Major Case Study: COPD - Emily Brantley Dietetic Intern: Andrews
advertisement

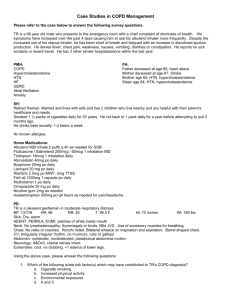
MEDICAL CASE STUDY : COPD EMILY BRANTLEY DIETETIC INTERN ANDREWS UNIVERSITY INTRODUCTION NM is a 62 year old white female who is 160.02 centimeters tall weighing 107.2 kilograms. She was admitted to Winter Park Memorial Hospital with shortness of breath, respiratory abnormality, diarrhea and hypokalemia. I have chosen to conduct a case study on this patient because of the multiple complications that she is facing such as Diabetes Mellitus, Addison’s disease, Irritable Bowel Syndrome and IgA Deficiency. This case study began on December 5, 2013 and ended two visits later on December 6, 2013. Although she has been diagnosed with many health complications, the primary problem that NM has is Chronic Obstructive pulmonary disease, or COPD. NM has other comorbidities that are comparable in importance. Nevertheless, she is most often admitted to the hospital for exacerbation of COPD. Therefore, COPD is the focus of this study. SOCIAL HISTORY NM is a Christian woman who lives at home with her husband and pet parakeet. She is currently on Medicare. She is a retired RN. Her three children are all adults and live within the region. NM is a former smoker but Medical records indicate that she does not smoke or drink alcohol anymore. NORMAL ANATOMY AND PHYSIOLOGY OF APPLICABLE BODY FUNCTIONS COPD is characterized by slow, progressive obstruction of the airways. There are two physical conditions that make up COPD. The first is known as Emphysema and it is characterized by abnormal, permanent enlargement and destruction of the alveoli. The second is chronic bronchitis where there is a progressive cough with inflammation of bronchi and other lung changes. In both cases, the disease limits the airflow and frequently, both illnesses coexist as part of this disorder.1&2 PAST MEDICAL HISTORY (INCLUDE PREVIOUS ADMISSIONS TO HOSPITAL) Past medical history indicates that NM initially received the diagnosis of COPD in 1997. According to the American Thoracic Society, comorbidities such as cardiac disease, diabetes mellitus, hypertension, and psychological disorders are commonly reported in patients with COPD, but with great variability in reported prevalence. Along with the original diagnosis, NM also has also been diagnosed with Diabetes Mellitus. The evidence for an interaction between diabetes and COPD is supported by studies that demonstrate reduced lung function as a risk factor for the development of diabetes. In fact, smoking has been established as a risk factor for both COPD and Diabetes Mellitus. 3 NM has been hospitalized six times within the past year for episodes of pneumonia. When compared to other chronic diseases, COPD is more frequently associated with pneumonia. Corticosteroids are standard of care for acute exacerbations of COPD, but their role in the management of patients with COPD with pneumonia is less defined. 3 NM also suffers from Gastro-esophageal reflux disease (GERD). An increased prevalence of GERD has been reported in patients with COPD. A recent study of 421 patients with severe COPD using 24-hour esophageal pH monitoring showed that 62% had pathological GERD, and notably 58% of the patients reported no symptoms of GERD.3 Besides COPD, Diabetes Mellitus and GERD as previously mentioned above, NM’s past medical history also included other comorbidities. They are as follows: Bronchial Asthma Adrenal Insufficiency Coronary Artery Disease Trachaeomalacia Addison’s disease Hypothyroidism Bipolar Disorder Irritable Bowel syndrome Vascular stent placement Hyperlipidemia Hyperthyroidism Anemia PRESENT MEDICAL STATUS AND TREATMENT Theoretical Discussion of Disease Condition COPD is the fourth leading cause of death in America. COPD is also more prevalent in women.3&4 The primary risk factor in the development of COPD is smoking. Beyond the cessation of smoking, it has been shown that the inflammatory stress continues to damage the lung tissue. Other risk factors include air pollution, secondhand smoke, history of childhood infections, and occupational exposure to certain industrial pollutants. Although normal lung function gradually declines with age, individuals who are smokers have a more rapid decline—twice the rate of nonsmokers. Low body weight has also been shown to be a risk factor for the development of COPD even after adjusting for other potential risk factors including smoking and age.2 Malnourished patients with COPD experience worsened respiratory muscle strength, decreased ventilator drive and response to hypoxia, and altered immune function. 