Higher Human Biology
advertisement

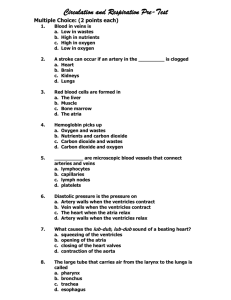
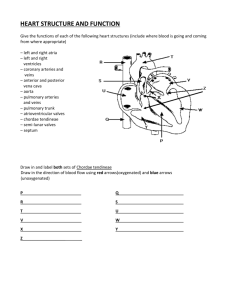
Higher Human Biology Unit 2: The continuation of life Chapter 20: Transport Mechanisms: The cardiac cycle 22/03/2016 Mrs Smith Ch19 The need for transport 1 Learning Intentions Success Criteria To understand the anatomy of the heart, to find out how the heartbeat is controlled and to look at differences in blood pressure in the circulatory system. 1. Describe the cardiac cycle of the heart 22/03/2016 2. Explain the cardiac cycle of the heart in relationship to pressure changes Mrs Smith Ch19 The need for transport 2 Cardiac Cycle The cardiac cycle is the pattern of contraction and relaxation of the heart during one heartbeat. The average heart rate is 75 beats/min with a cardiac cycle of 0.8 secs. Systole = contraction Diastole = relaxation Image source: www.classes.kumc.edu Heartbeat animation The average human heart rate at rest is 75 beats a minute Each heart beat lasts for approximately 0.8 of a second at rest Each heart beat involves a series of Events referred to as THE CARDIAC CYCLE Heartbeat: Atria & Ventricular diastole Stage 1: A heartbeat begins with the heart muscle relaxed and valves closed. Blood flows into the two atria and both sides fill up with blood. This blood has to be pushed through the valves to get into the ventricles. How does this happen? Heartbeat: Atrial systole Stage 2: The atria contract and the blood is squeezed which causes the AV valves leading to the ventricles to open. Blood then flows from the atria into the ventricles. What happens to the open valves when the atria are empty? Heartbeat: Atrial systole Stage 2 (continued): The AV valves between the atria and the ventricles close. This prevents any backflow. What happens next to the blood in the ventricles? Heartbeat: Ventricular Systole Stage 3: Almost immediately, the ventricles contract and the blood is squeezed again. The pressure of the blood forces open the SL valves leading out of the heart. Blood is pumped out of the heart. What happens to the open valves when the ventricles are empty? Heartbeat: Ventricular Systole Stage 3 (continued): When the ventricles are empty, the SL valves leading out of the heart close and the heart muscle relaxes. This completes the sequence of contraction and relaxation in one heartbeat. What will happen next? Stages of a heartbeat Stage 1 (again): The atria fill up with blood as the heartbeat sequence begins again. Why are the walls of the atria thinner than the walls of the ventricles? Why is the wall of the left ventricle thicker than the right ventricle? Try this Scholar Animation Fig.3.9 http://courses.scholar.hw.ac.uk/vle/scholar/session.controller?action=viewContent&contentGUID=dfaf24ad-00219d39-4277-e967e919c79f 2. Heart Valves & Sounds Throughout the cardiac cycle, pressure changes take place in the atria, ventricles and arteries Pressures in the right and left atrium, right and left ventricle, aorta and pulmonary arteries can be recorded and illustrated in graphical form The graph on the next slide shows pressure changes in the left side of the heart and the aorta A similar graph can be drawn for the right side of the heart and the pulmonary arteries Such a graph is similar in shape to that obtained for the left side of the heart but all the pressures readings are of a lower value Pressure Changes in the Heart 120 SL valve closes SL valve opens pressure (mm Hg) 100 aortic pressure 80 left ventricular pressure 60 40 AV valve opens AV valve closes 20 left atrial pressure 0 0 0.1 0.2 0.3 0.4 0.5 0.6 time (s) ATRIA VENTRICLES = systole = diastole 0.7 0.8 Pressure Changes in the Left Side of the Heart During One Cardiac Cycle 120 aortic pressure pressure (mm Hg) 100 The pressure changes in the left ventricle, left atrium and aorta can be related to the phases of the cardiac cycle 80 left ventricular pressure 60 40 20 left atrial pressure 0 0 0.1 0.2 0.3 0.4 time (s) 0.5 0.6 0.7 0.8 Pressure Changes in the Left Side of the Heart A WX A Z Y 120 aortic pressure DUB pressure (mm Hg) Period Z to A represents the phase of Passive Filling of the ventricles when the AV valves are open and 100 the semi-lunar valves are closed Period A to W represents the phase of Atrial Systole 80 when the atria contract and the ventricles are filled to full capacity Period W to X represents 60 the first phase of Ventricular Systole when the ventricles contract in an isometric fashion; the greatest rise in ventricular 40 pressure occurs during this phase and the ventricular volume remains constant Period X to Y represents the20 second phase of Ventricular Systole when ejection of blood takes place and pressure in the aorta rises 0 Period Y to Z represents relaxation 0 of the ventricles (diastole) when the ventricular pressure drops sharply left ventricular pressure left atrial pressure LUB 0.1 0.2 0.3 0.4 time (s) 0.5 0.6 0.7 0.8 Heart Murmur Abnormal cardiac blood flow causes abnormal heart sounds known as heart murmurs. This is often caused by faulty valves that fail to open or close fully. This is often an inherited condition but can be caused by illness e.g. rheumatic fever. Learning Success Criteria Intentions To understand the anatomy of the heart, to find out how the heartbeat is controlled and to look at differences in blood pressure in the circulatory system. 