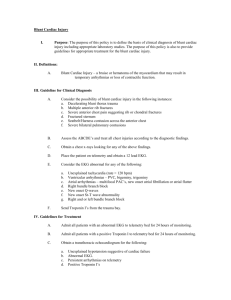
Traumatic Cardiac Injuries (11 Mar 2009)
advertisement

TRAUMATIC CARDIAC INJURIES SHORT CASE STUDY HENNIE LATEGAN CASE HISTORY • 25 YEAR OLD, PENETRATING STAB TO THE CHEST (6th intercostal space, 1.5cm left lateral to sternum) • BP: 70 systolic • Pulse: poor volume, 65bpm • GCS: 12/15 • Ward Hb: 7g/dl • Fluid challenge: 3 litres of lactated ringers plus 500ml of voluven. Poor response to resucitative efforts. • Heart sounds: muffled WHAT NOW? • If at GSH C14: Thoracotomy of course! • Tygerberg Trauma? Argue with the nurses as to indications, outcome, yes they do it at C14 and yes you are able to possibly do it. • Victoria Hospital: “Thora…..what? No no no Dr. over here we transfer to GSH C14.” • GF Jooste: “well the nurse who normally does it is on tea, but I will help you” General Cardiac Injuries • Blunt cardiac injuries • Penetrating cardiac injuries Blunt Injuries • Cardiac contusion commonest • Usually partial thickness injury as rupture is fatal • High speed deceleration • Often assoc. with rib fractures, sternal and thoracic spine fractures. • Clinical Features: – Low BP with Bradycardia – Raised JVP – Arrhythmias, MI type syndrome – Tamponade • ECG Changes – S-T segment raised or depressed – Q waves in anterior leads – Brady or Tachyarrhythmias Penetrating Injuries • Several presentations: – Exsanguinating haemorrhage – Tamponade group – Asymptomatic cardiac injury Pericardial included in Penetrating • 1. Unstable cardiac tamponade • 2. Stable cardiac tamponade • 3. Asymptomatic/Subclinical pericardial injuries Commonest cause is a precordial stab. • Clinical Features – STABLE TAMPONADE • PERIOD OF HYPOTENSION • REVERSED WITH 500-1000ML OF CRYSTALLOID • BUT ELEVATED CVP/JVP • Unstable Cardiac Tamponade – Shock with hypotension and tachycardia – Dyspnoea – Raised venous pressures: JVP/CVP – Pulsus paradoxus Unreliable: distant heart sounds and impalpable apex. • Subclinical Pericardial Injuries – – – – – – Pericardial rub Pneumopericardium Raised ST J waves Straight left cardiac border Globular heart – Note: ECG screening tool – U/S no value, no fluid present INDICATIONS • • • • The patient fits into 1 of 3 groups 1. Accepted indications 2. Relative indications 3. Contraindications • This decision needs to be made very quickly. • Some of the following slides may help! Gunshot Chest Underground Rock Fall Gunshot Chest Stab Back Gunshot neck with cardiac injury Crush injury Blunt chest trauma, MVA Accepted Indications • PENETRATING – Traumatic arrest with previously witnessed cardiac activity (pre-hospital or in-hospital) – Unresponsive hypotension ( systolic < 70 ) • BLUNT – Unresponsive hypotension (systolic < 70) – Rapid exsanguination from chest tube (>1500ml) Relative Indications • Penetrating thoracic – Traumatic arrest without previously witnessed cardiac activity. – Penetrating non-thoracic • Traumatic arrest with previously witnessed cardiac activity. (pre-hospital or in-hospital) • Rel. Indications Cont’d. • Blunt Thoracic Injuries – Traumatic arrest with previously witnessed cardiac activity. ( pre-hospital or in-hospital) Contraindications • Blunt Injuries: – Blunt thoracic with no witnessed cardiac activity – Multiple blunt trauma – Severe head injury So did this patient fit the criteria? • Yes. • Ultrasound machine was on hand to confirm Dx. • Cardiac Ultrasound video What other diagnostic modalities could be used? • ECG • Diagnostic pericardiocentesis • CT What ECG changes? • Penetrating – Electrical alternans – J waves( more pericardial injury) • Blunt – – – – – MI changes Multiple PVC’s Sinus tachycardia Atrial fibrilation Bundle branch blocks • Previous slide: Electrical alternans • Next slide: J waves So we have the criteria, why actually do it? what is the evidence?” • Survival is btw. 4-33% (protocol dependant) • GSH: 50% survival for penetrating Blunt trauma: survival rates: 0-2.5% • Stab wounds: Greater survival than gunshot wounds. • Isolated thoracic stab wounds causing cardiac tamponade highest survival rate: 70% Blunt? Should it be done? • According to literature, YES • When? – Isolated blunt trauma undergoing arrest in the A&E Debate: arresting in the prehospital setting. Location of the cardiac injury • Most survivors are of the isolated injury type • Cardiac highest survival rates • Great vessels poor • Pulmonary hila even poorer Back to the patient • A supine anterolateral thoracotomy was performed. • Video of procedure to follow Briefly the step by step • If the patient is reasonably stable: – – – – – – – – CVP insertion Intubation/RSI Peripheral IV CXR Chest Drain Cross match 4 units blood Ultrasound Subxiphisternal window to look directly if no US • Incision: Left anterolateral. 5th intercostal space from the nipple to the ant/mid axillary line. • Rib retractor to open up • Enter the 5th interspace and open the pericardial sac longitudinally • Note: anterior to the phrenic nerve • Once open scoop out the clot • • • • Usually a clinical improvement is evident Locate the ?hole in the heart Place a finger in the hole Either insert foleys catheter with 5mls of saline or suture close. • Prolene thread • Pledgets of dacron can be used • Avoid coronary vessels when suturing • Check for through and through wounds • Tie off internal mammary if it has been cut • Look for any other injuries • At GSH the patients if they have survived are taken to theatre for closure of the thoracotomy. Incision and pericardial splitting Rib retraction/suturing Pericardial opening Pledgets Cross Clamping • The patient in the video survived and walk out of the unit 6 days later. References • 1.Emergency Department Thoracotomy: Karim Brohi, trauma.org 6:6, June 2001 • 2.Trauma Manaul: UCT 2002 Edition. Editor Peter Bautz 3.ATLS Student course manual, 7th Edition 4.Atlas of Emergency Medicine, Peter Rosen MD 5. Basic surgical skills manual, Royal College of Surgeons, 2007