PLAN - PA SPREAD
advertisement

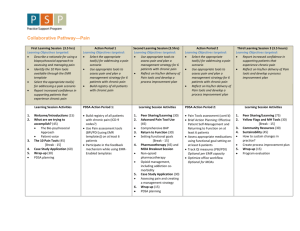
More on PDSAs Connie Sixta, RN, PhD MBA Patricia L. Bricker, MBA Characteristics of the Improvement Model • Action-oriented – “What are you going to test next Tuesday?” • Rapid-cycle testing of changes • Evaluation and revision of all changes before implementation • Testing and implementing the changes in small populations, then spreading to the larger population • Evaluate impact using annotated run charts • Monthly reporting of tests and outcomes Chronic Care Model Health System Community Health Care Organization Resources and Policies SelfManagement Support Informed, Activated Patient Delivery System Design Productive Interactions Decision Support Clinical Information Systems Prepared, Proactive Practice Team Improved Outcomes Model for Improvement What are we trying to accomplish? How will we know that a change is an improvement? What changes can we make that will result in improvement? Act Plan Study Do PDSA versus PPPP Act Plan Study Do Action & Improvement Plan Plan Plan Plan No Action, no improvement Why Test? • Increase the belief that the change will result in improvement • Predict how much improvement can be expected from the change • Learn how to adapt the change to conditions in the local environment • Evaluate costs and side effects of the change • Minimize resistance upon implementation The PDSA Cycle Act • What changes are to be made? • Next cycle? Study • Complete the analysis of the data • Compare data to predictions • Summarize what was learned Plan • Objective • Questions and predictions (why) • Measure of success • Plan for the cycle (who, what, where, when) Do • Carry out the plan • Document problems and unexpected observations • Begin analysis of the data Repeated Use of the Cycle A P S D A P S D Hunches and Theories Changes that result in improvement Testing on a Small Scale • Conduct the test with one provider in the office, or with one patient • Conduct the test over a short time period • Test the change with the members of the team that helped develop the plan • Test the change on a small group of volunteers • Minimize confusion, frustration until bugs are worked out, then spread Plan (P) for Organized Evidence-based Care PDSA 1: Test EMR alert system for patients with DM Objective: Implement DM alert system for staff/providers PLAN: Predictions: EMR alert system will help staff/providers in recognizing patients with DM on schedule, during pre-visit, visit. Who, what, when, where: Develop EMR alert. On Wednesday Jean (MA) will use alert to identify DM patients on schedule next day and measures not met and due. On Thursday Dr. Moore will identify patients with DM when EMR page opened. How will you measure success of the test: The success of the test will be identification by MA of 100% of the patients with DM on the schedule and 100% identification by MD when opening the EMR page. Ease in recognition and accuracy. The DSA Part of the PDSA DO: Test completed as planned and provider/staff provided feedback. DM patients on the schedule/seen Thursday counted. Provider and staff kept track of # DM patients identified with alert. STUDY: For 90% of DM patients, the alert activated. One patient with DM without an alert had problem list error. Both MA and MD felt the alert was very helpful in giving planned care at every visit and proactively addressing needs. ACT: Retest with another MA and MD on Monday. Plan (P) for Organized Evidence-based Care PDSA 2: Test clinical guidelines/reminders for DM patients Objective: Implement DM guidelines/reminders PLAN: Predictions: EMR clinical guidelines/reminders that default whenever DM patients seen will support planned care at every visit. Who, what, when, where: Develop clinical guideline/reminder EMR template. On Wednesday morning session, Dr. Moore and Pam (MA) will test the template with scheduled DM patients. How will you measure success of the test: The success of the test will be an immediate default to the clinical guideline/reminder template for 100% of patients with DM seen. Ease in reminder interpretation, accurate status regarding