1, 5 & 6 Usual Treatment of Condition An early and accurate diagnosis of COPD is the key to treatment. Quitting smoking is the single most important thing that can be done to help treat COPD. 7 Once identified, the usual treatment of COPD is composed of four main goals for effective management. They are to: 1. Assess and monitor the disease 2. Reduce risk factors 3. Maintain stable COPD and respiratory status 4. Manage any exacerbations Once the disease progresses, rehabilitation programs along with oxygen therapy are used as treatment. Additionally there are numerous medication prescriptions that include bronchodilators, glucocorticosteroids, mucolytic agents, and antibiotics to treat infections. In cases where COPD may be advanced, there is an option for surgical intervention, such as a lung transplant.1 Patient’s Symptoms upon Admission Leading to Present Diagnosis NM was admitted with shortness of breath, cough, diarrhea, hypokalemia and fever. The patient revealed that one of the possible causes of her diarrhea may be the fact that she had “been around a couple of people with Clostridium Difficile.” NM also showed symptoms of hyperlipidemia and hypertension – High blood pressure is a complication of COPD. 6 Hyperglycemia is a side effect of steroid therapy for COPD. Steroids can increase the blood sugar making diabetes harder to control.8 Laboratory Findings and Interpretation The lab values for NM on December 5th were as follows: Lab Value Normal Range Sodium 138 135 to 145 milliequivalents per liter (mEq/L) Potassium 3.5 3.7 to 5.2 mEq/L BUN 16 7 to 20 mg/dL Creatinine 0.69 0.6 to 1.1 mg/dL for women Blood Glucose 152 70 to 100 milligrams per deciliter (mg/dL) Accuchecks 70 to 100 milligrams per deciliter (mg/dL) 188, 130, 239, 282, 279, 233 1 Medications Below is a table that explains the uses and purpose of NM’s medications along with their food/drug interactions and side effects. Drug Name Dosage Uses Depakote ER (Valproic Acid) 1000 mg Lexapro (Escitaloprem) 5 mg Valproic acid is in the anticonvulsant class of medications. Valproic acid is used to treat mania (episodes of frenzied, abnormally excited mood) in people with bipolar disorder. It works by increasing the amount of a certain natural substance in the brain. Escitalopram is in a class of antidepressants called selective serotonin reuptake inhibitors (SSRI’s). It is used to treat depression and generalized anxiety disorder. It works by increasing the amount of serotonin, a natural substance in the brain that helps maintain mental balance. Fludrocortisone is used to treat Addison's disease and syndromes where excessive amounts of sodium are lost in the urine. It is a corticosteroid, used to help control the amount of sodium and fluids in the body. It works by decreasing the amount of sodium that is lost (excreted) in urine. Fluticasone is in a class of medications called steroids. Salmeterol is in a class of medications called long-acting beta-agonists (LABAs). It works by relaxing and opening air passages in the lungs, making it easier to breathe. The combination of fluticasone and salmeterol is used to prevent wheezing, Florinef 0.1 mg (Fludrocortison Acitate) Fluticasone – salemeterol 2 puffs Food/Drug interaction Continue normal diet Continue normal diet Side Effects Drowsiness, dizziness, headache, diarrhea, constipation, changes in appetite, weight changes, back pain, agitation, mood swings, abnormal thinking, uncontrollable shaking of a part of the body, loss of coordination, uncontrollable movements of the eyes, blurred or double vision, ringing in the ears, hair loss Dizziness, sweating, nausea, vomiting, tremor, drowsiness, fast or pounding heartbeat, seizures, confusion, forgetfulness, fast