Powerpoint 24 Urinary - People Server at UNCW
advertisement

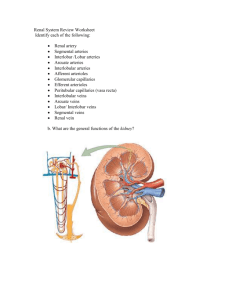
Urinary System A. Kidneys 1. External anatomy 2. Internal anatomy 3. Nephron a. Parts of the nephron b. Cortical and juxtamedullary nephrons c. Histology of the nephron 4. Blood and nerve supply B. Physiology of urine formation 1. Glomerular filtration a. Net filtration pressure b. Glomerular filtration rate c. Regulation of GFR 2. Tubular reabsorption 3. Countercurrent multiplier and exchange system 4. Tubular secretion 5. Renal clearance C. Ureters 1. Structure 2. Histology 3. Physiology D. Urinary bladder 1. Structure 2. Histology 3. Physiology E. Urethra 1. Histology 2. Physiology What is excretion? How is it different from secretion? Why do we need a urinary system? 1. protein catabolism yields toxic nitrogenous wastes (ammonia and urea) 2. water and essential ions tend to accumulate Organs that contribute to the function of waste elimination from the body include: 1. 2. 3. 4. kidneys lungs sudoriferous glands gastrointestinal tract The urinary system consists of: 1. 2. 3. 4. kidneys (2) ureters (2) urinary bladder urethra The kidneys have several general functions: 1. regulate blood volume and composition 2. regulate blood pressure (renin) 3. secrete erythropoietin 4. vitamin D synthesis Kidney-external 1. location a. T12 - L3 b. retroperitoneal 2. gross appearance 3. hilus 4. coverings a. renal fascia b. adipose capsule c. renal capsule Kidney-internal 1. medulla a. renal pyramids b. renal papillae 2. cortex a. renal columns b. cortical vs juxtamedullary nephrons 3. renal pelvis and calyces Nephrons, the functional units of the kidneys, have three basic functions: 1. filtration 2. reabsorption 3. secretion Types of Nephrons juxtamedullary nephron (with very long loop of Henle) 1. cortical (85%) 2. juxtamedullary (15%) cortical nephron (with relatively short loop of Henle) Parts of a Nephron 1. renal corpuscle a. glomerulus b. Bowman's capsule (parietal vs visceral) 2. renal tubule a. proximal convoluted b. loop of Henle c. distal convoluted Bowman's capsule and the endothelialcapsular membrane 1. parietal vs. visceral layers 2. fenestrated endothelial cells (restrict formed elements) 3. fused basement membranes (restrict plasma proteins) 4. visceral layer = podocytes a. pedicels b. filtration slits Renal Tubule Histology 1. PCT = simple cuboidal + brush border 2. loop of Henle = simple squamous 3. DCT = simple cuboidal + hormone receptors 4. Collecting Ducts= Simple cuboidal Renal Blood Supply 1. ~25% of CO (1,250 ml/min) via the renal arteries segmental arteries interlobar arteries arcuate arteries 2. afferent arteriole ---> glomerulus ---> efferent arteriole---> 3. peritubular capillaries and vasa recta Renal Blood Supply 1. ~25% of CO (1,250 ml/min) via the renal arteries segmental arteries interlobar arteries arcuate arteries 2. afferent arteriole ---> glomerulus ---> efferent arteriole---> 3. peritubular capillaries and vasa recta Juxtaglomerular Apparatus 1. location 2. macula densa cells 3. juxtaglomerular cells ___________________ 4. decreased BP = renin secretion 5. vasoconstrictor substance Filtrate formation high-increased Filtrate formation low-decreased Nerve supply of the kidneys Renal nerves arise from the superior mesenteric ganglion- mostly sympathetic fibers Regulate blood flow and stimulate secretion of renin Nephrons carry out three important functions: 1. control blood concentration and volume 2. regulate blood pH 3. remove toxic wastes from the blood What do nephrons accomplish? Urine formation requires three processes: 1. glomerular filtration by the renal corpuscle 2. tubular reabsorption by the renal tubule 3. tubular secretion by the renal tubule Glomerular filtration is the first step in urine formation. 1. 2. 3. 4. principle of filtration endothelial-capsular membrane blood hydrostatic pressure is the driving force filtrate = all blood components except formed elements and plasma proteins 5. filtrate = 180 L/day urine = 1 - 2 L/day filtrate reabsorbed = 178 - 179 L/day Features of the renal corpuscle that enhance its blood-filtering capacity: 1. glomerular capillaries are long 2. endothelial-capsular membrane is porous and thin 3. glomerular blood hydrostatic pressure is high due to relationship between afferent and efferent arterioles Net filtration pressure (NFP) 1. glomerular blood hydrostatic pr. 2. capsular hydrostatic pr. 3. blood colloid osmotic pr. ___________________________ 4. NFP = GBHP - (CHP + BCOP) = 60 - (18 + 32) or (15 + 27) = +10 mm Hg ___________________________ 5. filtration fraction = 10% (1,250 ml/min x 0.1= 6. GFR = 125 ml/min) Glomerular filtration rate (GFR) 1. GFR = 125 ml filtrate produced every minute 2. GFR is directly related to the NFP. 3. Homeostasis requires a relatively constant GFR: a. if GFR is too high, then... b. if GFR is too low, then... Regulation of GFR 