Water Balance
advertisement

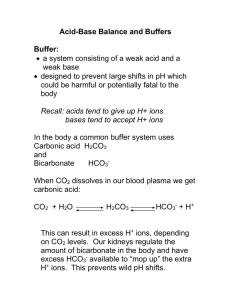
Body Fluids A. Body water content 1. Water is the largest single component of the body A) Early embryo = 97% water B) Newborn infant = 77% water C) Adult male = 60% water D) Adult female = 54% water E) Elderly adult = 45% water B. Fluid compartments 1. Intracellular fluid compartment (ICF) = 25L 2. Extracellular fluid compartment (ECF) =15L A) divided into two sub-compartments: 1) Plasma – fluid portion of blood = 3L 2) Interstitial fluid – the fluid in the spaces between cells = 12L 3. Other = lymph, cerebrospinal fluid, humors of the eye, synovial fluid, serous fluids, and secretions of the gastrointestinal tracts C. Major Components of Body Fluids 1. Water – 79-85% 2. Proteins – 10-20% 3. Lipids – 2% (adipose tissue itself has ~95%) 4. Carbohydrates – 1% 5. Electrolytes – substances that dissociate into ions when dissolved in water A) Major Cations 1) Na+, K+, Ca++ B) Major Anions 1) Cl-, HCO3-, HPO4D. Comparison of ECF & ICF ECF ICF 7.35-7.45 7.35-7.45 glucose fatty acids amino acids Gases higher higher higher used up immediately used up immediately used up immediately oxygen carbon dioxide Ions higher lower lower higher Na+ & Ca++ Cl- & HCO3- K+ HPO4- pH Nutrients cations anions Water Balance A. To maintain proper water volume, the body must balance water losses (both obligatory and nonobligatory) with water gains over the course of the day 1. To remain properly hydrated, water intake must be equal to water output (~2500ml/day) B. Water Output 1. Water output (loss) can be divided into 2 categories: A) Nonobligatory 1) water loss beyond that created by normal homeostatic events; not necessary to maintain homeostasis, and may or may not be avoidable 2) includes excess perspiration due to exercise, strenuous work, etc.; also includes vomiting and diarrheal illnesses 3) vary from person to person, hard to measure, and are generally not calculated into a person’s “normal” daily water loss B) Obligatory 1) water loss created by normal homeostatic events; necessary to maintain homeostasis, and are unavoidable and necessary to maintain life 2) fall into 1 of 2 categories: a) Insensible losses i) Skin (16%) ii) Lungs (12%) b) Sensible losses i) Urine (60%) ii) Sweat (perspiration) (8%) iii) Feces (4%) 3) The kidneys are responsible for our largest obligatory water loss each day a) They must produce at least a small amount of urine each day because: i) They must remove unnecessary blood solutes to maintain normal blood homeostasis ii) They must then flush those solutes out of the body in water (as opposed to in solid form) b) Failure to do so would result in improper blood composition which, in turn, could lead to imbalances/disease/death of other tissues in the body c) Beyond the homeostatic minimum, the solute concentration and volume of urine excreted depend on fluid intake, diet, and water loss via other mechanisms C. Water Intake 1. Varies greatly from person to person, and is often dependent on diet, lifestyle, activity level, etc. 2. Major sources of water intake: A) Liquids (60%) B) Solid foods (30%) C) Metabolic water (10%) 3. Regulation of Water Intake: thirst mechanism A) Increased plasma osmolarity (high solutes) or decreased plasma volume triggers the thirst mechanism, which is mediated by hypothalamic osmoreceptors B) When osmoreceptors lose water by osmosis to a hypertonic ECF, the hypothalamic thirst center is stimulated motivating the individual to drink C) Thirst is inhibited by distention of the GI tract by ingested water and then by osmotic signals 1) May be dampened before the body needs for water have been met Homeostatic Imbalances A. Dehydration – water loss exceeds water intake over a period of time 1. May result from hemorrhage, severe burns, vomiting, diarrhea, profuse sweating, water deprivation, or diuretic abuse B. Hypotonic Hydration – excessive water build up in the cells causing them to swell 1. Particularly damaging to neurons 2. May result from excessive water intake in a short period of time or renal insufficiency C. Edema – accumulation of fluid in the interstitial spaces, leading to tissue swelling 1. May result from increased blood pressure and capillary permeability, hormones, blockage of the lymphatic vessels, or low plasma proteins as a result of glomerulonephritis, malnutrition, or liver disease Acid-Base Balance