breathing, coma (loss of consciousness for a period of time) Doctors may instruct to follow a LowSodium, LowSalt, PotassiumRich, or HighProtein diet. Upset stomach, stomach irritation, vomiting, headache, dizziness, insomnia, restlessness, depression, anxiety, acne, increased hair growth, easy bruising, irregular or absent menstrual periods Talk to doctor about eating grapefruit or drinking grapefruit juice runny nose, sneezing, sore throat, throat irritation, sinus pain, headache, nausea, vomiting, diarrhea, stomach pain, muscle and bone pain, dizziness, weakness, tiredness, sweating, tooth pain, red or dry eyes, shaking of a part of the body that cannot be controlled, sleep problems Metronidazole Flagyl 500 mcg Insulin lispro (Humalog) Medium scale Misoprostal (Cytotec) 100 mcg Monlelukast (Singulair) 10 mg shortness of breath, coughing, and chest tightness caused by asthma and chronic obstructive pulmonary disease. It works by reducing swelling in the airways. Metronidazole eliminates bacteria and other microorganisms that cause infections of the reproductive system, gastrointestinal tract, skin, vagina, and other areas of the body. Antibiotics will not work for viral colds, flu, or other viral infections. Insulin lispro is used to treat type 1 and type 2 diabetes. In patients with type 2 diabetes, insulin lispro may be used with another type of insulin or with oral medication(s) for diabetes. Insulin lispro is a short-acting, man-made version of human insulin. Insulin lispro works by replacing the insulin that is normally produced by the body and by helping move sugar from the blood into other body tissues where it is used for energy. Misoprostol is used to prevent ulcers in people who take certain arthritis or pain medicines, including aspirin, which can cause ulcers. It protects the stomach lining and decreases stomach acid secretion. Montelukast is in a class of medications called leukotriene receptor antagonists (LTRAs). It works by blocking the action of substances in the body that cause the Continue normal diet Vomiting, diarrhea, upset stomach, loss of appetite, dry mouth; sharp, unpleasant metallic taste, dark or reddishbrown urine, furry tongue; mouth or tongue irritation, numbness or tingling of hands or feet Important to eat a consistent carbohydrate diet. Skipping or delaying meals or changing the amount or kind of food eaten, especially carbohydrates can cause problems with blood sugar control. Talk to doctor about decreasing high acid foods. Redness, swelling, or itching in the place where insulin is injected. Changes in the feel of skin such as skin thickening or indentation in the skin, weight gain, constipation Continue normal diet headache, dizziness, heartburn, stomach pain, tiredness Diarrhea, headache, stomach pain, upset stomach, gas, vomiting, constipation, indigestion Pantoprazole (Protonix oral) 40 mg Potassium chloride 40 mEq RisperiDONE (RisperDAL) 0.5 mg Rosuvastatin (Crestor) 5 mg symptoms of asthma and allergic rhinitis. Used to prevent wheezing, difficulty breathing, chest tightness, and coughing caused by asthma; prevent bronchospasm during exercise; relieve symptoms of seasonal, and perennial allergic rhinitis. Pantoprazole is in a class of medications called protonpump inhibitors. It works by decreasing the amount of acid made in the stomach. Pantoprazole is used to treat symptoms of (GERD), allow the esophagus to heal, and prevent further damage to the esophagus; Used to treat conditions where the stomach produces too much acid, such as Zollinger-Ellison syndrome. Electrolyte mineral in tablet form used to treat deficiency. Risperidone is in a class of medications called atypical antipsychotics. It works by changing the activity of certain natural substances in the brain. It is used to treat the symptoms of schizophrenia, episodes of mania or mixed episodes in bipolar disorder. Risperidone is also used to treat behavior problems such as aggression, selfinjury, and sudden mood changes in teenagers and children 5 to 16 years of age. Rosuvastatin is in a class of medications called HMG- Continue normal diet headache, dizziness, nausea, vomiting, gas, joint pain Doctor may