3. Describe the structures involved in the conducting system of the heart 4. Describe the role of the sinoatrio node in the conductivity of the heart 5. State the sequence of electrical conductivity of the heart. 3. Conducting System of the Heart • The heart is special in Pace maker (Sino-atrial that the electrical node (SAN)) stimulation necessary for contraction of its muscles originates from within the heart itself • The sequence of events which occurs during each heartbeat is brought about by the activity of the PACEMAKER and the CONDUCTING SYSTEM of the heart As well as the Pacemaker the conduction system consists of... • Atrio-ventricular node or AV node • Bundle of conducting fibres, which divides into left & right branches (Bundle of His) • Dense network of Conduction fibres in the ventricle walls (Purkinje fibres) • The above cells are specialised muscle cells which join in a network called the CONDUCTION SYSTEM • http://www.bbc.co.uk/learningzone/clips/th e-human-heart/12225.html The PACEMAKER AKA – Sino-atrial Node (SAN) • The pacemaker is located in the wall of the right atrium. • The pacemaker is specialised tissue which exhibits spontaneous excitation. • This means that it initiates electrical impulses which make the heart contract at a certain rate. • This rate can then be regulated by other factors to suit the bodies requirements. • The pacemaker works automatically and would continue to function in the absence of nerve connections from the rest of the body. http://www.youtube.com/watch?v=te_SY3MeWys&fe ature=related Conduction system of the Heart Understanding these DEFINITION will help with the following slides: SYSTOLE; The phase of the heartbeat when the heart muscle contracts and pumps blood from the chambers into the arteries. (the chambers empty). DIASTOLE; The phase of the heartbeat when the heart muscle relaxes and allows the chambers to fill with blood Conduction of the heart: step by step! 1.The electrical signal originates from the pacemaker (sino-atrial node) this makes heart muscle cells contract at a certain rate. 2. A wave of excitation (from the SA node) spreads across the muscle cells of the two atria making them contract (atrial systole). 3.The impulse is picked up by the atrioventricular node (AV node) located near the base of the atria. Conducting System of the Heart 4. The impulse passes from the AV node to the bundle of His. This bundle of conducting fibres divides into right and left branches which are continuous with the Purkinjie fibres in the ventricular walls. 5. Stimulation of these fibres causes contraction of the two ventricles (Ventricular systole). The contraction of the ventricles spreads upwards from the apex. 6. The muscle cells contract in unison, and then relax awaiting the next signal. Summary: Conduction of the heart with an ECG. Such coordination of the heartbeat ensures each type of systole recieves the combined effect of many muscle cells contracting and that the ventricular systole occurs slightly later the atrial systole allowing time for the ventricles to fill completely before they contract. & AGAIN Conducting System of the Heart: Explained a little differently. The origin of the heartbeat is from within a specialised patch of cardiac muscle tissue, located in the wall of the right atrium, and known as the sino-atrial node or SA node SA node in wall of right atrium The AV node connects with a bundle of large fibres called the bundle of His, which divides into left and right bundle branches AV node Another node of specialised tissue known as the AV node is located in the right portion of the septum between the atria and close to the AV valves Bundle of His with left and right bundle branches The left and right bundle branches divide into smaller branches called Purkinje fibres that spread throughout the ventricular muscle CON’T: Conducting System of the Heart: Explained a little differently. When the SA node emits spontaneous electrical impulses, they spread rapidly across both atria due to the inter-connecting nature of the cardiac muscle cells When the electrical impulses reach the border between the atria and ventricles they are blocked by a band of nonconducting fibrous tissue In order to reach the ventricles, electrical impulses must pass through the AV node, which slows down the speed of electrical transmission This delay, called the AV delay, is extremely important as it allows the atria to complete their contraction before the ventricles begin to contract As the impulses spread across the atria, they stimulate a wave of contraction within the atrial walls and atrial systole is triggered Fibrous Tissue AV Node Impulses are conducted from AV node along the bundle of His The bundle fibres divide into numerous Purkinje fibres that permeate throughout the ventricular muscles The spread of electrical impulses throughout the ventricles