51'oUL cUoa
advertisement

Biochemistry Practical Notes
Authors:
Ida Fakla Péter Ferdinandy Janos Fischer
Gyorgyi Jakab —.. ^Margit Keresztes
Zsuzsanna Kiss ' Im re Ocsovszki Janos Rohan
Marianna Török Erno Zador ^
Editors:
Laszlo Dux Zsuzsanna Kiss
Reviewer:
Dr. György Falkay associate professor
Albert Szent-Györgyi Medical University
Department of Biochemistry 1995
Contents
Safety regulations .....................................................................................................
Substrate specificity and temperature optimum of Amylase enzyme
activity ...................................................................................................................
Determination of albumin in serum ....................................... ................................
Determination of total protein in serum..................................................................
Assay of the activity of Alkaline Phosphatase ..........................................................
Practical enzyme kinetics .........................................................................................
Determination of Glucose-6-phosphatase activity in rat liver.................... ...........
Enzymatic-colorimetric assay of urea in human serum ..........................................
Detection of the oxygen consumption of isolated mitochondria by
methylene blue reduction ......................................................................................
Serum protein electrophoresis ............................. ...................................................
Determination of orosomucoid concentration in human serum with
immunonephelomctry ...........................................................................................
Determination of uric acid concentration in serum ................................................
Determination of triglycerides in serum ..................................................................
Principle of dry chemistry diagnostic tests ..............................................................
Determination of serum bilirubin ............................................................................
Determination of enzyme activity ............................................................................
Fixed-time (Two-point) assay of the a-Amylase enzyme ............................
Kinetic assay (Multipoint, Continuous Monitoring) of Aspartate
Aminotransferase and Alanine Aminotransferase enzymes ...................
Determination of serum calcium, potassium, and chloride ion
concentration.........................................................................................................
Enzymatic determination of blood glucose level ....................................................
Assay of glycosylated haemoglobin ..........................................................................
Safety regulations
1. It is compulsory to wear labcoats during practices. Coats and bags etc. are to be kept in the
wardrobe on the corridor during practices.
2. Laboratory equipment, chemicals and samples must be used as described in the protocol.
3. Spilling or splashing any chemicals or samples is prohibited. Contact of the
chemicals/samples with the skin (inhalation, contact with eyes or swallowing) should be
prevented.
4. Harmful chemicals (concentrated acids, oc. bases, organic solvents and toxic materials)
are to be handled with special care, following the safety instructions. When such materials
are in liquid form, only automatic pipettes or glass syringe dispensers are allowed. Before
sampling or dispensing, proper operation of the pipette must be checked (no dripping is
allowed).
Should the above chemicals get into contact with the skin, it has to be removed
immediately with plentiful water. When spilled on clothes or onto lab equipment it has to
be removed immediately with towels or tissue paper (while wearing gloves). Upon contact
of the chemicals with the eye, the eye must be rinsed using a neutr alizing solution and/or
plentiful water, and the supervisor must be notified.
5. Extreme care must be taken when handling human samples because of the potential risk
of infections. In addition to the above general rules, all manipulations must be done using
gloves and the prescribed disinfecting handwashes are compulsory.
6. Laboratory glassware is fragile and might cause injuries. Should any injuries occur, the
supervisor must be notified in order to obtain appropriate treatment of the injury.
7. Smoking, eating and pipetting by mouth is strictly forbidden in the laboratory. Fire
precautions
1. After using Bunsen-burners (to prepare boiling water-bath) gas valves both under the
fume hood and the mains must be returned to the closed position.
2. Use of electric equipment in improper condition is forbidden. Upon finishing the work in
the lab, electric switches (on the benches etc.) must be turned off.
3. Students should be familiar with the location and the mode of the operation of the
fire-extinguisher.
4. Electric fires must not be "put out" with water. Proper fire-extinguishers are to be used or
the air supply to the fire should be blocked, if possible (e.g. using textile) or else.
5. Routes in the lab as well as exits must be kept free, unblocked!
Substrate specificity and temperature optimum of Amylase enzyme
activity
Amylase (1,4-a-glucosidase) is responsible for the enzymatic hydrolysis of alimentary
starch. In the hydrolytic reaction disaccharide units (maltose) are removed from the
unbranched glucose chain termini of starch. Amylase is also capable of hydrolyzing glycogen,
though this polysaccharide is not considered to be an important nutrient (glycogen, while
present as a minor component of white muscle cells, is rapidly decomposed during food
processing).
In the alimentary tract, the breakdown of polysaccharides is initiated by the amylase of the
saliva. This is followed by a more effective and complete pancreatic amylase hydrolysis in the
small intestine. Amylase, in low concentration, can be traced in blood serum. Due to its
molecular mass (Mw: 50 000), amylase readily appears in kidney filtrate and urine. Elevated
activity of amylase in serum and urine indicates diseases of the pancreas (acute pancreas
necrosis) or the salivary glands.
In this practical demonstration we use amylase as a model enzyme to show the influence
of temperature on catalytic activity. We also compare the efficiency and specificity of enzymatic
versus acidic hydrolysis of starch.
Principle
Amylase activity can be detected by thc Fehling reaction, which is based on the
measurement of reducing sugar released by enzymatic hydrolysis. Undegraded starch is
traceable by iodine colour reaction.
Materials
- Amylase solution: is obtained by extraction from germinating barley seeds
- Iodine reagent: 2% KI and 1% I2 in aqueous solution
- Fehling I reagent: 4% CUSO4 solution
- Fehling II: 20% K-Na-tartarate + 15% NaOH solution
- 1% starch solution
- phosphate-citrate buffer solution, pH 6.8 (0.2 M Na2HPC>4 and 0.1 M citric
acid in 7.7:2.3 volume ratio)
- 10% H2S04 solution
- 20% NaOH solution
- 1% sucrose solution
- 20% sulfosalicylic acid
The influence of temperature on the enzymatic and acidic hydrolysis
of starch
Procedure
Dispense the following amounts of reagents into 6 test tubes in the order given below.
Table 1.
test tubes
reagents (ml)
1
2
3
4
5
6
starch
2
2
2
2
2
2
buffer
5
5
5
-
-
-
< ;£Kfmin. preincubation (°C)
amylase
10% h2so4
0
37
100
0
37
100
1
1
1
-
-
-
-
-
-
6
6
6
37
100
-
-
15 min. incubation (°C)
20% sulfosalicylic acid
0
37
100
0.5
0.5
0.5
0
n
Incubation time is counted from the point of the addition of the enzyme solution or
H2SO4; the enzymatic reaction is stopped by addition of 20% sulfosalicylic acid.
Divide the content of each test tube into two equal portions.
To one part add Fehling I and Fehling II reagents. Since the reaction requires alkaline
conditions, 20% (w/v) NaOH solution should be added to adjust the pH of H2SO4
-containing (4 to 6) tubes (till the colour of the solution turns blue; approx. 3 ml NaOH is
required).
Table 2.
test
tubes
reagents (ml)
1/A
2/A
3/A
4/A
5/A
6/A
Fehling I
1
1
1
1
1
1
Fehling II
1
1
1
1
1
1
-
-
-
3
3
3
20% NaOH
5 min. incubation at 100°C
(boiling waterbath)
Compare the intensity of the colour reactions. (It is proportional to the extent of starch
hydrolysis).
To the other part of the reaction mixture 1 to 6 add iodine reagent as follows:
Table 3.
test
tubes
reagents (ml)
1/B
2/B
3/B
4/B
5/B
6/B
iodine
1
1
1
1
1
1
Mix well and compare the intensity of the colour reactions (this is proportional to the
amount of starch present).
Evaluation
By comparing the results obtained with the Fehling and iodine reactions determine the
optimal conditions of enzymatic versus acidic hydrolysis. Write down the possible
explanation of the results.
Analysis of Ihc substrate specificity of the enzyme
Procedure
Dispense the following reagents in 4 test tubes in the order given below: Table 4.
test tubes
reagents (ml)
1
2
3
buffer
5
5
-
-
starch
2
-
2
-
sucrose
-
-
2
2
4
10 min. preincubation (°C)
amylase
10% H2SO4
37
37
1
1
-
-
100
100
-
-
6
6
15 min. incubation (°C)
20% sulfosalicylic acid
37
37
100
100
0.5
0.5
-
-
Divide the content of each tube evenly as done earlier. With half of the reaction mixture
perform the Fehling reaction. Table 5.
test tubes
reagents (ml)
1
2
3
4
Fehling I
1
1
1
1
Fehling II
1
1
1
1
20% NaOH
-
-
3
3
5 min. incubation at 100 °C
Evaluation
Compare the efficiency of enzymatic (amylase) and acidic hydrolysis of starch and
sucrose . Interpret the results in terms of specificity.