recommend foods high in potassium foods such as bananas Continue normal diet Muscle cramps or spasms, abnormal heart rhythms, fatigue, constipation Low cholesterol or Constipation, heartburn, dizziness, difficulty falling asleep Drowsiness, dizziness, nausea, vomiting, diarrhea, constipation, heartburn, dry mouth, increased saliva, increased appetite, weight gain, stomach pain, anxiety, agitation, restlessness, dreaming more than usual, difficulty falling asleep or staying asleep, decreased sexual interest or ability, breast milk production, vision problems, muscle or joint pain, dry or discolored skin, difficulty urinating NaCl 1 gm Tolterodine (Detrol LA) 2 mg Voriconazole 200 mg CoA reductase inhibitors (statins). It works by slowing the production of cholesterol in the body to decrease the amount of cholesterol that may build up on the walls of the arteries and block blood flow to the heart, brain, and other parts of the body. It is used together with diet, weight-loss, and exercise to reduce the risk of heart attack and stroke and to decrease the chance that heart surgery will be needed in people who have heart disease or who are at risk of developing heart disease. Combination of sodium and chloride in tablet form to assist with hydration and elecrolyte balance. Tolterodine is in a class of medications called antimuscarinics. It is used to relieve urinary difficulties, including frequent urination and inability to control urination. It works by preventing bladder contraction. Voriconazole is in a class of antifungal medications called triazoles. It works by slowing the growth of the fungi that cause infection. It is used to treat serious fungal infections such as invasive aspergillosis and esophageal candidiasis. low saturated foods diet. or staying asleep, depression, joint pain, cough, memory loss or forgetfulness, confusion Caution with foods high in sodium, restrict use of table salt. No side effects known. Dry mouth, blurred vision, upset stomach, headache, constipation, dry eyes, dizziness Talk to doctor about eating grapefruit and drinking grapefruit juice while taking this medicine Blurred or abnormal vision, difficulty seeing colors, sensitivity to bright light, diarrhea, vomiting, headache, dizziness, dry mouth, flushing 9 Observable Physical and Psychological Changes in Patient Upon observation, Nm physically looked well nourished. She did not appear to have difficulty breathing until after she spoke for a long period of time. She did have a severe cough that she tried to conceal. NM was a very agreeable patient for both psychological interviews. In spite of her COPD diagnosis and all of the multiple medical comorbidities that NM faced, she still presented a positive attitude and spoke openly about her faith. Treatment NM received a chest x ray that revealed consolidation in the left lung and midline lung level. Once this was identified, she was admitted to the hospital from the Emergency room for treatment. She was started on IV steroids, IV antibiotics, flagyl and nebulizers around the clock to see how she progressed. MEDICAL NUTRITION THERAPY Nutrition History NM stated that beginning in March 2012, she began intentionally losing weight by following a PCP prescribed commercial diet known as Optifast. Optifast offers shakes, protein bars and soups. With this regimen, NM has lost 70 pounds since March 2012. At home, NM usually sticks to her Optifast food items for breakfast, lunch and snacks between meals. For dinner, however, she shares a meal with her husband. He is a professional chef who is control of purchasing groceries and prepares dinner most nights. Analysis of Previous Diet Below is an example of a typical day for NM with her Optifast products incorporated multiple times during the day. Time Meal 8:00 Breakfast AM Food Item 1 cup Oatmeal 160 31 5 3 160 20 14 3 108 10 0 3 0 0 12 0 1 large apple 110 29 1 0 Optifast 800 Bar Optifast 800 Ready to Drink Shake Optifast 800 Soup 8 Wheat Thins ¾ cup Raw Carrots 1 Tbs Ranch dressing 170 21 14 5 160 20 14 3 170 60 25 71 20 10 5 1 14 1 1 0 4 2 0 8 170 21 14 5 2 Tbs Alfredo Sauce ¾ cup Yellow Squash ¾ cup Green Beans 220 125 25 25 43 1 5 5 8 3 1 1 1 0 