Nutritional Concerns During Pregnancy – Well
advertisement

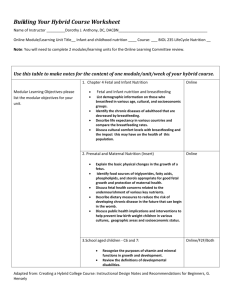
Substance Abuse and Nutrition: Imperfect Together Alyce Thomas, RD Perinatal Nutrition Consultant Dept. of Obstetrics and Gynecology St. Joseph’s Regional Medical Center Paterson, NJ 1 Outline Potential Effects of Substance Use on Nutritional Status Specific Risks Associated with Substance Use in Pregnancy Components of Nutrition Assessment Assessing Dietary Intake Nutrients of Major Concern in Pregnancy Nutrition-related Concerns of Substance Abuse in Pregnancy Nutrition Interventions 2 Potential Effects of Substance Use on Nutritional Status Appetite suppression Poor food choices Reduced nutrient intake Impaired nutrient absorption/metabolism Inadequate weight loss/gain Gastrointestinal discomforts 3 Nutritional Risks Associated with Substance Use Alcohol Cocaine Heroin Marijuana Tobacco Caffeine 4 Alcohol Alcohol contains calories!! Interferes with digestion, storage, utilization and excretion of nutrients Alcohol affects maternal and fetal nutrition 5 Calorie Content Carbohydrates Protein Fat Alcohol 4 kcal/gram 4 kcal/gram 9 kcal/gram 7 kcal/gram 6 Alcohol Alcohol contains calories!! Interferes with digestion, storage, utilization and excretion of nutrients Alcohol affects maternal and fetal nutrition 7 Gastrointestinal Tract 8 Central Nervous System 9 Nutrients Affected by Alcohol Protein Carbohydrates Lipids Vitamins Minerals Water 10 Alcohol Alcohol contains calories!! Interferes with digestion, storage, utilization and excretion of nutrients Alcohol affects maternal and fetal nutrition 11 Alcohol Affects to Fetus Impairs placental nutrient transport Glucose transport necessary for fetal brain development Prenatal insulin resistance may lead to glucose intolerance later in life Folate and zinc deficiency may lead to neural tube teratogenesis Animal studies found that the effect of alcohol was not as severe when maternal diet adequate in zinc 12 Cocaine Little is known about effects of cocaine on maternal and fetal nutrition Interferes with appetite Causes maternal and fetal vasoconstriction → fetal hypoxia nutrient supply → IUGR 13 Growth patterns of infants exposed to cocaine and other drugs in utero Author: Harsham et al Setting: Northern California Sample: 31 infants exposed to drugs in utero Outcome: 1. Birth weight, birth length were significantly lower than NCHS 2. By 6 months, no significant differences for weight, but differences in length J Amer Diet Assoc 1994;94(9):999 14 Heroin Associated with birth weight, prematurity and IUGR Common symptom of opiate abuse: constipation May be poorly nourished Vitamin deficiencies Iron deficiency anemia Folic acid deficiency anemia May experience food cravings 15 Marijuana Associated with birth weight and length Conflicting study results have not shown any nutrition-related effects of marijuana use in pregnancy Weight gain ? Weight loss ? No difference in women who smoked marijuana and those who did not 16 Tobacco Decreased birth weight associated with maternal smoking Associated with IUGR Nutrition-related effects Lower availability of calories ↑ iron requirements availability of certain nutrients (B12, amino acids, vitamin C, folate, zinc 17 Caffeine Affects the CNS 15 minutes after ingestion Caffeine intake > 300 mg/day linked to ↑ 1st trimester abortions Moderate to heavy caffeine linked to: Lower birth weight ↑ risk of preterm labor Delayed conception absorption and ↑ urinary losses of vitamin B1, zinc, iron and calcium 18 Caffeine Content of Selected Beverages 8-oz. Mg. Coffee, drip 115-175 Coffee, brewed 80-135 Coffee, espresso 100 Coffee, instant 65-100 Tea, iced 47 Tea, brewed 60 Tea, green 15 Hot cocoa 14 Coffee, decaf 3-4 12 oz. Mg. Red Bull Pepsi One Mountain Dew Diet Coke Pepsi Coke Snapple teas Slim Fast 80 55.5 55 45.6 37.5 34 31.5 20 (chocolate flavored) Sprite 0 19 Nutrition Assessment Medical history – past and present Obstetrical history Psycho/social/economic history Nutrition history Weight 20 Medical/Obstetric History Age Estimated due date Present history Previous obstetric