Psychological Disorders and Treatments
advertisement

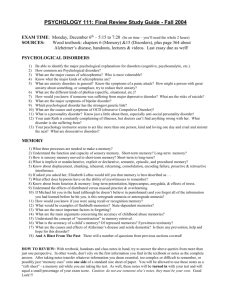
PSYCHOLOGICAL DISORDERS AND TREATMENTS 8-10% and 7-9% (A combined 15-19% of the exam) QUESTIONS TO CONSIDER How should we define psychological disorders? How should we understand disorders? Do underlying biological factors contribute to disorders? How do troubling environments influence our wellbeing? How do nature and nurture interact? How should we classify psychological disorders? And can we do so in a way that allows us to help people without stigmatizing them with labels? DEFINING PSYCHOLOGICAL DISORDERS According to the American Psychiatric Association…. Psychological Disorder- a syndrome marked by a clinically significant disturbance in an individual’s cognition, emotion regulation, or behavior Disturbed behaviors are maladaptive— they interfere with everyday life RISK FACTORS- NATURE OR NURTURE THE DIATHESIS STRESS MODEL NO STRESS NO GENETIC PREDISPOSITION GENETIC PREDISPOSITION STRESS PREVALENCE OF PSYCHOLOGICAL DISORDERS 26% of American Adults Immigrants experience better mental health than their native US counterparts 75% Experience Symptoms before Age 24 Poverty plays a large role in psychological disorders, why? THE MEDICAL MODEL Psychological disorders are diseases that have physical causes that can be diagnoses, treated, and in most cases, cured, often through hospitalization Does not account for environmental factors THE BIOPHYCHOSOCIAL APPROACH Includes the influences of both nature and nurture Bio- psycho- social Biological Influences Evolution Genetics Brain structure and chemistry Psychological Disorder Psychological Influences Stress Trauma Learned helplessness Mood-related perception and memory Social-Cultural Influences Roles Expectations Definitions of normality and disorder CLASSIFYING PSYCHOLOGICAL DISORDERS American Psychiatric Association’s Diagnostic and Statistical Manual for Mental Disorders (5th Edition) DSM-V Guides medical diagnoses and defines who is eligible for treatments, including medication CLEARING UP SOME TERMINOLOGY Psychologist vs. Psychiatrist People with psychological disorders vs. insanity PERSON FIRST LANGUAGE PSYCHOLOGICAL DISORDERS PROJECT THE PROS AND CONS OF DIAGNOSTIC LABELS The Rosenhan Study Pros Cons PSYCHOLOGICAL DISORDERS AND TREATMENTS Organization: Name and classification (when applicable) of the disorder (How is it classified in the DSM-V?) Diagnostic criteria (How is it diagnosed? What are the common symptoms? Understanding the disorder (how do the different perspectives contribute to the understanding of the disorder and how it is formed?) Anxiety Disorders ANXIETY DISORDERS- CLASSIFICATION Generalized Anxiety Disorder Panic Disorders Specific Phobias Social Anxiety Disorder Agoraphobia ANXIETY DISORDERS- DIAGNOSTIC CRITERIA Distressing, persistent anxiety or maladaptive behaviors that reduce quality of life Duration of 6 months or more GENERALIZED ANXIETY DISORDERDIAGNOSTIC CRITERIA Continually tense, apprehensive, and in a state of autonomic nervous system arousal Worry continuously, jittery, agitated, and sleepdeprived May cause a depressed mood and lead to physical problems such as high blood pressure Debilitating- interferes with normal functioning PANIC DISORDERS- DIAGNOSTIC CRITERIA Marked by unpredictable, minutes-long episodes of intense dread in which a person experiences terror, accompanying chest pain, choking , or other frightening sensations SPECIFIC PHOBIA- DIAGNOSTIC CRITERIA Irrational fears cause the person to avoid some object Individual become incapacitated by their efforts to avoid the fearful situation SOCIAL ANXIETY DISORDER- DIAGNOSTIC CRITERIA Intense fear of being scrutinized by others, avoiding potentially embarrassing social situations, such as speaking up, eating out, or going to parties Fear of performance situations is a specialized subset AGORAPHOBIA- DIAGNOSTIC CRITERIA Fear or avoidance of situations, such as crowds or wide open