1. glomerular blood flow depends on 2 factors: a. systemic blood pressure b. afferent and efferent arteriolar diameters 2. factors regulated by three mechanisms a. renal autoregulation b. hormonal regulation c. neural regulation Renal Autoregulation 1. myogenic mechanism Tendency of smooth muscle of afferent arteriole to contract when arterial BP is high, relaxes when arterial BP is low 2. tubuloglomerular feedback (vasoconstrictor substance) Renal Autoregulation MYOGENIC MECHANISM increased blood pressure TUBULOGLOMERULAR FEEDBACK increased GFR increased flow of tubular fluid stretch of afferent arteriole arteriolar vasoconstriction decreased glomerular blood pressure decreased NFP macula densa cells secrete vasoconstrictor substance onto juxtaglomerular cells vasoconstriction of afferent arteriole decreased glomerular blood pressure decreased NFP decreased filtration decreased filtration works the opposite way with decreased BP works the opposite way with decreased GFR Renin-Angiotensin System Atrial Natriuretic Peptide (ANP) When BP is too high, ANP is produced by the heart which inhibits sodium and water reaborption and the secretion of renin and ADH. Kidneys eliminate more sodium and water and lower blood pressure Neural Regulation of GFR Sympathetic Nervous System Tubular Reabsorption of Solutes 1. tubular maximum (TM) 2. active transport a. receptors (carriers) b. glucose and amino acids (100% of the time) c. Na+ and K+ (aldosterone controlled) d. Ca++ (PTH and CT controlled) 3. passive transport (diffusion) a. diffusion or electrical b. Cl-, PO4-- Tubular Reabsorption of Water 1. obligatory reabsorption (90%) a. osmosis related to solutes b. Na+ has major effects 2. facultative reabsorption (10%) (controlled by ADH) Negative Feedback Control of ADH CONTROLLED CONDITION Blood osmotic pressure (decreased water concentration) is increased in response to some stressor RETURN TO HOMEOSTASIS In response, there is increased water reabsorption, and blood osmotic pressure decreases RECEPTOR Hypothalamic osmoreceptors respond to increased blood osmotic pressure and send nerve impulses to appropriate neurons in hypothalamus EFFECTORS In response to ADH, aquaporins in distal tubules and collecting ducts become more permeable to water CONTROL CENTER Hypothalamic neurons, via the posterior pituitary gland, secrete ADH in the blood The concentration gradient in interstitial fluid Contributing factors: 1. The nephron loop via the countercurrent multiplier 2. The Vasa recta via the countercurrent exchange system 3. Urea Recycling The countercurrent multiplier-Responsible for establishing the salt concentration gradient with the interstitial fluid. Countercurrent- tubular fluid reversing directions Multiplier- positive feedback loop that increases concentration of salts. Blood flows in opposite direction to nephron loop Exchanges salts for water Countercurrent Exchange System (Loop of Henle and Vasa Recta) Blood flows in opposite directions To Loop of Henle. As blood flows down alongside Ascending loop of Henle, water is lost and salt gained. As blood flows up alongside Descending loop of Henle, water is gained and salt lost. Overall, vessels absorb more water on the way out than they Gave up on the way in. Osmolarity of medulla maintained And water and solutes maintained. The Loop of Henle acts as a Countercurrent multiplier Tubular secretion 1. cells secrete directly into filtrate 2. two principal effects a. directly excrete substances (H+, NH3, K+, creatinine) b. control body fluid pH (H+, NH4+) If H+ secretion = HCO3- filtration then no change occurs in extracellular fluid pH. If H+ secretion < HCO3- filtration, then extracellular fluid(blood) pH decreases. If H+ secretion > HCO3- filtration, then extracellular fluid (blood)pH increases. Secretion and Neutralization of H+ ions in Kidney Renal Clearance Renal clearance is the volume of blood plasma from which a particular waste is completely removed in 1 minute. What would you expect the renal clearance of glucose to be in a normal individual? Summary of Nephron Functions Urine Drainage 1. papillary ducts ---> minor calyces ---> major calyces ---> renal pelvis ---> 2. ureters a. location b. anatomy c. function Urinary Bladder 1. location 2. anatomy 3. histology a. detrusor muscle b. sphincters 4. micturition reflex Urethra 1. anatomy 2. location a. female b. male (1) prostatic (2) membranous (3) penile Micturition reflex (in the adult) 1. stretch of the bladder (1/2 full) stimulates stretch receptors 2. sacral parasympathetic area output, causing: a. contraction of the detrusor muscle; and b. reflex relaxation of the internal urethral sphincter 3. association neuron carries information to cerebrum for conscious awareness 4. voluntary relaxation of the external urethral sphincter (in the infant, this is also reflexive) 5. expulsion of urine through urethra Neural Control of Micturition