A. Recall the definitions of acids and bases: 1. Acids (pH 1-6.9) – release H+ when in solution; often called hydrogen donors 2. Bases (pH 7.1-14) – release OH- when in solution; often called hydrogen acceptors B. The homeostatic pH range of arterial blood is 7.35 to 7.45 1. Higher pH = alkalosis 2. Lower pH = acidosis C. Abnormalities of Acid-Base Balance 1. Respiratory acidosis is the result of an increase in CO2 in the blood A) may be caused by hypoventilation (for any reason), when there is airway obstruction (ex. asthma), or due to alveolar dysfunction (ex. pulmonary edema) B) Increased CO2 = increased H+ = decreased pH 2. Respiratory alkalosis is the result of a decrease in CO2 in the blood A) May be caused by hyperventilation (for any reason) or mechanical ventilation B) Decreased CO2 = decreased H+ = increased pH 3. Metabolic acidosis is due to a decrease in HCO3- which lowers pH A) May be caused by excessive alcohol consumption, prolonged diarrhea, renal dysfunction, hyperkalemia B) Decreased HCO3- = decreased pH 4. Metabolic alkalosis is due to an increase in HCO3- which increases pH A) May be caused by excessive vomiting, hypokalemia, or excessive NaHCO3 (sodium bicarbonate; ex baking soda & some antacids) consumption B) Increased HCO3- = increased pH D. Chemical Buffering Systems 1. Work by replacing a strong acid with a weak one or a strong base with a weak one to minimize the pH change in the body fluid 2. Responsible for immediate changes to pH 3. 3 examples A) Bicarbonate buffer system – ECF; utilizes NaHCO3 (sodium bicarbonate) and H2CO3 (carbonic acid) 1) NaHCO3 functions as a weak base 2) H2CO3 functions as a weak acid 3) when a strong acid is added to the solution, NaHCO3 dissociates to form HCO3 and Na+ a) HCO3 binds with excess H+ create H2CO3 (weak acid) eliminating large amounts of H+ from the solution and preventing a drastic drop in pH 4) when a strong base is added to the solution, H2CO3 dissociates to form HCO3- and H+ a) HCO3 binds with the Na+ to form NaHCO3 (weak base) and preventing a drastic rise in pH b) H+ binds with excess OH- to create H2O eliminating large amounts of OH- from the solution and preventing a drastic rise in pH B) Phosphate buffer system – urine & ICF; utilizes Na2HPO4 (disodium monohydrogen phosphate) and NaH2PO4 (sodium dihydrogen phosphate) 1) Na2HPO4 functions as a weak base 2) NaH2PO4 functions as a weak acid 3) when a strong acid is added to the solution, Na2HPO4 dissociates into NaHPO4 and Na+ a) NaHPO4 binds with excess H+ to create NaH2PO4 (weak acid) 4) when a strong base is added to the solution, NaH2PO4 dissociates into NaHPO4 and H+ a) NaHPO4 binds with the Na+ to form Na2HPO4 (weak base) b) H+ binds with excess OH- to create H2O C) Protein buffer system – plasma & ICF; utilizes carboxyl and amine side groups on amino acids 1) Most abundant chemical buffering system in the body 2) Utilizes the carboxyl group or amine group from an amino acid a) alkalosis – rising pH (decreasing H+) results in the release of H+ from -COOH i) causes H+ levels to rise = decreased pH b) amine – dropping pH (increasing H+) causes excess H+ to bind to NH2 NH3 i) causes H+ levels to drop = increased pH E. Physiological Buffering Systems 1. Respiratory Control A) responsible for minute-to-minute changes in pH B) Utilizes bicarbonate reaction 1) recall CO2 + H2O H2CO3 HCO3- + H+ C) Driven by CO2 levels 1) Decreased pH (acidosis) causes increased ventilation; pushes the reaction to the left (decreased CO2 = decreased H+ = increased pH) 2) Increased pH (alkalosis) causes decreased ventilation; pushes the reaction to the right (increased CO2 = increased H+ = decreased pH) 2. Renal Control A) The kidneys provide the major longterm mechanism for controlling acid-base balance B) In addition, metabolic acids (phosphoric, uric, lactic, and keto) can only be eliminated by the kidneys C) Works by creating/reabsorbing or secreting (excreting) HCO3- D) Utilizes bicarbonate reaction 1) Tubule cells are impermeable to HCO3 on their tubule borders but not on their vascular borders a) Therefore, HCO3- is continually lost in urine b) Blood HCO3- levels are controlled by the bicarbonate reaction within the tubule cells i) To counteract acidosis, HCO3- is produced and reabsorbed resulting in more H+ secretion ii) To counteract alkalosis, HCO3- is produced and secreted resulting in more H+ reabsorption