places, where one has felt loss of control or panic OBSESSIVE COMPULSIVE DISORDERDIAGNOSTIC CRITERIA Characterized by unwanted repetitive thoughts (obsessions) and or actions (compulsions) Persistently interfere with everyday living and causes distress Onset occurs in the late teens or 20s; effects 2-3 percent of the population OCD IN MRS. LALLEMAND’S FAVORITE MOVIE CRASH COURSE- ANXIETY AND OCD POSTTRAUMATIC STRESS DISORDERDIAGNOSTIC CRITERIA Classified under Trauma and Stress Related Disorders 4 Diagnostic Criteria Re-experience (through dreams or thoughts) Avoidance (of situations or people) Persistent Negative Alterations in Cognition and Mood (numbing of mood, persistent negative emotional state) Alteration in Arousal and Reactivity (includes irritability, aggressive behavior, reckless or selfdestructive behavior) ANALYSIS OF ANXIETY DISORDERS, OCD, AND PTSD HOW DO THEY FORM? From the behavioral perspective Classical conditioning Operant conditioning Observational learning Biological perspective Natural selection Genes The brain Mood Disorders (Not a DSM-V Term) MOOD DISORDERS-CLASSIFICATION Major Depressive Disorder Bipolar Disorder MAJOR DEPRESSIVE DISORDERDIAGNOSIS The presence of at least five of the following symptoms over a two week period of time Depressed mood most of the day Markedly diminished interest or pleasure in activity most of the day Significant weight loss or gain when not dieting, or significant decrease or increase in appetite Insomnia or sleeping too much MAJOR DEPRESSIVE DISORDERDIAGNOSIS The presence of at least five of the following symptoms over a two week period of time Physical agitation or lethargy Fatigue or loss of energy Feeling worthless, or excessive or inappropriate guilt Problems in thinking, concentrating, or making decisions Recurrent thoughts of death or suicide BIPOLAR DISORDER- DIAGNOSTIC CRITERIA Mania- a mood disorder marked by hyperactive, widely optimistic state Individuals with bipolar disorder alternate between depression and mania (from week to week, not day to day) UNDERSTANDING MOOD DISORDERS Some facts about depression…. Many behavioral and cognitive changes accompany depression Depression is widespread Women’s risk of major depression is double that of men’s Most major depressive episodes self-terminate UNDERSTANDING MOOD DISORDERS Some facts about depression… Stressful events related to work, marriage, or relationships often precede depression With each new generation, depression is striking earlier, affection more people, with the highest rates in developed countries Depression has 37% heritability, bipolar disorder 80% UNDERSTANDING MOOD DISORDERS THE BIOLOGICAL PERSPECTIVE Mood disorders run in families Heritability of depression is 37% Heritability of bipolar disorder is 80% THE BIOLOGICAL PERSPECTIVE The Depressed Brain Lower levels of serotonin and dopamine PET SCAN OF DEPRESSED VS. BIPOLAR BRAIN Review: How does a PET scan work? What can it show us? PET scans show that energy consumption in the brain goes up during manic episodes of bipolar disorder THE SOCIAL-COGNITIVE PERSPECTIVE Learned helplessness- when faced with adverse events, an individual (animal or human) may begin to believe that they have no control over situations and begin to feel hopeless Rumination- staying focused on a problem Adaptive when trying to solve an external problem or overcome a challenge Problematic when self-focused THE SOCIAL-COGNITIVE PERSPECTIVE Depression prone people tend to respond to bad events in an especially self-focused, self-blaming way Think about it from a mindset perspective… CRASH COURSE- DEPRESSION AND BIPOLAR DISORDER SCHIZOPHRENIA-CLASSIFICATION Means “split mind” NOT THE SAME AS MULTIPLE PERSONALITY DISORDER OR SPLIT BRAIN RESEARCH!! Split, as in split from reality Classified under Schizophrenia Spectrum and Other Psychotic Disorders Psychosis- a psychological disorder in which a person loses contact with reality, experiencing irrational ideas and distorted