-y -
- 9-
Dctcrmination of albumin in serum
Introduction
Albumin makes up about 60% of the loial plasma proteins. It has two important
biological functions: It is responsible for 75-80 % of colloid osmotic or oncotic pr essure of
the plasma, and it is the most important carrier protein.
Because of diminished synthesis, plasma albumin levels fall in any chronic illness. Very
low levels arc often found in patients with advanced hepatocellular disease and in patients
with conditions in which diminished synthesis is accompanied by loss of large amounts of
albumin into the urine (nephrosis) or into the gastrointestinal tract (protein-losing
enteropathies).
Principle
Bromcresol green binds to albumin specifically forming a green colored complex in the
presence of Brij 35.
Color reagent:
Dist. water
Glycine solution (1 M) HCI (1
N) Brij 35 (30%)
1600
ml 189
Bromcresol green stock
ml
I 1 ml
solution
8 ml 6
ml
Procedure
Introduction
- 10-
Dispense in the test tubes the following amounts of solutions:
test tubes
reagents
1
sample
2
standard
3
blank
color reagent(ml)
5
5
5
serum(pl)
50
-
-
standaid(pl)
-
50
-
dist. water(jil)
-
-
50
15 min. incubation at 25 °C
Measure the absorbance of sample and standard at 625 nm.
Evaluation
-^sample
x
^--standard = ^serum (S^O
^-standard
A = absorbance C =
concentration
me>r<£ S-pocî cc
CQ^OJ
(hOi^xhc
§51'oUL cUoa^
c_
yiOl- <oidu p o k lu** (jKUu^ i u O K d r f i ' SioU CUClal^
QjbunX^^
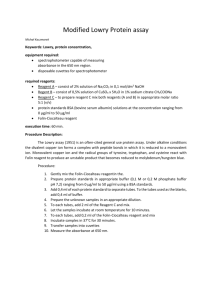
Determination of total protein in serum (Lowry method)
Plasma proteins serve a number of different functions in the organism. Not only the
relative amount of plasma protein fractions but the total protein content can undergo a
change depending on the different disease states. A large number of methods are available for
determination of plasma proteins and they are different in their sensitivity and specificity.
The commonly used spectrophotometric methods are based on the change of absorbance
resulting from the interaction of the reagents with peptide bounds or certain amino acid
residues. Some examples are as follows:
- Biuret reaction - Substances containing peptide linkages give a violet coloration with the
reagent. The method is of low sensitivity, but it is not affected by free amino acids.
- Lowry method - The intensity of color formed is due to the reduction of phosphomolybdate
by Tip and Tyr present in the proteins. The method is fairly sensitive, but free amino acids
inteifere with the reaction.
- Bradford reaction - The color reagent binds to basic (especially Arg) and aromatic 1 amino
acid residues giving a blue color complex. A reliable method of high sensitivity and specificity.
Principle
The method is based on the color reaction of the Folin reagent (phosphotungstomolybdic
acid) with Trp and Tyr side chain of proteins.
Materials
Sol."A": 4% Na2C03 in 0.2N NaOH
Sol."B": 1.1% CUSO4 x 5H20, 2.2% K-Na tartarate in 1:1 ratio Sol."C":
"A" and "B" Sol. in 50:1 ratio
Folin reagent (dilute with dist. water in 1:1 ratio before use)
distilled water
protein standard: 1 mg/ml
diluted serum
phosphate buffer (pH:7.2)
Procedure
Dilute the Folin reagent with distilled water in 1:1 ratio
Prepare Sol."C" by mixing Sol."A" and Sol."B" in 50:1 ratio Dispense
Introduction
- 12-in the test tubes the following amounts of solutions
test tubes
1
2
3
standard(jil)
10
50
100
dil. serum(pl)
-
-
-
-
-
-
-
-
-
-
reagents
phosphate buffer(pl)
dist. water(jjl)
Sol. "C" ml)
4
5
150
200
6
7
-
-
200
-
-
200
590
550
500
450
400
400
400
3
3
3
3
3
3
3
300
300
10 min. preincubation at 25 °C
dil. Folin reagent(fjl)
300
300
300
300
300
30 min. incubation at 25 °C
Measure the absorbance of the samples at 710 nm
Evaluation
Make a calibration curve using the values obtained with standards (1-5. test tubes),
(abscissa: protein standard concentration fpg/mlj, ordinate: measured absorbance).
Use this curve to determine protein concentration of the diluted serum (6. test tubes).
Assay of the activity of Alkaline Phosphatase
Introduction
represent a group of enzymes, which hydrolyze phosphate esters
- 1 3Phosphatases
-»
(phosphatides, carbohydrate phosphoric acid esters, glycerophosphoric acid, nucleotides).
According to their pH-optima phosphatases are classified as alkaline or acidic phosphatases.
They are activated by
and Mn2+ ions, while enzyme
activity is hindered by Zn2+, Bc2+, PO43", ASO43", CN~, oxalate, citrate ions, and thiol
compounds. Both groups have a fairly broad substrate specificity, thus they are capable of
hydrolyzing a variety of physiological and nonphysiological substrates, like glycerol phosphate
and p-nitrophenyl phosphate, which are widely used in in vitro enzyme assays.
Phosphatases are involved in bone matrix formation, polysaccharide and protein
biosynthesis of the connective tissue, in nucleic acid metabolism, in regulation of glycogen
metabolism and signalization processes taking place in membranes. Serum alkaline
phosphatase activity is the result of different isoenzymes of intestinal , placental, liver, kidney,
and osteoblast origin. A physiological increase of enzyme activity occurs in pregnancy, while
both severe starvation and protein-rich diet result in decreased activity. Certain pathologic
conditions, like certain bone and liver t diseases (especially those involving biliary
obstruction) and recovery from bone fractures are associated with increased phosphatase
activity. Enzyme activity of the serum is decreased in hypothyreosis and during osteoblast
damage.
In this practical, the dependence of enzyme activity on substrate concentration is studied
by using the alkaline phosphatase (ALP) as a model system.
Normal value (in human serum)
adult: 13-45 U/l
infant (2 to 12 months): 40-160 U/l
(One unit [U] of alkaline phosphatase activity is, defined as the activity of enzyme which
produces reaction in 1 pmole of substance in 1 minute under defined conditions. The values of
enzyme activity are referred to 1 liter serum.)
Principle
p-Nitrophenyl phosphate is hydrolyzed by alkaline phosphatase. The resulting p-nitrophenol, which is yellow in alkaline medium , can be quantified by spec troph otometry.
Materials
- alkaline buffer solution (pH 10.5; 220 mM Tris(hydroxymethyl)aminomethane, 5.5 mM
MgCl2)
- 14 -
- substrate, 55 mM p-nitrophenyl phosphate (Mw. 371.1) stock solution
- 0.2 M NaOH solution
- blood serum
Procedure
We will make a bisecting dilution series from the stock substrate solution as follows: Pipette
1 ml of the stock solution (55 mM p-nitrophenyl phosphate) into the first tube (1/a). Then
pipette 0.5 ml of distilled water into the tubes marked 2/a, 3/a, 4/a and 5/a, respectively. Then
take out 0.5 ml of the stock solution from the first tube (1/a) and put it into the second tube
(2/a). After thorough mixing the p- nitrophenyl phosphate concentration in this tube is the 1/2
of the original one, namely 27.5 mM. Pipette 0.5 ml of the diluted solution from the second tube
(2/a) into the third tube (3/a). As a result, the concentration of the mixed solution is the 1/4 of
the original concentration, 13.75 mM. Prepare 1/8 and 1/16 dilutions (6.87 mM; 3.43 mM) in the
same way. This substrate dilution series is used in alkaline phosphatase enzyme assay.
test tubes
reagents (ml)
1
buffer
0.7
corresponding diluted
0,1
2
3
4
5
0.7
0.7
0.7
0.7
0.7
0.1
0.1
0.1
0.1
-
-
-
0.2
0.2
- 15 -
6(blank)
substrate
dist. water
serum
-
0.2
-
0.2
0.1
0.2
-
15 min. incubation at 37°C
0.2M NaOH
serum
2
2
2
2
2
2
-
-
-
-
-
0.2
Mix the samples (tubes 1-5) again and determine absorbances (extinctions) at 400 nm.
Use control sample (tube 6) as a reference.
Evaluation
Absorbance values are proportional to the quantity of p-nitrophenol and the rate of the
enzyme reaction. Plot the results on graph paper indicating the measured absorbances (A)
as a function of concentrations of the substrate according to Michaelis-Menten. (All
substrate were diluted lOx, thus the concentrations are the follows: 0.343; 0.687; 1.37; 2.75
and 5.5 mM.) Evaluate the experimental results on the basis of Lineweaver-Bnrk and Direct
Linear Methods for comparison as well. (Theoretical bases and practical applications can be
found in the section of Practical Enzyme Kinetics:)
Practical enzyme kinetics
The Michaelis-Mcnten equation
According to Michaelis and Menten, the kinetics of enzyme catalysis can be
described with the following equation:
E+S
kx
k2
ES ------------ > E + T
k3
if and only the conditions numbered 1-5 are fulfilled.
where E — enzyme S =
substrate
ES = enzyme-substrate complex P =
product
kj, k2, = reaction rate constants
1. There has to be an ES temporary complex during the reaction.
2. The product P is not converted back to ES (therefore there is no k4 reaction constant). It can
be supposed because P is converted further at once in most reactions.
