMEDIATE OPERATIVE / PROCEDURE NOTE Date/Name of Procedure: __________________________________________________________ Surgeon: ____________________________________________________ Assistant: ________________________________________ Preoperative Diagnosis: ________________________________________ Postoperative Diagnosis _______________________________ Findings: _____________________________________________________________________________________________________________ Technical procedure performed: ________________________________________________________________________________________ Specimens removed: ____________________________________________ Drains ____________________________ EBL __________ Complications: _____________________________________________________________________________________________________ Physicians Signature: __________________________________________________________________ Date: _______________________ DISCHARGE NOTE Date: _____________________________________________ Time: _____________________________________________________ Course in hospital: __________________________________________________________________________________________________ Communications: □ None □ Yes, Describe: ________________________________________________________________________ Home Care Diet: □ Regular □ Other: _____________________________________________________________________________ Activity: □ No restrictions □ Restricted to: __________________________________________________________________________ Follow up Dr. ______________________________________________________ When: ______________________________________ Physician Signature: ________________________________________________ Date _______________________________________ SHORT STAY FORM (REV 7/08)