perceptions SCHIZOPHRENIA- DIAGNOSIS AND SYMPTOMS Individual exhibits two of the following symptoms Delusions Hallucinations Disorganized speech and behavior Other symptoms that cause social and occupational dysfunction (often diminished or inappropriate emotion) Symptoms present for 6 months with at least 1 month of active symptoms DELUSIONS VS. HALLUCINATIONS Delusions- false thoughts Often about grandeur or persecution Can manifest as paranoia- fear based delusions Hallucinations- false sensory experiences Seeing, hearing, smelling, or tasting something that is not actually there Auditory hallucinations are common, hearing voices, often persecuting or ordering ANDERSON COOPER SCHIZOPHRENIA SIMULATION INAPPROPRIATE EMOTIONS AND DISORGANIZED BEHAVIORS Emotions Expressed emotions are utterly inappropriate Anger for no reason, laughing when others are crying May exhibit flat affect- expressing no emotions at all Most have difficulty perceiving facial emotions and exhibiting empathy Behaviors Senseless, compulsive acts such as continually rocking or rubbing arms Catatonic (motionless for hours), followed by becoming agitated ONSET AND DEVELOPMENT Strikes as young people are maturing into adulthood Affects 1 in 100 people All cultures are susceptible Effects both men and women, thought men seem to get it earlier and it strikes more severely ONSET AND DEVELOPMENT Can appear suddenly in reaction to stress (easier to treat) Can develop gradually- typically individuals with a history of social inadequacy and poor school performance (harder to treat) Positive Symptoms- hallucinations, disorganized talking, inappropriate emotions Negative Symptoms- toneless voice, expressionless faces, mute rigid bodies UNDERSTANDING SCHIZOPHRENIABIOLOGICAL PERSPECTIVE NEUROTRANSMITTERS Dopamine over activity Brains of deceased schizophrenics show a six fold increase in dopamine receptors Intensified hallucinations and paranoia ABNORMAL BRAIN ANATOMY AND ACTIVITY Review…what are the functions of the following brain structures? Thalamus- AmygdalaCorpus callosumCerebrum/ cortex/ cerebral cortexFrontal Lobe (a portion of the cortex)- ABNORMAL BRAIN ANATOMY AND ACTIVITY Review…what are the functions of the following brain structures? Thalamus- filters incoming sensory information and relays it to the proper area of the cortex for processing and storage Amygdala- fear processing center Corpus callosum- connection between the two hemispheres of the brain Cerebrum/ cortex/ cerebral cortex- where sensory information is processed, memories are stored, and higher order thinking occurs Frontal Lobe (a portion of the cortex)- reasoning, planning, and problem solving ABNORMAL BRAIN ANATOMY AND ACTIVITY Considering the function of each part of the brain and the symptoms of schizophrenia, try to predict how the brains of schizophrenic patients may differ from a nonschizophrenic individual. ABNORMAL BRAIN ANATOMY AND ACTIVITY Thalamus- PET scans show increased activity during hallucinations Amygdala- PET scans show increased activity during paranoid episodes Increased fluid and smaller brain regions (cortex, thalamus, and corpus callosum) slows neural firing and interrupts coordination of neural signaling Frontal Lobe (a portion of the cortex)- a noticeable decline in the brain waves GENETIC FACTORS Twin studies show an increased risk 60-70% of identical twins both being diagnosed with schizophrenia vs. 10-30% for fraternal twins NATURE VIA NURTURE Low birth weights, maternal diabetes, older paternal age, and oxygen deprivation during delivery Brain fully develops during midpregancy (2nd trimester) Viral infections during pregnancy Increased risk if the country experiences a flue epidemic Increased risk if you are born in more densely populated area Increased risk if you were born in the spring or summer Increased risk if your mother was sick while pregnant NURTURE- RISK FACTORS A mother whose schizophrenia was severe or long-lasting Birth complication, often involving