guideline completion, and ease in guideline updating. The DSA Part of the PDSA DO: Pam was ill on Wednesday, so Pat (MA) and Dr. Moore completed the test as planned and provided feedback. Counted default clinical guideline/reminder template for DM patients. Determined accuracy of reminders on the template. STUDY: For 100% of the DM patients, guideline/reminder template appeared as a default mechanism. DM reminder status incorrect for eye exam and vaccines (flu and pneumovax). Both MA & MD stated default clinical guideline/reminder template supported planned care at every visit. Easy to use. ACT: Revise DM eye exam and vaccine reminders and retest with MA and MD on Monday. PDSA Cycle: Self-Management Act • Revise tool • Retest with 2 more patients Plan • Use a SM tool • Tool supports SM process, goal setting • Staff and patient satisfaction, # goals • Select tool, teach staff, use tool with 2 patients Study Do • Staff and patients • Use SM tool with 2 pts liked tool and • Document problems, process, one goal satisfaction, # of goals set per patient • Begin analysis • Want to revise tool of the data • Successful test Plan (P) for Patient-centered interactions PDSA 3: Test the DM self-management tool with patients Objective: Set self-management goals with patients using a tool PLAN: Predictions: Patients with DM can improve self-care when they are taught behaviors to improve DM management and can select a behavior change they want to work on and are confident they can achieve. Who, what, when, where: Use the NYC DOH DM form for teaching DM management; use it to set a goal, and to score confidence. Susan will use the tool on Friday with 2 DM patients (Mather & Thomas) to teach DM management, set one goal, score confidence. How will you measure success of the test: The success of the test will be the completion of the DM self-management tool with at least one goal and stated patient satisfaction with the approach/tool. The DSA Part of the PDSA DO: Test completed as planned with 2 DM patients. Patients and staff asked for feedback. STUDY: One goal set per patient. Patients identified one behavior to work on and were confident (>7.0) they could achieve it. Susan slightly uncomfortable with process but wants to use the tool again to gain comfort with goal setting. ACT: Retest tool with two patients on Friday. Revise tool by end of next week, adding importance score, symptoms & management of hypoglycemia and retest. To Be Considered a PDSA Cycle • The test or observation was planned (including a plan for collecting data). • The plan was attempted. • Time was set aside to analyze the data and study the results. • Action was rationally based on what was learned. Do Study • Reasons for failed tests 1. Change not executed well – re-look at plan 2. Support processes inadequate 3. Hypothesis/hunch wrong • Collect data during the “Do” of the PDSA Cycle to help differentiate these situations • Follow improvement trend of measure graphs • Spread changes when they work well across providers, care teams, patient population 0 Feb-11 Jan-11 Dec-10 Nov-10 Oct-10 Sep-10 Aug-10 Jul-10 Jun-10 May-10 Apr-10 Mar-10 Feb-11 Jan-11 Dec-10 Nov-10 Oct-10 Sep-10 Feb-11 Jan-11 Dec-10 Nov-10 Oct-10 Sep-10 Aug-10 Jul-10 Jun-10 May-10 Apr-10 Mar-10 Feb-10 Jan-10 Dec-09 Nov-09 Oct-09 Sep-09 Aug-09 Jul-09 Jun-09 80 Aug-10 Jul-10 Jun-10 May-10 Apr-10 Mar-10 Feb-10 Jan-10 Dec-09 Nov-09 Oct-09 Sep-09 Aug-09 Jul-09 Jun-09 May-09 Apr-09 Apr-09 May-09 100 Feb-10 Jan-10 Dec-09 Nov-09 Oct-09 Sep-09 Aug-09 Jul-09 Jun-09 May-09 Apr-09 Mar-09 0 Mar-09 0 Mar-09 Pct of DM patients with latest A1C >9 DM Outcome Measures PDSA 2 60 40 20 100 Pct of DM patients with latest BP <130/80 80 60 40 20 100 Pct of DM patients with latest LDL <100 80 60 40 20 What changes do you plan to test by next Tuesday? Some PDSA Ideas • Population alert on medical records • Template/Flow sheet with embedded guidelines • Pre-visit planning • Provider-care team (nurse, MA) huddles • Identifying patients not seen in past 6-12 months that need follow-up care • Standing orders • Planned care at every visit • Self-management tool • Risk assessment process, tool