3. We observe the reaction only with one substrate (first order reaction) and consider only one
ES complex and one product to be formed.
The velocity of the reaction equals with the velocity of the product formation:
V = k2 [ES]
4. We suppose the reaction to be at steady state. This means that the [ES] is not hanging
because the speed of its formation and its breakdown are equal. (The situation is different at
the beginning stage of the reaction where more ES is formed than broken down.)
ES complex formed at Vf velocity and is broken down at V^ velocity:
Vf=ki [E] [S]
Vf = ki [E] [S]
Vb = k2 [ES] + k3 [ES] = (k2+k3) [ES]
Steady state means Vf = Vb
ki [E] [S] = (k2 + kg) [ES]
by rearranging the equation we get: [E] [S] k2 + k3
[ES]
ki
this is a new constant, called the Michaelis constant (Kjyj)
km=
k2 + k3
------kl
this includes the 3 reaction constants, [E] [S]
---------- =KM
[ES]
where [E] = free enzyme concentration: [E] = [Et] - [ES] [EJ = total
enzyme concentration
[S] = the actual substrate concentration equals with total substrate concentration
because 5. We suppose that free substrate concentration supersede many times that of the
enzyme linked one, so since enzyme
- 1 7 - concentration is relatively low compared to substrate
concentration, we always have surplus substrate.
To calculate enzymatic velocity (V = k2 [ES]), we have to determine the actual ES
concentration. On substituting [E] for [EJ - [ES]
( [Et] - [ES] ) [S]
-------------------------- =KM
[ES]
([EJ - [ES]) [S] = KM [ES] [Ed [S]
- [ES] [S] = KM [ES] [EJ [S]=KM
[ES] + [ES] [S] [Et] [S] = [ES] (
KM + [S] ) [Et] [S]
[ES] = ---------------KM + [S]
Now on substituting this into V = k2 [ES] we get
[Et] [S] V = k2
------------------------KM + [S]
Here only [S] is a variable.
Now let us examine when the maximal rate Vmax is attained. This is the case when the
enzyme active sites are saturated with substrate; in other words [S] is much greater than Km»
thus
[S]
[S] + Km
Since Vmax = k2 [Et],
= 1 (approaches 1)
Vmax
lEt[ [S]
substituting k2 = ------------- into the equation V = k2 ------------------lEt]
[S] + KM
we get
[S]
^ = ^max
- 19 -
[Si + Km
This is the Michaelis-Menten equation which with two constants accounts for the
relation of the rate of enzyme catalysis to the concentration of substrate.
The Michaelis-Menten equation describes a hyperbole where Vmax is the
asymptote of the curve, while Km is the concentration of substrate [S], having the
half of the maximal value of the velocity. This is evident, if we substitute Vmax/2
into the Michaelis-Menten equation:
[S]
^ max/2 = ^max
[S] + KM
by rearranging the equation
1=2[S]/(KM + [S]) KM + [S] = 2[S]
[S] = KM (when V = Vmax/2)
That is, Km is numerically equal to the substrate concentration, at which reaction rate is
half of its maximal value.
The Km value is a characteristic constant of the particular enzyme (isoenzyme). The lower
Km reflects to a lower substrate concentration, at which Vmax can be attained.
The conversion of the Michaelis-Menten equation to a Straight Line Plot
It is difficult to estimate Km and Vmax values from the hyperbolic Michaelis curve
graphically, since the asymptote can not correctly be determined. However, for determination
of Km the correct asymptote value is needed.
Exact graphical representation is possible, if we linear ize the original equation. There are many
different methods for doing this but we present only one here, the one called the Lineweaver
and Burk linearization. The method is based on the reciprocal transformation of the sides of the
Michaelis-Menten equation that gives a straight line plot.
1/V = (KM + [S])/
v max [S] 1/V = K /V
M
max [S] + 1/Vmax
Graphical representation means plotting 1/V as a function of 1/[S]. If our enzyme follows
the Michaelis-Menten kinetics, we get a straight line.
The slope is
The intercept on the y axis : 1/Vmax
The intercept on the x axis : - 1/Km
: i\M/Vmax
Because of the nature of this linearization
- 20V-max can be determined more correctly than Kjyj-
Direct Linear Method
The other method to determine Km and Vmax correctly is the so-called "direct linearization
method". Here we use the original Michaelis-Menten curve to generate a constant in the
following way.
We draw parallel lines with the x and y axis which run through the original determined
points, thus we get a series of rectangles. We draw the diagonal line from the lower right to the
upper left corner and extend it. All diagonal lines will intercept Vmax at the -Km- To prove this let
us take up a point on the x axis and let this point be at Km-
Fig. 1. Graphical Determination of Km Using the Direct Linear Method
abc and ABC triangles are equal because B =
Vmax
- 21
- /2 = b, so A = K^ Hence, this line will intercept
the Vmax asymptote at -Kj^j-
We can similarly prove it for any other point on the Michaelis curve. Let us now prove this at the
substrate concentration = 2Km» so
V=V
2KM
max
2 KM + K M
V = 2/3 Vmax
ma
x
K
M 2KM
The relation of triangles is:
Fig. 2. Determination of K^ at 2 Kj^ Concentration of the Substrate
(l/3)/(2/3) = a/(2KM)
b/B = a/A
1/2 =
a/2 KM a=
KM
Therefore, these diagonal lines intercept the Vmax asymptote at -Kj^j-
-22 -
Introduction
Determination of GIucose-6-phosphatase activity in rat liver
Glucose-6-phosphatase is an integral membrane protein of the endoplasmic reticulum
(ER), found mostly in liver, also in kidney, and in intestinal mucosa. The enzyme present in
liver is functioning by catalyzing the hydrolysis of glucose-6- phosphate originated from
glycogen catabolism and through this by maintaining constant blood glucose level. The
glucose-6-phosphatase system involves also 3 translocases apart from the enzyme, which allow
the transport of glucose-6-phosphate to the ER, or the efflux of inorganic phosphate or glucose
from the ER, respectively.
Physiologically, damaged or no activity of the enzyme can be shown in the plasma; in cases
of liver damage (hepatitis, cirrhosis) enzyme activity is increased in the plasma, while reduced
in liver. In type I/a glycogen storage disease (Gierke s disease) low blood glucose level is found
(fasting hypoglycemia) caused by the lack of the enzyme. Similar" symptoms are seen in type
I/b glycogen storage disease where glucose-6-phosphate translocase is missing. During long
fasting increased synthesis of glucocorticoid hormones bring about increased synthesis of
glucose-6-phosphatase.
Principle
The enzyme present in liver homogenate cleaves
inorganic phosphate from
glucose-6-phosphate; the amount of inorganic phosphate is determined by a turbidimetric
assay. Phosphate reacting with ammonium molybdate forms a phosphomolybdate complex;
adding Triton X-100 (a detergent) to the solution, turbidity will develop, the degree of which is
related to the concentration of the complex. EDTA and NaF (in the reaction mixture) inhibit the
activity of acidic and alkaline phosphatases.
Materials
- liver homogenate (rat liver homogenized in 3 vol buffer solution containing 10 mM Tris, 2
mM MgCl2, 30 mM NaCl, pH 7.3); used after a 5-fold dilution
- malate buffer solution (75 mM malate, 12.3 mM EDTA, 12.3 mM NaF pH 6.0)
- glucose-6-phosphate (diNa salt) (200 mM)
- 12% trichloracetic acid
- 1% Triton X-100
- 23 -
- 2.5% ammonium molybdate x 4 H20 in a solution containing 16.6% (v/v) conc. sulfuric
acid.
Be careful! Strong acid!
Procedure
Take 2 test tubes: 1 for the enzyme reaction (sample tube) and 1 for the determination of
inorganic phosphate present in the glucose-6-phosphate solution and in the liver
homogenate (control). Fill 0.55 ml malate buffer in all test tubes. Pipette 50-50 pi (5 x
diluted) liver homogenate to the sample and to the sample control tubes. (Before pipetting
shake the liver homogenate well!). Incubate all tubes for 5 minutes at 37 °C. Then add 2 ml
12% tr ichloroacetic acid to the control tube and 0.1-0.1 ml glucose-6-phosphate solution to
the sample and to the control tubes. Incubate for 15 minutes at 37 °C. Stop the reaction by
adding 2 ml cold 12% trichloroacetic acid to the sample tube. Then filter the contents of the
test tubes into 2 labelled short tubes.