oxygen deprivation and low birth weight Short attention span and poor muscle coordination Disruptive or withdrawn behavior Emotional unpredictability Poor peer relations and solo play OTHER DISORDERS Other Disorders Somatic Symptom and Related Disorders Dissociative Disorders Somatic Symptom Disorder Illness Anxiety Disorder Dissociative Identity Disorder Anorexia nervosa Eating Disorders Bulimia nervosa Binge Eating Disorder Personality Disorders Antisocial Personality Disorder SOMATIC SYMPTOM DISORDER Psychological disorder in which the symptoms take a somatic (bodily) form without apparent physical cause Vomiting, dizziness, blurred vision, difficulty in swallowing, prolonged pain Can be strongly influenced by culture Diagnostic Criteria: Persistently symptomatic (at least 6 months) Significantly distressing or disruptive to daily life and must be accompanied by excessive thoughts, feelings, or behaviors ILLNESS ANXIETY DISORDER Formerly known as hypochondria Disorder in which the individual interprets normal physical sensations as symptoms of a serious disease Diagnostic Criteria: heightened bodily sensations, are intensely anxious about the possibility of an undiagnosed illness, or devote excessive time and energy to health concerns, often obsessively researching them DISSOCIATIVE IDENTITY DISORDER A rare disorder in which a person has two or more distinct and alternating personalities Diagnostic Criteria Two or more distinct personality states must be present, each with their own way of being Recurrent gaps in the recall of everyday events, important personal information, and/or traumatic events that are inconsistent with ordinary forgetting No substance abuse problems DISSOCIATIVE DISORDER CONTROVERSYIS IT A REAL DISORDER? Disorder is localized in time and space We are all capable of presenting a different version of ourselves Hillside strangler case Individuals diagnosed show heightened brain activity in brain areas associated with the control and inhibition of traumatic memories Psychodynamic theory and learning theory support a possible mechanism CRASH COURSE! EATING DISORDERS You have notes about this! Look in the motivation and emotion unit! ANOREXIA NERVOSA- DIAGNOSIS 1. Significantly low body weight for their developmental stage (85% of what is considered normal in previous additions) and restrictive calorie intake. 2. An overtly expressed fear of weight gain AND persistent behavior that interferes with weight gain. 3. Distorted body image. ANOREXIA NERVOSA Associated problems Growth of fine hair on the body White Thinning of bones and hair Female Severe constipation Middle or higher income family Low blood pressure Damage to heart and thyroid Risk indicators Perfectionist Traumatic event BULIMIA NERVOSA- DIAGNOSIS 1. Bing eating and inappropriate purging (via induced vomiting or laxative use) behavior once weekly BULIMIA NERVOSA Associated problems Chronic soar throat Kidney problems Dehydration Gastrointestinal disorders Dental problems Risk indicators Highly perfectionistic Secretive Low self-efficacy Impulsiveness Depression Sexual and physical abuse in childhood CAUSES AND TREATMENTS Causes Susceptibility to social pressure treatments Psychotherapy Genetic influence on psychological Hospitalization characteristics (perfectionism, impulsivity, serotonin regulation) A combination of both Changes in the brain due to the disorder BINGE-EATING DISORDER- DIAGNOSIS 1. Bing eating once weekly over the last 3 months Characteristics Most are overweight Eat quickly, a great deal when not hungry, or until they are uncomfortably full Experience disgust or shame after binging Often eat alone BINGE-EATING DISORDER Associated problems Diabetes Risk indicators Overweight already Hypertension Cardiovascular disease Likely to place emphasis on physical appearance, weight, and body shape Emotional eaters CAUSES AND TREATMENTS Causes Emotional eating/stressful events treatments Psychotherapy Areas of the brain and