triggers ventricular systole Electrocardiogram (ECG) The electrical signals of the heart can be detected by electrodes on the skins surface. They are displayed on an oscilloscope screen to produce a pattern called an electrocardiogram (ECG). The diagram below shows a normal ECG The ECG trace for each heartbeat displays 3 distinct waves: A P wave, a QRS complex and a T wave The waves of an ECG R P wave T wave Q S • P wave - Electrical impulses spreading across the atria from the SAN; it coincides with atrial contraction or systole. • QRS complex - Wave of excitation passing through ventricles; coincides with ventricular systole. • T wave - Electrical recovery of the ventricles at the end of ventricular systole. ECG waves : The intervals P–R interval R P wave T wave T–P interval Q S • The P – R interval time between the events of atrial systole and ventricular systole. This period represents the time taken for the impulse to spread from the SA node through the atria, plus the delay in transmission to the AV node, together with the conduction time through the bundle of His and Purkinje fibres. • The T – P interval is the time spent by the heart in diastole before the next atrial systole begins A Abnormal ECGs Heart disease and unusual heart rhythms can be detected by ECG patterns. The Normal ECG diagrams below show identifiable patterns for some common heart conditions. http://www.youtube.com/watch?v=x67vRkooZDc&feature=related Abnormal ECG: Arterial Flutter • In an arterial flutter the contractions occur much too rapidly than normal but do remain coordinated. • The example shown in the diagram shows several P waves for ever QRS complex. Abnormal ECG: Fibrillation • In a fibrillation, contractions of different groups of muscle cells occurs at different times making it impossible for coordinated pumping of the heart chambers to take place. • Ventricular fibrillation, for example produces an ECG with an irregular pattern. • This condition is lethal if not corrected. Abnormal ECG: tachycardia. • During ventricular tachycardia, abnormal cells in the ventricle walls act like pacemakers and make these chambers beat rapidly and independently of the atria. • The P (atrial) waves are absent and the wide QRS waves are abnormal. Pacemakers Abnormal heart rhythms can be controlled by fitting an artificial pacemaker. This stimulator regulates the heart beat by sending out small electrical impulses to the heart making it beat normally. Task: Torrance-TYK pg152 Qu’s 1&4 22/03/2016 Mrs Smith Ch18 Birth & Post-natal development 41 Essay Questions: SQA 2010 Discuss the conducting system of the heart and how it is controlled. (10) 22/03/2016 Mrs Smith Ch19 The need for transport 42 Learning Intentions Success Criteria To understand the anatomy of the heart, to find out how the heartbeat is controlled and to look at differences in blood pressure in the circulatory system. 6. Describe the changes in blood pressure as blood flows through the circulatory system. 7. Explain these changes in blood pressure in reference to peripheral resistance. 8. Explain the role of elastic walls of the main arteries. 22/03/2016 Mrs Smith Ch19 The need for transport 43 4. Blood Pressure Contraction of the ventricles creates pressure which causes the blood to flow. The pressure in the arteries rises and falls as the heart goes through systole & diastole. Ventricular systole = maximum ~120 mm Hg Ventricular diastole = minimum ~80 mm Hg Blood Pressure Con’t • During ventricular systole (contraction) the pressure of the blood in the aorta rises to a maximum e.g. 120 mmHg • During ventricular diastole (relaxing) it drops to a minimum e.g. 80 mm Hg Measurement of the blood pressure Try the Scholar Animation 3.4.7 Measuring Blood Pressure http://courses.s cholar.hw.ac.uk/v le/scholar/sessi on.controller?act ion=viewContent &contentGUID= 06fbef35-81055747-fc8955365ca328af Systolic and diastolic blood pressures are measured using a sphygmomanometer and varies widely from person to person. The graph below shows arterial blood pressure trace The graph below shows arterial blood pressure trace 5. Role of Elastic walls Large arteries are elastic They conduct blood from the heart to medium sized arteries When the heart contracts and ejects blood, the walls stretch to accommodate the surge of blood. The stretched fibres store some of the energy. During the diastole phase the arteries recoil, causing the blood to move forward in a continuous flow. Diagram of the Elastic walls 6. Decreasing Blood Pressure • Although the pumping action of the heart causes fluctuations in aortic blood pressure (e.g. Systolic 120mm Hg and diastolic 80mm Hg), the average pressure in the aorta remains fairly constant at 100mm Hg. • The diagram shows how a progressive decrease in pressure occurs as blood travels round the circulatory system dropping to almost zero by the time it reaches the right atrium again Why does the Blood Pressure decrease? • The pressure of the blood decreases as the blood moves away from the heart. • Changes are due to the peripheral resistance as the vessels become narrower. • Blood pressure