Three long test tubes are labelled for the determination of inorganic phosphate (1
sample, 1 control, 1 blank). Deliver 0.4 ml filtrate to the appropriate tube, then add 5- 5 ml
dist. water to each. Prepare the blank one by adding 5.4 ml dist. water to a tube. Fill 60-60 pi
1% Triton X-100 in all tubes and mix well. Then add 0.6-0.6 ml ammonium molybdate
solution to all tubes and mix them again. Read absorbance 4 (against blank) at 620 nm 20
minutes later.
Table 1.
test tubes
- 24 -
1
sample
reagents
malate buffer(ml)
2
control
0.55
liver homogenate dil.(pl)
0.55
50
50
5 min. preincubation at 37 °C
12% TCA(ml)
2
-
glucose-6-phosphate(pl)
100
100
15 min. incubation at 37 °C
12% TCA(ml)
2
-
filtration
+
+
Table 2.
test tubes
1
sample
reagents
filtrate(ml)
2
control
3
blank
0.4
0.4
-
dist. water(ml)
5
5
5.4
Triton X-lOO(jil)
60
60
60
ammonium-molybdate(ml)
0.6
0.6
0.6
reading absorbance at 620 nm 20
minutes later
=
i
-
^
^
Calculation
Take the average of the absorbance values of the 2 samples, 2 substrate controls and 2
sample controls, respectively. Read the inorganic phosphate (Pj) amounts (in nmol)
corresponding to these absorbance values from the Pj calibration curve. Subtract the P^ values of
the substrate plus sample controls from the P^ value of the sample, thus we get ?\ liberated by
the enzyme.
Enzyme activity calculated for 1 ml diluted liver homogenate (nmol Pi / ml sample x
min):
Pi (nmol) x 6.75
- 25 -
diluted 0.05 ml homogenate x 15 min
Pi (nmol)
calculated for 1 hour: ------------------------------------------- x 60
diluted ml homogenate x min
calculated for the undiluted liver homogenate (diluted 5x):
Pi (nmol) x 5 —>
ml homogenate x h
volume factor:
final volume of reaction mixture 2.7ml ---- .= -------------- = 6.75
volume of filtrate used for Pi determination
0.4ml
If protein concentration of the liver homogenate is known, specific activity
corresponding to mg protein can be calculated: enzyme activity (nmol Pi / mg protein x
min):
Pi (nmol) x 6.75
protein quantity in 50 ul (in mg) x 15 min
This value can be calculated with, as described above; units in nmol Pj can be
converted to higher units.
¿Ul^lM A Staple : (So*- C f S r & ^ y
-
Z^li^t^
Introduction
Enzymatic-colorimetric assay
of urea in human serum
-26 -
Due to the degradation of nitrogen containing compounds, 80-90% of the total excreted
nitrogen gets into the urine as urea. Urea is synthesized in the liver in the "urea cycle"
consuming NH3, CO2, the amino nitrogen of aspartate, and ATP. This process detoxicates the
highly toxic ammonia formed by the metabolism of nitrogen compounds, and by the enteral
bacteria. In case of severe insufficiency of the urea cycle due to hereditary enzyme deficiency or
hepatic cirrhosis, the extrahepatic detoxication of the accumulated ammonia may lead to
metabolic disorders causing mainly neurological symptoms. High ammonia concentration and
low urea concentration in the plasma have great diagnostic value in this case. Elevated urea
concentration may be observed as a result of protein-rich diet, or enhanced protein degradation
that occurs in starvation or due to overproduction of glucocorticoid hormones. Insufficiency of
kidney function also leads to high urea concentration.
Principle
Urease cleaves urea producing carbon dioxide and ammonia in alkaline pH.
urea + H20 ------ > 2NH3 + C02
Ammonia is immediately converted to ammonium ion in aqueous solution. Ammonium
forms a green compound with salicylate and Na-hypochlorite in the presence of the catalyst
Na-nitroprusside. The intensity of the color measured at 600 nm wave length is proportional to
the concentration of urea in the range of 0 - 2 5 mmol/1.
Materials
Reagent 1.: urease powder
Reagent 2.: (phosphate buffer):
Na-salicylate (60 mmol/1)
Na-nitroprusside (3.5 mmol/1)
EDTA (1.31 mmol/1)
Reagent 3.: Na-hypochlorite (45 mmol/1)
NaOH (1 mmol/1) Standard:
mmol/1)
Sample:
serum, or heparinized plasma
urine (100 times dilution)
urea (8.325
Procedure
test tubes
-27-
reagents
1
sample
2
standard
3
blank
1.+2. reagent(ml)
1
1
1
dist. water(jil)
-
-
10
standard(jil)
-
10
-
10
-
-
sample(pl)
5 min. incubation at 25 C
3. reagent(ml)
1
1
1
15 min. incubation, then
measurement of absorbance at 600
nm
Calculation
[urea] (mmol/1) = (A sample / A standard) x [standard] (mmol/1)
-28-
Reagent 3.: Na-hypochlorite (45 mmol/1)
NaOH (1 mmol/1)
Standard:
urea (8.325 mmol/1)
Sample:
serum, or heparinized plasma
urine (100 times dilution)
Procedure
test tubes
reagents
1
sample
2
standard
3
blank
1.+2. reagent(ml)
1
1
1
dist. water(jil)
-
-
10
standard(pl)
-
10
-
10
-
-
sample(pl)
5 min. incubation at 25 C
3. reagent(ml)
1
1
1
15 min. incubation, then»
measurement of absorbance at 600
nm
Calculation
[urea] (mmol/1) = (A sample / A standard) x [standard] (mmol/1)
- 29 -
Detection of the oxygen consumption of isolated mitochondria by
methylene blue reduction
Mitochondria - as the organelles of intracellular respiration - produce high amount of
reduced coenzymes ( NADH+H+, FADH2 ) in mitosol during the breakdown of acetyl-CoA by the
enzymes of the citric acid cycle. The elections from these reduced coenzymes are transported to
molecular 02 by the enzymes of the electron transport chain localized in the inner mitochondrial
membrane. Under normal conditions this process is strictly connected with ATP production
which is regulated by oxygen as a substrate and even by the ATP/ADP ratio.
The velocity of the intracellular respiration depend therefore on the actual 0 2 supply and the
energy saturation of the cell.
Certain drugs or chemicals interfere with this regulation mechanism, either destroying the
proton (pH) gradient which exists between the matrix and the intramembranous space, or
blocking the transport of electrons which in turn is responsible for the generation and
maintenance of the proton gradient. Such chemicals are the so called uncoupling agents
(2,4-dinitrophenol, dinitrocresol, pentachlorphenol) arid enzyme inhibitors (barbiturate,
atractyloside, rotenone, antimycin, oligomycin, KCN).
Principles
Mitochondria are easily isolated from soft tissues (i.e. liver) and under physiological
conditions they remain functionally active for a longer period of time. The aim of this practice is
to demonstrate some functional aspects of intact mitochondria.
The oxygen consumption will be followed therefore suspension containing mitochondria and
substrates has to be overlayered by paraffin-oil to exclude further 02 supply. In this case the
available 02 content of the suspension equals to the amount of 02 which has been dissolved into
the medium from the air to its partial pressure at room temperature.
We will also add redox-indicator molecules to the suspension. Elections flowing through the
electron transport system of the inner mitochondrial membrane will reduce the dye molecules
into a colorless (leukomethylene blue) product, if molecular oxygen is no more available.
Materials
- mitochondria suspension (prepared from rat liver in isotonic solution)
- incubation solution: 20mM TRIS buffer pH 7.2 containing 8mM KC1, ImM EDTA, lOmM
KH2P04, 0.01 M Na-succinate
- solutions of lOmM 2,4-dinitrophenol, 0.1M KCN, 0.3M ADP
- 0.5% methylene blue
- 30 -
Procedure
test tubes
reagents (ml)
1
2
3
4
incubation solution
4
4
4
4
mitochondrium susp.
1
1
1
1
-
0.2
-
-
-
-
0.2
-
Toxic!
KCN sol.
-
-
-
0.2
Toxic!
dist. water
0.2
-
-
-
ADP sol.
dinitrophenol
Remarks
Shake well before use!
After shaking, 2 min. preincubation 37 C at
methylen blue
0.1
0.1
0.1
0.1
Shake the mixture!
paraffin-oil
1
1
Put the meth. blue first
into the 4. tube. Shake well
and overlay with
1
1
paraffin-oil carefully!
incubation at 37 C
Check the tubes every 30 seconds and compare their colors!
Evaluation
Bleaching of methylene blue refers to the loss of dissolved 02 from the reaction mixture
which in turn is an indicator of an intact electron transport.
-31 -
Introduction
Serum protein electrophoresis
Protein molecules migrate in electric field. The migration is determined by their structure
and the pH of the solvent. The majority of proteins has isoelectric point (when the molecule is
neutral) around or under pH 7. In a moderate basic solvent (pH 8-9) the molecule dissociates
protons, it becomes negatively charged and migrates toward the positive electrode (anode).