endocrine system that respond to stress are overactive- more likely to see events as stressful Weight loss Changing relationship with food PERSONALITY DISORDERS A collection of psychological disorders characterized by inflexible and enduring behavior patterns that impair social functioning Divided into three “clusters” with key characteristics PERSONALITY DISORDERS Cluster A- Eccentric or odd behaviors Paranoid Schizoid Schizotypal Cluster B- dramatic or impulsive behaviors Antisocial Borderline (I love you, I hate you, Please don’t leave me) Histrionic (attention seeking) Narcissistic (intense love of self) Cluster C- Fearful sensitivity to rejection Avoidant Dependent Obsessive-compulsive ANTISOCIAL PERSONALITY DISORDERDIAGNOSIS Significant impairments in personality functioning manifest by impairments in self-functioning and interpersonal functioning. Self-Functioning: Identity: Ego-centrism; self-esteem derived from personal gain, power, or pleasure. Self-direction: Goal-setting based on personal gratification; absence of prosocial internal standards associated with failure to conform to lawful or culturally normative ethical behavior. Impairments in interpersonal functioning: Empathy: Lack of concern for feelings, needs, or suffering of others; lack of remorse after hurting or mistreating another. Intimacy: Incapacity for mutually intimate relationships, as exploitation is a primary means of relating to others, including by deceit and coercion; use of dominance or intimidation to control others. ANTISOCIAL PERSONALITY DISORDER The most troubling and heavily research of the personality disorders Sociopath/psychopath Male that shows symptoms before age 15 Criminality is not an essential component, but about 50% participate in criminal behavior Behave impulsively and then feel and fear little UNDERSTANDING ANTISOCIAL PERSONALITY DISORDER Specific genes associated with antisocial personality disorder have been identified Individuals with the disorder show little fear and little autonomic nervous system arousal, low levels of stress hormones If channeled it may lead to adventurousness, heroism, and athleticism The genes that put individuals at risk for antisocial personality disorder also put them at risk for substance abuse problems UNDERSTANDING ANTISOCIAL PERSONALITY DISORDER Decreased brain activity in the frontal lobe and the area of the cortex that helps control impulses Deficits in frontal lobe functions such as planning, organization, and inhibition Respond poorly to the facial displays of those in distress Inability to feel empathy CRASH COURSE! TREATMENTS PSYCHOTHERAPY MYTH PSYCHOTHERAPY REALITY BEHAVIOR THERAPIES Applies learning principles to the elimination of unwanted behaviors View maladaptive behaviors as behaviors that can be replaced by constructive behaviors CLASSICAL CONDITIONING REVIEW CLASSICAL CONDITIONING TECHNIQUES Work on the principle of counterconditioning- using classical conditioning to evoke a new response to stimuli that are triggering unwanted behaviors Two substitute a positive response for a negative response in a harmless situation Exposure therapies Systematic Desensitization The third substitutes a negative response for a positive response in a harmful situation Aversive Conditioning EXPOSURE THERAPIES Expose people to what they normally avoid or escape (behaviors that are reinforced by reduced anxiety) “Face your fears” Allows people to habituate to the fear HABITUATION EXPOSURE THERAPY SYSTEMATIC DESENSITIZATION if you can repeatedly relax when facing anxiety-providing stimuli, you can gradually eliminate your anxiety Must proceed gradually Involves progressive relaxation AVERSIVE CONDITIONING Unwanted behavior is associated with an unpleasant feeling Bitter nail polish for nail biting Bitter apple spray for dogs that chew Alcohol mixed with drugs that cause vomiting Not as effective Individual outside of treatment has free will Once the pairing is terminated there may be extinction