history Past medical history Family history of chronic illness Medications or nutrient supplements Physical signs of nutritional deficiencies 21 Psycho/Socio/Economic History Financial status Current living conditions Relationship with family Cultural/religious background Food availability Participation in food programs Work/school schedule Educational level 22 Nutrition Assessment Pre-pregnancy weight/usual weight Current height Appetite Recent appetite changes Current diet or food plan Cravings/allergies/ intolerance Pica Medications – herbal, dietary supplements PNV, OTC Alcohol – drink or cook 23 Nutrition Assessment Snack patterns Dental problems Raw or undercooked protein foods GI discomforts Fluid intake Substance use Ptyalism Physical activity Planned method of infant feeding Foods eaten away from home 24 Assessing Dietary Intake Referral Form Nutrition Questionnaire Food Frequency Questionnaire 24-Hour Recall Food Record 25 Why Is Weight Gain Important? Effects fetal growth and length of gestation Inadequate weight gain associated with ↑ prematurity &low birth weight (LBW) LBW major determinant for morbidity and mortality LBW associated with ↑ risk of CVD, DM, HTN and obesity in later years 26 Body Mass Index BMI IOM NHLBI WHO Underweight < 19.8 < 18.5 < 18.5 Normal > 19.8 – 26.0 18.5 – 24.9 18.5 – 24.9 Overweight >26.0 – 29.0 25.0 – 29.9 25.0 – 29.9 Obesity > 29.0 > 30.0 > 30.0 27 Recommended Weight Gain Underweight 28 – 40 lb. Normal weight 25 – 35 lb. Overweight 15 – 25 lbs. Obese Individualize 28 Components of Weight Gain Baby Placenta Amniotic fluid 7½ lb. 1½ lb. 2 lb. Mother Breasts Uterus Body fluids Blood Maternal Stores 2 lb. 2 lb. 4 lb. 4 lb. 7 lb. 29 Inadequate Weight Gain Measurement error Disordered eating Restrictive eating or dieting Pica Depression/stress Inadequate food access GI Discomforts 30 Excessive Weight Gain Measurement error Smoking cessation Infrequent large meals ↑ calorie intake Physical inactivity Multiple gestation Depression/stress Binge eating Pica 31 32 Nutrient Concerns During Pregnancy Carbohydrates Fiber Protein Fat Calcium Magnesium Vitamin D Iron Folate Zinc* 33 Carbohydrates Choose fiber rich fruits, vegetables and whole grains Limit intake of foods with added sugar Fiber recommendation – 14 gm/1000 calories Discretionary calories Not to exceed allowance for calorie level 34 Protein Dietary Reference Intake for protein in pregnancy: 71 gm/day + 25 gm after 1st trimester 35 Fats < 10% of calories from saturated fats < 300 mg/day dietary cholesterol Keep trans fats as low as possible Total fat intake: 20 to 35% of total calories mostly from unsaturated fats 36 Essential Fatty Acids Omega-3 (linolenic acid) All fish and seafood Egg yolks Soybeans Canola, flaxseed and olive oils Omega-6 (linoleic acid) Walnuts, peanuts, almonds Seeds, such as sunflower Corn, safflower and sunflower oils 37 Calcium, Vitamin D and Magnesium Calcium Vitamin D Deposited in fetal skeleton mainly in 3rd trimester Required for calcium homeostasis Maternal deficiency associated with neonatal rickets Magnesium Regulates calcium absorption and relaxes smooth muscle Main foods sources: unprocessed whole grains 38 Folate 600 mcg in pregnancy ↑ up to 4 mg if previous NTD or anti-seizure meds Food sources Fortified and whole grain breads and cereals Dark, green, leafy vegetables Avocado, oranges 39 Iron Iron deficiency is very common in women Pre-pregnant requirements: 15 – 18 mg/d Pregnancy requirements: 27 mg/d CDC recommends 30 mg/d supplement at initial prenatal visit Food sources Heme iron rich or non-heme iron with facilitators 40 Zinc Essential for fetal growth & development Affects protein synthesis Aids absorption of B-complex vitamins Deficiencies: congenital anomalies, IUGR, prematurity Food sources: meat, fish, eggs, shellfish 41 42 43 Food Groups to Encourage Eat 2 cups of fruits and 2½ cups of vegetables daily Vegetables Dark green, orange, legumes, starchy vegetables, other vegetables Fruits Fresh, frozen, canned, dried 44 Food Groups to Encourage Whole Grains Important for fiber and other nutrients Recommend > 3 oz. equivalents/d ½ of all grains should be whole grains 45 Milk and Milk Products Pregnancy Requirements > 3 servings/day Milk alternatives Yogurt Lactose-free milk Non-dairy calciumcontaining alternatives 46 Pregnancy and Vegetarian Nutritional Concerns Calories Iron Zinc Calcium and Vitamin D Vitamin B12 Fats 47 Tips for Common GI Discomforts of Pregnancy Nausea and Vomiting Heartburn Constipation Ptyalism 48 Food Safety Avoid in pregnancy Raw or unpasteurized milk products Raw or soft cooked eggs Raw or rare meat products Unpasteurized juices or milk products 49 Food Safety Wash hands, utensils and cutting surfaces after handling food Cook foods thoroughly Wash raw fruits and vegetables before eating Separate uncooked meat products from other foods Chill perishable foods promptly 50 Breastfeeding and Substance Abuse AAP recommends exclusive breastfeeding for 1st 6 months of life Healthy People 2010: 75% women breastfeeding in early postpartum period Recommendations for substance abusing women? 51 Breastfeeding and Substance Abuse Most illegal drugs contraindicated to breastfeeding Smoking – separate room from baby, after breastfeeding Alcohol – no more than 1 –2 drinks per week Caffeine – AAP considers safe Limit to < 2 cups/day 52 Treatment of Neonatal Abstinence Syndrome with Breastmilk Containing Methadone Author: Ballard Setting: Children’s Hospital, Cincinnati, OH Sample: 6 infants exposed to methadone Observations: 1.Feeding breastmilk associated with withdrawal symptoms 2.Frequent small doses from breastmilk shown to be more effective than large dose 3.Breastmilk may be most effective method in providing methadone to infants J Perinal Neonat Nurs 2002;15(4):76 53 Nutrition and Detoxification “Nutrition intervention, provided by a qualified dietetic practitioner is an essential component of the treatment and recovery from chemical dependency.” American Dietetic Association Position Statement - 1990 54 Nutrition and Detoxification Assess nutritional status Obtain weight history GI disturbances Adequate fluids Regularity of meal times Taste and presentation important Avoid substitute addictions!! 55 Multidisciplinary Team Physicians Psychiatrists/psychologists Case managers Nurses Social workers Mental health/behavioral health workers Substance abuse counselors Dietetic practitioners ? 56 Nutrition Education is Positively Associated with Substance Abuse Treatment Program Outcomes Author: Grant et al Setting: Cross-sectional survey Sample: 152 registered dietitians Outcome: 1. Positive associations found when nutrition education services incorporated into substance abuse tx programs 2. Group education/substance abuse education improved ASI scores improved 3. Individual nutrition/substance abuse education ASI scores improved by 99% (P<.05) J Am Diet Assoc 194;94(9):999 57 Brief Intervention 10 – 15 minutes sessions of counseling delivered by non-alcohol abuse specialists Shown to be low cost, effective treatment alternative for alcohol use Uses time-limited, self-help strategies to promote reductions in alcohol use in nondependent individuals or to facilitate referral to specialized treatment programs in alcohol-dependent persons 58 Brief Intervention for Alcohol Use by Pregnant Women Author: O’Connor, Whately Setting: WIC Program in Southern California Sample: 250 pregnant women who reported drinking alcohol Outcome: 1. Women in brief intervention group were 5x more likely to report abstinence after intervention 2. Newborns from brief intervention had higher birth weights and birth lengths 3. Fetal mortality rates were 3x lower (0.9%) in intervention group 4. In both groups, women reduced their drinking substantially Am J Public Health 2007;97:252 59 Summary Use of legal and illegal substances can affect the nutritional status in pregnancy Positive nutrition may improve pregnancy outcome All pregnant substance abusing should receive comprehensive nutrition assessment and counseling by a qualified dietetic practitioner Nutrition services and education should be part of the multidisciplinary care Breastfeeding not totally contraindicated in substance use 60