Protein molecules with isoelectric point at basic pH are less frequent and move toward the
negative electrode (cathode), if the solvent has moderate basic pH. On a suitable carrier matrix
(filter paper, agarose, acrylamide, cellulose acetate) this feature can be utilized for electric
separation - for the electrophoresis.
The electrophoresis has been used in biological, medical research and in clinical diagnosis
for nearly thirty years. It is a basic method that has been developed into more sophisticated ones.
Here we introduce the basic principles of some of these methods.
Native electrophoresis
Protein isoforms occurring in a small quantity but having catalytic activity can be identified
by this method. After separation resulting in a relatively low resolution, enzymes can be stained
histochemically. Special gels like starch-agarose or cellulose acetate membrane are used to
preserve enzyme activity.
SDS-gel electrophoresis
Molecular weight of protein subun
stermined by electrophoresis. After
boiling with sodium-dodecilsulfate (SDS) and DTT that breaks the disulphide bounds, proteins
dissociate into subunits, become negatively charged and move toward the anode. The speed of
migration is inversely proportional to the molecular weight. The resolution can be improved by
repeating the electrophoresis among altered conditions (pH, gel concentration) into an other
direction.
Isoelectric focusing
Protein molecules are separated according to their isoelectric point on a gel carrying pH
gradient. Proteins migrate to the pH zone of their isoelectric point and stop there.
Immunelectrophoresis
The sample is applied to gel made with the antibody or the antibody is electrophoresed
toward the sample. At the zone where the proteins and the antibody form complexes
precipitation arches are formed. The place and size of these arches are evaluated quantitatively
and qualitatively.
Electrophoresis of nucleic acids
The separation of nucleic acid fragments is also made by electrophoresis in molecular
biology. Nucleic acids are macromolecules therefore must be digested by restriction enzymes
before electrophoresis. The length of the restriction fragments will characterize the nucleic acid
macromolecule or the chromosomal DNA. The linearized double stranded DNA fragments
migrate toward the anode at basic pH in 1% agarose . Single stranded nucleic acid molecules
have to be denatured for the electrophoresis. The electrophoretic mobility is in inverse
proportion with the size. The size of the fragments can be determined by standards.
Gel blotting
Protein molecules or nucleic acid fragments can be transferred to nitrocellulose/nylon
membrane from a gel after denaturation. Protein molecules are transferred by electric field,
while the nucleic acid fragments mostly by capillary * diffusion. The transferred molecules are
fixed to the membrane by heat, vacuum or UV irradiation. The membrane has the advantage of
keeping its size during the wetting and drying procedure. Proteins on the membrane can be
hybridized with antibodies - this is the Western blot. Blots made from nucleic acid gels are
hybridized with a nucleic acid fragment labelled with radioactive nucleotide. If the DNA
fragments are on the membrane that is the Southern analysis. If RNA fragments are on the
membrane that is the Northern analysis.
Protocol for the practice
This practical demonstrates the electrophoresis of serum proteins on a special ready made
agarose gel. Under these circumstances the protein molecules migrate according to the electric
charge and molecular size. The serum protein bands, in the order of their migration: the
albumin, the ct[ and ct2, the P-globulin and the y- -globulin - has clinical significance. Except
the albumin, each band contains multiple proteins. The ratio of these proteins might change in
diseases. Certain additional proteins might also accumulate in the serum in acute infections.
- 33 -
Use plastic gloves!
1. Open protective bag and blot the buffer from the gel.
2. Place template on gel, remove air bubbles and apply 5 pi of the diluted serum. Wait 5 minutes
until sample infiltrates the gel.
3. Remove template, center gel over bridge, squeeze and locate on paragon.
4. Pour 45 ml buffer into each cell reservoir, connect the chamber into the electric circuit and
electrophorese at 100 V for 25 minutes.
5. Place gel in frame and the frame into frame holder.
Keep the gel in:
6. Acetic acid-methanol for 3 minutes.
7. Drying oven (maximum 90 °C), dry gel completely, aprox. 30 minutes.
8. Blue stain solution for 3 minutes.
9. Acetic acid for 2 minutes.
10. Acetic acid-alcohol solution for 2 minutes.
11. Acetic acid solution for 2 minutes
12. Dry gel completely (maximum at 90 °C).
Gel can be scanned by densitometer at 600 nm. The ratio of serum proteins: albumin:
58.8-69,6%; globulins: cq: 1.8-3.8%; a2: 3.7-13.1%; P: 8,9-13,6%; y: 8,4- 18,3%; A/G ratio
1.39-2.23%. Ratios might be different in pathological samples.
- 34 -
Determination of orosomucoid concentration in human serum with
immunonephclometry
The major portion of plasma seromucoids has been recognized as orosomucoid (acid a
j-glycoprotein). Orosomucoid is an acute phase protein. Increased orosomucoid serum can be
observed in less than 24 hours after the tissue damage. Increases occur also in rheumatoid
arthitis, systemic lupus erythematosus, malignant neoplasms and in myocardial infarction.
Decreases occur in malnutrition, severe hepatic damage and severe protein-losing
gastroenteropathies.
Measurement range: ca. 0.2-3.0 g/1
Expected values: 0.3-1.1 g/1
Principle
Following dilution of serum, anti-orosomucoid antibody is added. The intensity of the
antigen - antibody reaction can be measured by nephelometry. This method is based on the
light-scattering properties of immun-complexes (precipitates) and the measured values correlate
with
the
amount
of
these
complexes.
Recorder
Light Source
Immunoprecipitate
----------- of
Analyte
- 35 -
Materials
- sample: serum
- buffer for the antibody solution
- blank buffer
- antibody solution
- calibrator solution
- 0.9 % NaCl solution (physiological salt sol.)
Procedure
Human serum is used for the determination of orosomucoid, therefore the use of
surgical gloves is required!
1. Antiserum buffer solution: pipette 500 pi antiserum reagent into the 30 ml buffer. Mix
gently. Solution is stable for 12 weeks when stored at +2-+8 °C.
2. Blank-buffer: ready to use.
3. Calibrator: dilute 1:51 (10pl+500pl) with 0.9% NaCl.
4. Sample: dilute 1:51 (10pl+500pl) with 0.9% NaCl.
5. Pipette into the cuvettes the following solutions (prepare the calibrator as a duplicate):
calibrator
calibrator test
blank
dil. sample(jjJL)
dil. calibrator
blank buffer (HO
dil. antiserum <H0
-
25
500
-
sample
sample test
blank
-
25
-
500
25
25
-
-
500
-
-
500
Mix by shaking gently. Let stand for 30+5 minutes at room temperature. Note: Should
small bubbles develop during incubation, they will disappear when the cuvette is shaken
gently.
- 36 -
Measurement
1. Mix each cuvette gently before measuring.
2. Measure the calibrator and the samples according to the instructions for the
instrument.
3. Read the cuvettes in the following order:
Calibrator
blank
Calibrator test 1
Calibrator test 2
Sample 1 blank
Sample ltest
Sample 2 blank
Sample 2 test
Determination of uric acid concentration in serum
Uric acid formed during the catabolism of purine bases cannot be further used in the
"salvage" reactions; it is produced from hypoxantine (in 2 steps) upon the action of xanthine
oxidase. (In a healthy individual, 1 g is formed daily; most of which /cca. 600 mg/ is excreted
in the urine by secretion of kidney tubules /active transport/.) While most mammals further
catabolize uric acid to the highly water-soluble allantoin, in humans lacking uricase, uric acid
is the end product of the degradation. At the normal pH value of the blood plasma, uric acid
occurs primarily in the form of Na urate (solubility: 380 jimol/1 = 6.4 mg%). In the urine,
below pH 5, mostly undissociated uric acid can be found which is poorly water-soluble
(solubility is 20 times less, than that of Na urate).
Elevated uric acid level may occur physiologically, following strenuous physical exercise.
Pathological, primar y hipexuricemia results either from reduced excretion of uric acid in
urine or from enhanced biosynthesis (e. g. in Lesch-Nyhan syndrome). Secondary
hyperuricemia may occur a./ as a consequence of increased cell death in leukemia and in the
case of other malignant tumors (especially following cytostatic or irradiation treatment), in
addition, in hemolytic anemia, in heart attack and in severe pneumonia; b./ as a result of
reduced excretion in kidney failure, in metabolic and respiratoric acidosis.
Prolonged hyperuricemia leads to accumulation of uric acid in the organism, the
consequence of which is the condition of gout. The symptoms are due to the appearance of
- 37 -
Na urate and uric acid crystals in acidic milieu, primarily in the joints of foot and hand
and/or less often, in the kidney.