is also related to the volume of blood present. • e.g increase in volume increase in blood pressure Peripheral Resistance • Peripheral resistance means the resistance to the blood flow caused by friction between the blood and the walls of the vessels. • This friction occurs because blood is sticky and the arterioles and capillaries through which it passes are narrower in diameter and present a large surface area of wall in contact with blood. Peripheral resistance: Greatest in the arterioles The arterioles present the greatest resistance to blood flow and bring about the largest drop in pressure (around 50mm Hg). LARGE DROP IN THE ARTERIOLES Changes in blood pressure, velocity, and the area of the arteries, capillaries, and veins of the circulatory system Changes in blood pressure • Blood pressure is also directly related to volume of blood present in the arteries. An increased arterial volume leads to an increase in arterial pressure. High Blood Pressure Caused by: • Any factor that increases the rate and force of contraction of the heart tend to increase the arterial blood pressure For example •High levels of stress •Excessive salt in the diet. Dangers of High Blood Pressure Prolonged high blood pressure is dangerous because it • Requires the ventricles to work harder (in order to eject the blood into the arteries). • Makes arterial walls more prone to atherosclerosis. • May damage blood vessels (e.g. In cerebrum leading to a ‘stroke’). Image source: www.healthygoodies.ca Task: Torrance-TYK pg156 Qu’s 1&2 22/03/2016 Mrs Smith Ch18 Birth & Post-natal development 59 Learning Intentions To understand how the various vessels involved in the transport are related and how materials are exchanged between these vessels, tissue fluid and body cells. Success Criteria 9. Describe the structure and function of the vessels in the lymphatic system 10. Describe the method of movement of lymph through the lymphatic circulation 11. Describe the absorption of lipid in relation to the lymphatic circulation 12. Describe the structure and function of lymph nodes 9. Lymphatic System Image source: http://trc.ucdavis.edu 9. Lymphatic Vessels The lymphatic system is considered a specialised part of the circulatory system because lymph fluid is derived from blood and lymph vessels return lymph to the bloodstream. Tiny lymphatic vessels have porous walls that lets them absorb excess tissue fluid (lymph) filtered from the bloodstream at the capillary beds. This is collected by lymph capillaries which join to form larger lymphatic vessels. 10. Lymphatic Circulation • Flow of lymph is dependent upon the vessels becoming periodically compressed when muscles contract during breathing and movement • Backflow of lymph is prevented by valves • Lymph fluid is returned to the bloodstream by 2 lymphatic ducts in the veins of the arms 11. Absorption of lipids Each finger-like villus in the small intestine has a tiny lymphatic vessel called a lacteal. The epithelial cells on the surface of the villus absorb the products of fat digestion (lipids). Droplets of lipid then pass to the lacteal and to the lymphatic system where they become part of the lymph. 12. Lymph Nodes Lymph nodes are oval or bean-shaped structures found in the lymphatic system, particularly where lymph vessels meet. They are usually found in groups (glands) at the neck, armpit and groin. The Lymphatic System Task label the diagram from page 155 - Torrence Answer: Are your labels correct? Summary: Function of Lymph Nodes • Engulf microbes by phagocytosis. • Filter unwanted debris and toxins from lymph. • Produce lymphocytes which make antibodies Swollen Lymph Nodes During illness, if many micro-organisms enter the nodes they swell up and can even become infected. Oedema This occurs when tissue fluid gathers in the spaces between cells and blood capillaries causing tissues to swell. This can be caused by • Malnutrition Low levels of plasma proteins result in the tissue fluid and blood water concentration being equal, therefore, no net movement of water • High Blood Pressure Tissue fluid produced at a faster rate than it can be drained away. e.g. kwashiorkor Oedema Oedema can also be caused by parasites e.g. larvae of the filarial worm, transmitted by mosquitoes, which invade the lymphatic system then when they mature, blocking lymph vessels. This causes excessive growth of tissue – a condition called elephantiasis. http://www.youtube.com/watch?v=pwfdTndbNfA&feature=related Task: Torrance-TYK pg156 Qu 3 22/03/2016 Mrs Smith Ch18 Birth & Post-natal development 73 Testing Your Knowledge…. • Pg 156 Q 3 • 3a i) Describe the means by which lymph in a lymph vessel is forced along through the lymphatic system • ii) what structures prevent backflow of lymph? • iii) which structures along lymph to return to the blood circulatory system? • 3b) which type of food is absorbed into the body via the lymphatic system? • 3c i) which type of white blood cell is produced in the germinal centre of the lymph nodes? • ii) Which type of white blood cell removes micro-organisms from lymph as it passes through the spaces in a lymph node?