Physiology of kidney. Uropoesis. Role of kidney in keeping
advertisement

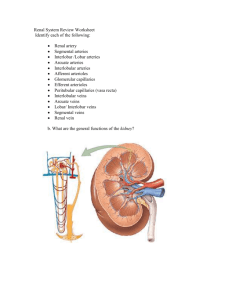
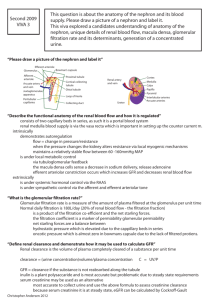
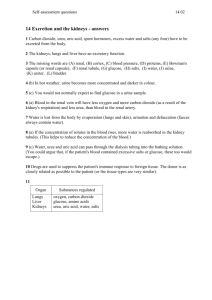
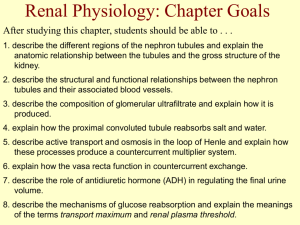
Physiology of excretory system (role of separate organs and systems) Function of kidney 1. Excretion of ending nitrogen metabolic products. 2. Excretion of strange substances. 3. Excretion of excess of organic and unorganic substances, which get into organism with food and formed in metabolic processes. 4. Supporting of osmotic pressure of blood in a constant level. 5. Supporting ionic balance of organism. 6. Supporting of acid-base condition of organism. 7. Take part in blood circulations' regulation. 8. Development of biological active substances and enzymes (bradikinine, prostaglandines, urokinase, vitamine D3, erythropoietin, renin etc.). 9. Take place in regulation of blood circulation volume. Juxtaglomerular Apparatus (continued) Insert fig. 17.25 PHYSIOLOGIC CONTROL OF GLOMERULAR FILTRATION AND RENAL BLOOD FLOW The determinants of GFR that are most variable and subject to physiologic control include the glomerular hydrostatic pressure and the glomerular capillary colloid osmotic pressure. These variables, in turn, are influenced by the sympathetic nervous system, hormones and vasoactive substances that are released in the kidneys and act locally, and other feedback controls that are intrinsic to the kidneys. Increased angiotensin II levels that occur with a low-sodium diet or volume depretion help to preserve GFR and to maintain a normal excretion of metabolic waste products, such as urea and creatinine, that depend on glomerular filtration for their excretion. Endothelial-Derived Nitric Oxide Decreases Renal Vascular Resistance and Increases GFR A basal level of nitric oxide production appears to be important for preventing excessive vasoconstriction of the kidneys and allowing them to excrete normal amounts of sodium and water. Administration of drugs that inhibit the formation of nitric oxide increases renal vascular resistance and decreases GFR and urinary sodium excretion, eventually causing high blood pressure. URINE FORMATION The rates at which different substances are excreted in the urine represent the sum of three renal processes, (1) glomerular filtration, (2) reabsorption of substances from the renal tubules into the blood, and (3) secretion of substances from the blood into the renal tubules. Expressed mathematically, Urinary excretion rate = Filtration rate - Reabsorption rate + Secretion rate Three basic renal processes The substance is freely filtered but is also partly reabsorbed from the tubules back into the blood. For each substance in the plasma, a particular combination of filtration, reabsorption, and secretion occurs. The rate at which the substance is excreted in the urine depends on the relative rates of these three basic renal processes. The three basic renal processes Glomerular filtration Tubular reabsorption Tubular secretion GFR is very high: ~180l/day. Lots of opportunity to precisely regulate ECF composition and get rid of unwanted substances. N.B. it is the ECF that is being regulated, NOT the urine. Role of effective filtration pressure Effective filtration pressure = P glomerulus blood - (P oncotic + P capsula) = 65 - (25+15) = 25 mm Hg. Glomerular filtration rate is the volume of filtrate produced by both kidneys each minute. Glomerular filtration rate in average is 90-130 ml/(min x 1,73 m2). Tubular reabsorption Tubular reabsorption may be active or passive. In primary convoluted tubule reabsorbted amino acids, glucose, vitamins, proteins, microelements, 2/3 of water, unorganic salts, such as Na+, K+, Ca++, Mg++, Cl-, HCO3-. It all connect with sodium reabsorption Na+, K+, and H+ Relationship Na+ reabsorption in CD creates electrical gradient for K+ secretion. Plasma [K+] indirectly affects [H+]. When extracellular [H+] increases, H+ moves into the cell, causing K+ to diffuse into the ECF. In severe acidosis, H+ is secreted at the expense of K+. Insert fig. 17.27 Determination of tubular reabsorption level Reabsorption of water = [(speed of glomerular filtration - diuresis per minute) / speed of glomerular filtration] x 100 %. At norm it equal 98-99 %. Concentration of urine In loop enters urea, which is isotonic according to intracellular fluid. Water reabsorbed here by help of countercurrent mechanism. This mechanism determined by functional characteristic of kidneys: 1) if the loop of Henle in deep position in medulla part it increase the osmotic pressure of intracellular fluid; 2) ascending part is not so permeable to water; 3) epithelium of ascending part by help of active transport system take out sodium and chloride ions. Descending Limb LH Deeper regions of medulla reach 1400 mOsm/L. Impermeable to passive diffusion of NaCl. Permeable to H20. Hypertonic interstitial fluid causes H20 movement out of the descending limb via osmosis, and H20 enters capillaries. Fluid volume decreases in tubule, causing higher [Na+] in the ascending limb. Insert fig. 17.16 Countercurrent Multiplier System Multiplies the [interstitial fluid] and [descending limb fluid]. Flow in opposite directions in the ascending and descending limbs. Close proximity of the 2 limbs: Allows