Normal value
male : 120-400 pmol/1 (2.1-6.7 mg%)
female: 110-380 pmol/1 (2.0-6.4 rng%)
Principle
Uric acid is converted to allantoin and hydrogen peroxide by uricase. Hydrogen peroxide
- in the presence of peroxidase enzyme - oxidizes the colour-forming molecule
(3.5-dichloro-2-hydroxybenzenesulfonic acid /3.5-DCHBS/) to a red- coloured compound,
the absorbance of which is detected at 520 nm.
uricase
uric acid + 02 + 2H202 ----------------- > allantoin + C02 + H202
peroxidase
2H202 + 3.5-DCHBS + 4-aminophenazone ---------------------- > ACSB + HC1 + 4 H20
(coloured)
Materials
reagent solution: (phosphate buffer /pH 7/ 50 mM; 4-aminophenazone 0.3 mM; 3.5DCHBS 4 mM; uricase 200 UA; peroxidase 1000 U/l; stabilizers, activators)
standard solution: 10 mg% =-595 pmol/1 uric acid
.
Hfr
serum sample
- 38 -
Procedure
test tubes
components
1
2
3
sample
standard
blank
reagent(ml)
1
1
1
serum(pl)
76
-
-
standard(pl)
-
20
-
dist. water(pl)
-
-
20
10 min. incubation at 25 °C,
reading absorbance at nm (in 15
min.)
Calculation, evaluation
-y>5"V A sample uric
acid concentration (pmol/I) = 595 x ----------------------A standard
A sample
uric acid concentration (mg%) = 10 x -----------------A standar d
Detcrmination of triglycerides in serum
(by enzymatic-colorimetric method)
Triglycerides are both ingested with the food (exogenous triglycerides) or synthesized in
the body (endogenous triglycerides). They are transported in the blood in the form of
lipoproteins. The mucosal cells in the small intestine convert the exogenous triglycerides into
chylomicrons, which are the lipoproteins that contain the largest amount of triglycrides. The
liver esterifies free fatty acids, coming for the greater part from the adipose tissue, into
endogenous triglycerides. Part of these is released into the blood in the protein-bound form,
this fraction consisting of pre- (3 lipoproteins. Like hypercholesterolemia, a rised serum
triglyceride level is a major risk factor for atherosclerosis and myocardial infarction.
- 39 -
Principle
LPL
triglyceride + 3 H2O ------------- > glycerol + 3 RCOOH
GK
glycerol + ATP ------------- > glycerol-3-phosphate +ADP
GDH
gIycerol-3-phosphate + NAD ------------- > dihydroxyacetone
phosphate + NADH+ H+
diaphorase
indicator + NADH+H+ -------------------- > indicator + NAD
(colorless)
(reddish)
LPL : lipoprotein lipase GK : glycerokinase
GDH : glycerophosphate dehydrogenase
Materials
1. Buffer solution pH 7,9
2. Reagent mixture (LPL, GK, GDH, diaphorase, ATP, indicator, NAD)
3. Standard solution: 2,29 mmol/1
4. Sample (serum)
Working solution preparation: dissolve the reagent mixture in buffer solution. (Solution is
stable for 5 days when stored at +2 - +8 °C for 1 day when stored at +20 - +25 °C)
Procedure
Pipette into the test tubes the following solution:
- 40 -
test tubes
components
I
sample
2
standard
3
blank
working sol.(ml)
1
1
1
10
-
-
standard(pl)
-
10
-
dist. water(pl)
-
-
10
serum(jjl)
20 min. incubation at 25 °C,
reading absorbance at 520 nm
JS vi u_
Calculation
AS
Concentr ations = -------------- x 2.29 (mmol/1)
A
St
S
:
Sample
Standard
Absorbance
A
St:
:
-41 -
Principle of dry chemistry diagnostic tests (measurement by Reflotron system)
After cleaning the measuring chamber and subsequently check the performance of the
optical system:
1. Determination of cholesterol content in plasma
2. Determination of HDL cholesterol content in plasma
3. Determination of triglyceride content in plasma
4. Calculation of LDL cholesterol from the values of cholesterol,triglycerides and HDL
cholesterol on the basis of the Friedewald formula (F3 key)
5. Risk calculation according to -FRAMINGHAM- (F2 key)
In the -FRAMINGHAM- study performed in the USA, the incidence of myocardial
infarction in dependence of defined risk factors was ascertained in 30- to 74-year old women
and men.
Evaluation
The example shows an incidence of 12.5% (incidence of infarction in percent over 6
years). The minimum and maximum incidences (range) of the sex-related age group are
listed for better risk assessment The individual risk is elevated by the factor 5.5 over the
minimum incidence of the sex-related age group.
Test principle
Determination of cholesterol
cholesterol
cholesterol ester ----------------------> cholesterol + RCOOH
esterase
cholesterol
cholesterol + 02 ------------ -----------> cholestenon + H202
oxidase
9
42
POD
indicator (colorless) + H202 ---------------- > indicator (blue) + H20
INCID.
12.5%
RANGE
2 .5% -26%
MULT.
5.5
- 43 -
Determination of triglyceride
esterase
triglyceride + 3 H20 ---------------- > glycerol + 3 RCOOH
GK
glycerol + ATP -------------- > L- a -glycerol phosphate + ADP
GPO
L- a -glycerol phosphate + 02 ----------------- > hydroxyacetone phosphate + H202
POD
indicator (colorless) + H202 ------------------ > indicator (blue) + H20
GK:glycerol kinase GPO:glycerol-3-phosphate oxidase POD:peroxidase
Determination of HDL cholesterol
Precipitation of chylomicrons, VLDL and LDL by means of magnesium ions / dextran
sulfate and subsequent determination of HDL cholesterol.
Reflotron optical system
Measurement of the reflectance, i.e. of the diffusely reflected light intensity, is performed
by the Ulbricht9 sphere. Strictly selected light-emitting diodes (LEDs) with wavelengths
44
centered on 567, 642 and 951 nm serve as light sources. Measurements can thus be taken at
the wavelength that is most appropriate for the individual test. Two symmmetrical-positioned
photodiodes serve as light detectors: a reference photodiode (Dp) and a measuring
photodiode (D).
Diagrammatic illustration of the structure of Ulbricht sphere
Structure of Reflotron reagent carriers
Determination of serum bilirubin
Introduction
-45 -
The partial degradation of hem in human body starts with cytochrome P450 heme
oxygenase in the RES cells. Oxidation of porphyrin ring results in biliverdin. In birds and
reptiles this green coloured substance is the final product of hem degradation. In spite of the
very poor solubility of bilirubin, mammals have been utilizing its advatage being a very
effective antioxidant. Humans secrete bilirubin- diglucuronide into the bile. Further
transformation of bilirubin occurs in the gut by bacteria.
In normal blood serum, bilirubin can be found in a low concentration. According to the
reactivity in the "van den Bergh reaction" "direct" and "indirect" bilirubin levels can be
determined. Direct bilirubin gives a direct colour reaction with diazo reagent, while indirect
bilirubin reacts only in the presence of accelerators, such as caffeine or ethanol. Direct
bilirubin is predominantly bilirubin-diglucuronide, a conjugate produced by the liver.
Indirect bilirubin is the serum albumin bound form. In normal serum, bilirubin is found
almost exclusively in the indirect form. One albumin molecule can bind and transport 2
molecules of bilirubin. The liver cells take up this bilirubin using a high capacity carrier
system. Bilirubin level of newborns is physiologically high in the first two weeks following
birth. In that case the yellow color of blood serum is originated almost exclusively from serum
bilirubin, and directly measurable by spectrophotometer at 455 nm.
In the case of adults, high serum bilirubin level may indicate occlusion of the bile duct
(direct bilirubin), haemolytic processes (indirect bilirubin) or liver damage (both direct and
indirect forms).
Normal values in human serum
total bilirubin : 8.6-17 uM (0.5-1 mg%) direct
bilirubin: 0.8-4.3 uM
(0.05-0.3 mg%)
Principle
In the "van den Bergh reaction" bilirubin reacts with diazo-benzoyl sulfanilic acid
forming an azo-compound (azorubin) which is red at neutral pH. Direct
bilirubin is determined without, while total bilirubin with the addition of caffeine to the
reaction mixture.
- 46 -
Materials
- human serum (is to be kept in dark before the test. Best results are obtained with fresh
serum. Hemolysed serum can not be used.)
- sulfanilic acid solution (29 mM in 0.17 M HC1)
- sodium nitrite solution (25 mM NaN02)
- Na-benzoate + caffeine solution (0.52 M and 0.26 M, respectively)
- K-Na-tartarate solution (0.93 M in 1.9 M NaOH)
- physiological NaCl solution (0.85%)
Procedure
Transfer 0.2 ml aliquots of sulfanyl reagent to four test tubes (2 for samples + 2 for
blank). Add 0.05-0.05 ml NaN02 solution to the two sample tubes.