OPERANT CONDITIONING Also known as behavioral modification Reinforcement of desired behaviors while withholding reinforcement for undesired behaviors In an institutional setting may take the form of a token economypatients receive tokens for positive behaviors that can be exchanged for prizes of their choosing Will it last? Is it ethical? COGNITIVE THERAPIES Therapy that teaches people new, more adaptive ways of thinking, based on the assumption that thoughts intervene between events and our emotional reactions Rational-Emotive Behavior Therapy (REBT) Arron Beck’s Therapy for Depression Cognitive Behavioral Therapy (CBT) RATIONAL-EMOTIVE BEHAVIOR THERAPY Confrontational therapy that vigorously challenges peoples illogical, self-defeating attitudes and assumptions Albert Ellis ALBERT ELLIS AND GLORIA CARL ROGERS AND GLORIA AARON BECK’S TREATMENT FOR DEPRESSION Cognitive therapist that believes in changing peoples thinking but emphasis a gentler approach A good example of the steps taken during cognitive therapy Aim of Technique Technique Reveal Beliefs Question your interpretations Rank thoughts and emotions Test Beliefs Examine consequences Decatastrophize thinking Change Beliefs Take appropriate responsibility Resist Extremes COGNITIVE-BEHAVIORAL THERAPY (CBT) Popular integrative therapy that combines cognitive therapy with behavior therapy Changes both thinking and behavior Become aware of your negative thinking, replace it with positive thinking, and practice that more positive approach everyday Works for anxiety disorders, mood disorders, and may also be helpful with OCD BIOMEDICAL THERAPIES Psychically changing the brain’s functioning by altering its chemistry with drugs or affecting its circuitry with electroconvulsive shock, magnetic impulses, or psychosurgery DRUG THERAPIES Antagonist compete for the receptor sites of neurotransmitters used when the neurotransmitter is found in excess Agonist Increase the availability of specific neurotransmitters Used when the neurotransmitter is lacking DRUG THERAPIES ANTIPSYCHOTIC DRUGS Drugs used to treat schizophrenia and other severe thought disorders Dopamine antagonist- they block dopamine receptor sites Examples: Chlorpromazine“Chlor-pro-ma-zine” Risperdal and Zyprexa Side Effects; sluggishness, tremors, twitches similar to those of Parkinson’s ANTIANXIETY DRUGS Depress the central nervous system to control anxiety and agitation Examples: Xanax Ativan Side Effects: learned response and dependency DRUG THERAPIES ANTIDEPRESSANTS Also known as SSRIs- selective serotonin reuptake inhibitors Agonists- work by increasing the availability by blocking its reuptake Also successful in treating anxiety disorders, obsessive-compulsive disorder, and PTSD Examples: Fluoxitine (Prozac) Zoloft Paxil NEURON SSRI MECHANISM NATURAL ANTIDEPRESSANTS Aerobic Exercise Cognitive Therapy RECENT RESEARCH Drugs (bottom-up) + Cognitive-behavioral therapy (top-down) MOOD STABILIZING MEDICATION Lithium and Depakote (usually used for epilepsy) are effective in treating the manic episodes associated with bipolar disorder BRAIN STIMULATION Electroconvulsive Therapy (ECT) – used for severely depressed patients by sending a brief electric current through the brain of an anesthetized patient Repetitive Transcranial Magnetic Stimulation (rTMS)- repeated pulses of magnetic energy to the brain of awake patients PSYCHOSURGERY Lobotomy- separating the frontal lobes from the emotion controlling centers of the brain Calmed uncontrollably emotional and violent patients Produced permanently lethargic, immature, and unreactive individuals No longer practiced THERAPEUTIC LIFESTYLE CHANGE Aerobic exercise (30 min per day, 3 times per week) Adequate Sleep (7-8 hours per night) Light Exposure (30 minutes per day)- amplifies arousal and regulates hormone levels) Social Connection (allows for human need to belong) Antirumination (identify and redirect negative thoughts) Healthy Diet (supports healthy brain and body function)