interaction. Positive feedback. Insert fig. 17.16 Vasa Recta Countercurrent exchange. Recycles NaCl in medulla. Transports H20 from interstitial fluid. Descending limb: Urea transporters. Aquaporin proteins (H20 channels). Ascending limb: Fenestrated capillaries. Insert fig. 17.17 Vasa Recta (continued) Vasa recta maintains hypertonicity by countercurrent exchange. NaCl and urea diffuse into descending limb and diffuse back into medullary tissue fluid. At each level of the medulla, [solute] is higher in the ascending limb than in the interstitial fluid; and higher in the interstitial fluid than in descending vessels. Walls are permeable to H20, NaCl and urea. Colloid osmotic pressure in vasa recta > interstitial fluid. Osmolality of Different Regions of the Kidney Insert fig. 17.19 Urea Contributes to total osmolality of interstitial fluid. Ascending limb LH and terminal CD are permeable to urea. Terminal CD has urea transporters. Urea diffuses out CD and into ascending limb LH. Recycle urea. Insert fig. 17.18 Collecting Duct Medullary area impermeable to high [NaCl] that surrounds it. H20 is drawn out of the CD by osmosis. The walls of the CD are permeable to H20. Rate of osmotic movement is determined by the # of aquaporins in the cell membrane. Permeable to H20 depends upon the presence of ADH. When ADH binds to its membrane receptors on CD, it acts via cAMP. Stimulates fusion of vesicles with plasma membrane. Incorporates water channels into plasma membrane. Secretion Secretion of substances from the peritubular capillaries into interstitial fluid. Then transported into lumen of tubule, and into the urine. Allows the kidneys to rapidly eliminate certain potential toxins. Proximal Tubule Secretion Insert fig. 17.13 Transport Process Affecting Renal Clearance Ability of the kidneys to remove molecules from plasma and excrete those molecules in the urine. If a substance is not reabsorbed or secreted, then the amount excreted = amount filtered. Quantity excreted = V x U Quantity excreted = mg/min. V = rate of urine formation. U = inulin concentration in urine. Secretion process a) Organic acids and bases (choline) (It secretes by help of active mechanism.) b) Potassium (Sodium can change on H+ and K+ ions). c) Ammonium (It secretes by help of mechanism of anionic diffusion.) K+ Secretion 90% filtered K+ is reabsorbed in early part of the nephron. Secretion of K+ occurs in CD. Amount of K+ secreted depends upon: Amount of Na+ delivered to the region. Amount of aldosterone secreted. As Na+ is reabsorbed, lumen of tubule becomes –charged. Potential difference drives secretion of K+ into tubule. Transport carriers for Na+ separate from transporters for K+. Modulation of K+ secretion Luminal factors Stimulators Inhibitors Flow rate [K+] [Na+] [Cl-] [Cl-] [Ca2+] [HCO3-] Ba2+ -ve luminal voltage Amiloride Selected Diuretics Peritubular Factors Stimulators Inhibitors K+ intake [K+] Adrenaline pH Aldosterone ADH pH K+ Secretion Final [K+] controlled in CD by aldosterone. When aldosterone is absent, no K+ is excreted in the urine. High [K+] or low [Na+] stimulates the secretion of aldosterone. Only means by which K+ is secreted. (continued) Insert fig. 17.24 Effective kidney plasma flow = (concentration of paraaminohippuric acid in urine x diuresis per minute) : concentration of paraaminohippuric acid in plasma Effective kidney blood flow = Effective kidney plasma flow : (1 – hematocrit).) Measurement of Renal Blood Flow Not all blood delivered to glomeruli is filtered in the glomerular capsules. Most of glomerular blood passes to the efferent arterioles. 20% renal plasma flow filtered. Substances are returned back to blood. Substances in unfiltered blood must be secreted into tubules to be cleared by active transport (PAH). PAH can be used to measure renal plasma flow. Measurement of Renal Blood Flow (continued) Filtration and secretion clear only the molecules dissolved in plasma. PAH clearance actually measures renal plasma flow. To convert to total renal blood flow, the amount of blood occupied by erythrocytes must be taken into account. Averages 625 ml/min. Foreign substances and drugs are also poorly reabsorbed but, in addition, are secreted from the blood into the tubules, so that their excretion rates are high. Excretion of Metabolic Waste Products, Foreign Chemicals, Drugs, and Hormone Metabolites The kidneys are the primary means for eliminating waste products of metabolism that are no longer needed by the body. These products include urea (from the metabolism of amino acids), creatinine (from muscle creatine), uric acid (from nucleic acids), the end products of hemoglobin breakdown (such as bilirubin), and metabolites of various hormones. These waste products must be eliminated from the body as rapidly as they are produced. The kidneys also eliminate most toxins and other foreign substances that are either produced by the body or ingested, such as pesticides, drugs, and food additives. Regulation of Arterial Pressure In addition, the kidneys contribute to short-term arterial pressure regulation by secreting vasoactive factors or substances, such as renin, that lead to formation of vasoactive products (for example, angiotensin II). The kidneys play a dominant role in longterm regulation of arterial pressure by excreting variable amounts of sodium and water.