A. Total bilirubin
Add 1 ml aliquots of caffeine reagent, then 0.2 ml aliquots of serum to a sample and a
blank tube. Stir the contents thoroughly and incubate the tubes for 10 min at room
temperature. Then add 1 ml tartarate solution to both tubes, mix well again, continue
incubation for five more minutes. Measure absorbance of the sample at 580 nm using the
blank as reference.
B. Direct bilirubin
Add 2 ml aliquots of physiological NaCl solution, then 0.2 ml aliquots of serum to the
two remaining (sample and blank) tubes. Stir their content thoroughly and incubate them for
5 min at room temperature. Measure absorbance, using blank as reference, at 540 nm.
test tubes
total bilirubin
sample
components (ml)
blank
- 47 0.2
sulfanilic acid
direct bilirubin
sample
0.2
blank
0.2
0.2
NaN02
0.05
0.05
Na-benzoate + caffeine
1
1
-
-
phys. NaCl
-
-
2
2
serum
0.2
0.2
0.2
-
0.2
10 min.
incubation at 25 °C
tartarate
1
5 min.
reading absorbance
580 nm
-
6
5 min.
1
incubation at 25 °C
7
O
-
-
-
-
540 nm
t
o
m
Calculation
total bilirubin concentration (uM): 185xA58q (mg%): 10.8 x A580
direct bilirubin concentration (uM) : 246 x A540
(mg%): 14.4 x A540 (9 Q( <{ db^kXUX CJ>
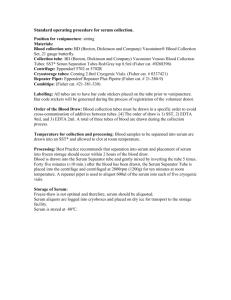
Determination of enzyme activity I.
Fixed-time (Two-point) assay of the a-Amylase enzyme
Hydrated starch and glycogen are attacked by the endosaccharidase a-amylase, which is
present in saliva and pancreatic juice. Amylase has specificity for internal a(l-4)-glucosidic bonds;
a(l-6) bonds are not attacked, nor are a(l-4) bonds of glucose units that serve as branch points. The
pancreatic isoenzyme is secreted in a large excess relative to starch intake and is more important
than the salivary enzyme from a digestive point of view. The products of the digestion by a-amylase
are mainly maltose (glucose-a( l-4)-glucose), maltotriose (glucose-a( l-4)-glucose-a(l- 4)-glucose)
and a-limit dextrins containing on an average eight glucose units with one or more a(
l-6)-glucosidic bonds.
Aim:
Quantitative assay of a-amylase in serum by using Phadebas Amylase Test.
Clinical Use:
Acute pancreatis is often characterized by high serum and urinary a-amylase levels.
Elevated levels may also occur in mumps, hepatic disorders, pancreatic pseudocyst, impaired
renal function (serum only), penetrating or perforating ulcer, peritonitis, intestinal obstruction,
pancreatic carcinoma, after abdominal operations, and following opiate therapy.
In pancreatic insufficiency decreased levels may be found.
Principle of the procedure
- 48 -
This enzyme test use a fixed time for the reaction and expressed the enzyme activity as the
amount of substrate transformed by a specified volume of serum under the particular conditions of
the test. The substrate is a water-insoluble cross-linked starch polymer carrying a blue dye. It is
hydrolyzed by a-amylase to form water- soluble blue fragments. The absorbance of the blue
solution is a function of the a- amylase activity in the sample.
Caution: Use rubber gloves, please! 1. Pipette into two centrifuge tubes the following solutions:
test tubes
components
1
blank
scrum(fil)
-
dist. water(j.il)
200
dist. water(ml)
4
2
sample
200
-
4
5 min. incubation at 37 °C
2. Pre-incubate the tubes for 5 minutes at 37 °C in water bath.
3. Add one tablet to each tube - use forceps - immediately vortex for 10 seconds and replace in
water bath.
4. Incubate by standing the tubes in a well stirred water bath at 37°C for exactly 15 minutes.
5. Stop the reaction exactly 15 minutes after tablet addition by adding 1.0 ml of 0.5 M sodium
hydroxide into each tube. Vortex immediately.
6. Centrifuge at > 1500 g for 5 minutes . Pipette the blue supernatant into a cuvette.
7. Measure the absorbance of the supernatant at 620 nm against distilled water using a cuvette
with 1 cm light path.
Calculation
Subtract the absorbance value of the blank from that of the sample and read the
a-amylase activity in U/l from the standard curve. This gives directly the ct-amylase
activity in serum samples.
Normal valuesi
Reference values in serum: 70-300 U/l.
(Linearity of the method: 35-1000
U/l.)
- 49 -
0.4 0.5 0.S o v a n 0.91 2
150(jh«Ul
3 4 5 S 7 H 9 10
20
Phadebas® Amylase Test
- 50 -
Absorbance 620 nm
3 4 5 8 7 » » 100
Detcrmination of enzyme activity II.
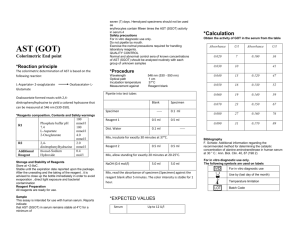
Kinetic assay (Multipoint, Continuous Monitoring) of Aspartate
Aminotransferase (ASAT, GOT) and Alanine Aminotransferase
(ALAT, GPT) enzymes
Aspartate Aminotransferase (ASAT) is found in practically every tissue of the body, including
red blood cells. It is in particularly high concentration in cardiac muscle and liver, intermediate in
skeletal muscle and kidney, and in much lower concentrations in the other tissues.
The measurement of the serum ASAT level is helpful for the diagnosis and following of cases
of myocardial infarction, hepatocellular- disease, and skeletal muscle disorders.
The concentration of Alanine Aminotransferase (ALAT) in tissues is not nearly as great as for
ASAT. It is present in moderately high concentration in liver, but is low in cardiac and skeletal
muscles and other tissues. Its use for clinical purposes is primarily for the diagnosis liver disease.
Aim:
Quantitative assay of ASAT (GOT) [Aspartate Aminotransferase] or ALAT (GPT) [Alanine
Aminotransferase] in serum by using LJV kinetic method.
Principle of the procedure
Kinetic Assay: the rate of the enzyme reaction as a function of time is measured by incubating
serum under specific reaction conditions and measuring the rate of change in substrate , cofactor,
or product concentration. The assay of ASAT/ALAT is based on the following series of reactions:
ASAT
L-Aspartate + a-ketoglutarate —* -----------> Oxaloacetate + L-Glutamate
MDH
Oxaloacetate + NADH + H+ --------------- > L-Malate + NAD+
or
ALAT
L-Alanine + a-ketoglutarate --------------- > Pyruvate + L-Glutamate
- 51 - LDH
Pyruvate + NADH + H+ --------------- > Lactate + NAD+
- 52 -
NDH: malate dehydrogenase
LDH: lactate dehydrogenase
The enzyme, aspartate aminotransferase (ASAT), reversibly transfers an amino group from
aspartate to a-ketoglutarate and forms oxaloacetate in the process. This reaction is coupled with
that of malate dehydrogenase, in which the oxaloacetate is reduced to malate as NADH is
simultaneously oxidized to NAD+.
The enzyme that transfers an amino group from the amino acid alanine to a- ketoglutarate is
alanine aminotransferase (ALAT).
The resulting decrease in absorbance is followed spectrophotometrically and is directly
proportional to the activity of ASAT (or ALAT) in serum.
Reagent composition: Tris buffer, L-aspartate or L-alanine, a-ketoglutarate, MDH, LDH,
NADH, stabilizers, non-reactive vehicle substances.
Test procedure^
Caution: Use rubber gloves, please!
Parameters of the method:
Wavelength: 340 nm Light path:
1 cm Temperature: 25°C
Procedure
1. Pipette 1000 pi reagent solution and 100 pi serum into a cuvette.
2. Mix, wait for 1 minute and measure the absorbance.
3. Measure it again exactly 1, 2 and 3 minutes later and determine 5A/min.
Calculation
8A/min x 1745 = U/l ASAT (or ALAT) activity
Normal values: ALAT:
male:
up to 22 U/l at 25 °C
female:
-52up to 17 U/l at 25°C
male:
up to 18 U/l at 25°C
ASAT:
- 54 -
female:
up to 15 U/l at 25°C
- 55 -
Determination of serum calcium, potassium, and chloride ion
concentration
It is apparent that the concentration of inorganic ions (Na+, K+, Ca++, Mg++, CI", PO^"
etc.) is regulated within very narrow limits in order maintain physiological osmotic pressure,
resting membrane potential, and the excitability of the cells. In the clinical laboratory
inorganic ions are usually determined by using either flame photometry, colorimetry,
refractometry, ion selective electrodes, or atomic absorption spectrophotometry. The subject
of the practical is the determination of K+, Ca++, and CI" by using refractometry, and
colorimetry.
Hypokalemia (decreased K+ concentration in the plasma) develops mostly as a
consequence of diuretic and insulin treatment, excess salt loss due to sweating or diarrhoea,
Cushing-syndrome, Conn syndrome, and metabolic alkalosis. The most frequently occurring
symptoms of hypokalemia are muscle weakness, cardiac arrhythmias, cardiac arrest,
hypotension. Decreased mineralocorticoid activity due to Addison's disease or
spironolactone treatment, metabolic acidosis, chronic renal failure etc. lead to an increase in
extracellular K+ concentration i.e. hyperkalemia. The most characteristic symptoms of
hyperkalemia are cardiac arrhythmias, smooth muscle spasm.
Pathological changes in the plasma chloridc concentration usually occur with parallel
changes in Na+ content in severe salt or water loss/loading.
The calcium in the plasma is present in three different foxms. Approximately 41% of the
total calcium is combined with the plasma proteins, and in this form is undiffusible through
the capillary membranes. About 9% of the calcium is diffusible, however, it is combined with
phosphate, citrate, oxalate etc. in such a manner that it is not ionized. The remaining 50% of
the calcium is both diffusible through the capillary membranes and ionized, therefore this
fraction is considered as active calcium. Hypocalcemia occurs in alkalosis, deteriorated
vitamin-D metabolism, insufficient parathyroid hormone activity, excess oxalate intake, and
steatoxThoea. Hypocalcemia results in tetanic muscle contractions, insufficient cardiac
functions, hypotension, and obstipation. A 50% decrease in plasma Ca++ level is life
threatening. Hypercalcemia may develop as a result of D-hypervitaminosis, increased level
of parathyroid and growth hormones, decreased activity of calcitonin. The symptoms of
hypercalcemia are characterized by mental depression, decxeased reflex activity, cardiac
arrhythmias. A two fold increase in plasma Ca++ content may lead to precipitation of calcium
phosphate throughout the body.
Determination of K+ by refractometry ("Reflotron" system) Test
principle
Potassium ion binds to the K+ selective ionophore valinomycin, than the complex binds
to the anion of an acid-base indicator. The anion of the dissociated indicator is a colourful
compound.
K+ + valinomycin + ind-H = [valinomycin-K]+ [indj" + H+
Normal values:
plasma:3.5-4.6 mmol/1
serum:3.6-5.0 mmol/1
- 56 The plasma or the serum should be separated from the cells within one hour to avoid the
release of intracellular K+
Determination of Ca++ by colorimetry
Test principle
The calcium ion forms a deep purple complex with o-cresolphthaleine in alkaline pH.
Magnesium ions (up to 4 mmol/1) which may interfere with the reaction are bond with
8-hydroxy-quinoline. The linearity of the assay extends up to 3.25 mmol/1 Ca++
Reagents
1. reagent: 360 mmol/1 diethylamine
2. reagent: 0.15 mmol/1 phthalein purple, 17.2 mmol/1 8-hydroxy-quinoline
Standard: 2.5 mmol/1 Ca++
- 57 -
Procedure
Ten pi of distilled water, standard, or sample is added to 1 ml of reagent mixture (1:1),
respectively. Absorbance is measured in 1 cm narrow cuvette using 570 nm
S
lighL
reagent control
standard
sample
1ml reagent lOpl
1 ml reagent lOpl
1 ml reagent lOpl
dist water
standard
sample
[Ca++sample] - (Asampie/Astanciarcj) x [Ca++Stancjar{j] Normal value: serum, plasma: 2.2-2.55
mmol/1
Determination of CI" by colorimetry
Test principle
Chloride releases rhodanide from mercury-rhodanide, and forms mercury- chloride.
Rhodanide forms a red complex with Fe^+.
2 CI" + Hg(SCN)2 ----------- > HgCl2 + 2 SCN"
Fe3+ + 3 SCN" ----------- > Fe(SCN)3
Normal value: 95-105 mmol/I
Procedure
blank
standard
sample
2ml reagent 20pl
2ml reagent 20pl
2ml reagent 20pl
dist. water
standard
sample
Ten minutes of incubation period (20-25 °C) is needed for the complete reaction.
Subsequently, absorbance is measured using 1 cm cuvette and 457 nm light.
[cr
sampleJ ~ (^sample^standard) x l^l standard J
(standard: 100 mM CI")
- 58 -
Enzymatic determination of blood glucose level
Carbohydrates are primarily functioning in metabolism as a fuel to be oxidized and
provide energy for other metabolic processes. In this role, carbohydrates are utilized by cells
mainly in form of glucose. Maintenance of constant glucose level in blood is controlled by
neurohormonal action.
A number of methods using colored product with glucose have been described
(iodometrical method, with o-toluidine). Enzymatic determination is the most specific
method in clinical use nowadays because other reducing hexoses can not alter the results.
Principles
Glucose
oxidase
catalyses
the
oxidation
of
nonphosphorylated
glucose
to
glucono-l,5-lactone with the formation of H2O2. In the presence of peroxidase H2O2 is
converted to oxygen free radicals and these produce a color compound (4-pBenzoquinone-monoimino-phenazone) with phenol and 4-amino antipyrine.
glucose-oxidase
glucose + O2 + H2O --------------------------- > glucono-l,5-lactone + H2O2
peroxidase
2H2O2 + phenol + 4-amino antipyrine --------------------> color compound + 4H2O
Normal values:
Serum:
3.9-5.8 mmol/1 (70-105 mg/dl; 0.7-1.05 g/1)
Liquor:
2.8-3.9 mmol/1 (50-70mg/l)
Materials
Trinder reagent (diluted 1+2 in distilled water)
Standard solution
Sample (serum or liquor)
Distilled water
- 59 -
Procedure
Components(ml)
test tubes
1
2
3
Blank
Sample
Standard
2
2
2
20
-
-
Standard
-
-
20
Sample
-
20
-
Trinder reagent
Dist. water
Mix and incubate for 15 min. at 37aC.
Measure the absorbance at 520 nm against blank. Reaction dye is stable for 1 h.
Calculation
^sample
concentration sample (mmol/1) = -------------------- x concentration standard
^standard
Assay of glycosylated haemoglobin by DCA 2000™ HbA|c system
The term "glycosylated haemoglobin" refers collectively to a series of stable compounds
that are formed between haemoglobin and sugars. Their concentrations are increased within
erythrocytes of patients with diabetes mellitus. The aim of therapy by clinicians is to maintain
their patients' glucose levels at constant normal or near normal levels in blood. Measurement
of serum or plasma glucose levels by laboratory or home monitoring techniques, gives the
measure of glucose regulation over very short time period. It has been found, however, that a
measure of long term blood glucose control can be achieved by measuring the glycosylated
haemoglobin fractions of erythrocytes.
Principle
The DCA 2000™ System relies on an immunochemical technique for the measurement
of HbA|c. A monoclonal antibody has been developed which reacts specifically with certain
amino acid sequences following the N-terminal valine on b- chain of HbAic. The antibody
- 60 -
doesn't binds the haemoglobin glycated at other positions, because both glucose and specific
acid sequences must be present for binding. An agglutinator present as one of reagents
causes agglutination of specific anti-HbA|c coated latex particles. This is measured as an
increase in turbidity by the spectrophotometer. HbAjc present in the patient's sample causes
an inhibition of the agglutination in proportion to its concentration in the blood.
The simplified reaction is described as follows:
- 61 -
Assay Principle Inhibition
Of Latex Agglutination
(Antibody-Latex)
— H i g h Scattering
(Increased Absortiance)
<>
•era
(Agglutinator) £r
Agglutination
«
A
I
»
Hemoglobin A1c
< ► in Patient's Blood
— L o w Scattering
k,C>T (Decreased Absortance)
O Inhibition
Agglutination Inhibited
DCA 2000™ HbA1c
Reagent Cartridge
Pull-Tab
(Pull to release
buffer from tray)
Capillary
Holder
Absorbant
(Picks up
all liquid at
test end)
1 fiL Blood
Sample
Cartridge
Removal Tab
Buffer
Solution Tray with
Foil Seal (600 ¿xL)
[P Agglutinator
Antibody Latex
yJJ^
- 62 -
Oxidant
Optical Window
-63The assay sequence is shown as follows.
2. Capillary
holder
1. Sample collected in capillary.
inserted
into
cartridge.
Cartridge
inserted into
4. Cartridge
rotates to
mix
blood
sample and
o
ferricyanid
e.
M.
-
instrument. Pull-tab
pulled and discarded.
Buffer
solution flows to read
area of the cartridge
where
a
"blank"
reading is obtained.
\J.
Optical window
C
Cartridge rotates
to read position
where total
hemoglobin
reading is taken.
5.
7. Cartridge
rotates to
read
position
where
HbAic
reading
is
obtained.
Cartridge
rotates to
mix
antibody
latex
and
agglutina
tor.