0 0 ½ cup Grapes 104 27 1 0 3 oz Cheddar 147 2020 2 264 21 113 6 52 Optifast 800 Ready to Drink Shake 3 tsp Margarine 3 packets Splenda 11:00 Mid-morning AM snack 1:30 Lunch PM 4:30 Mid-afternoon PM snack 7:00 Dinner PM 9:30 HS Snack PM Totals for the Day Calories Carbohydrates Protein Fat (kcal) (grams) (grams) (grams) Optifast 800 Bar 1 cup Spaghetti 1& 11 Current prescribed diet NM was on steroid therapy to treat her COPD. Because of the steroid therapy, NM was admitted with consistently high blood glucose levels. For this reason, doctor’s orders were given for an Average Diabetic Diet for the duration of her stay at Winter Park Memorial Hospital. An Average Diabetic Diet allows the patient to select up to 60-75 grams of carbohydrates for each meal. NM’s diet order remained the same for her entire stay. Objectives of dietary treatment The objective of the Average Diabetic diet is to maintain NM’s blood sugars within normal limits or as close as possible to normal levels. This may have proved an arduous task given the steroid therapy that NM was undergoing to treat her COPD. Finger-stick blood sugar levels referred to as “Accuchecks” ranged inconsistently from 130 to 289 as seen on the lab values table above. Patient’s Physical and Psychological Response to Diet NM stated that at home, she followed an eating pattern similar to that of the Average Diabetic Diet but with the addition of snacks in between meals. She denied facing vomiting or constipation while on this diet. She did admit to experiencing diarrhea and nausea upon admission to the hospital. As previously mentioned, NM believed she was exposed to Clostridium Difficile, to which she attributes to the cause of having diarrhea. List nutrition-related problems with supporting evidence COPD: Increased energy expenditure related to increased energy requirements during COPD exacerbation as evidenced by estimated resting energy expenditure greater than predicted needs. Evaluation of Present Nutritional Status According to the diet analysis table above, NM was meeting her increased caloric needs for COPD. Additionally, her diarrhea subsided by day two of hospitalization. Per lab values as those noted above in the table, there did not appear to be any indication of dehydration. Kcal/Protein Guidelines Nutritional needs are often increased in COPD due to the increased work of breathing. Optimal nutritional status plays an important role in maintaining the integrity of the respiratory system and in allowing maximal participation in daily living.1 Caloric requirements for COPD should be individually determined based on patient age, weight and gender, the extent of protein energy malnutrition loss of lean body mass, current medications and other acute or chronic medical conditions. The Mifflin St. Jeor equation can be used to estimate the REE. In patients with COPD, this calculation may underestimate the caloric requirements because of the caloric increase from metabolically active tissue in COPD. To compensate for this underestimation, a stress activity factor may be added according to the degree of stress. Furthermore, in most cases the total calorie intake of the COPD patient is more important than the source from calories. For maintenance 1.33 x REE or 25/35 calories per kilogram is appropriate for the needs of the COPD patient. Protein is recommended at 1.0-1.5 grams per kilogram of body weight for maintenance.1 Below is a chart of how NM’s needs were clinically calculated during her hospital admission on December 5th through the 6th. Kcal calculations Protein calculations for adjusted body weight Fluid requirements 1926-2408 66-79 1500 ml per physician Need for Alternative Feeding Methods and the Patient’s Nutrition Education Process Since NM was in fact meeting the additional needs required for COPD, I do not believe that there was any need for alternative feedings such as tube feeding. Moreover, in explaining the prescribed diabetic diet to NM, no type of barrier to learning was identified. PROGNOSIS NM expressed her motivation to continue to follow a diet similar to that of the Average Diabetic Diet upon her return home as long as her increased COPD needs were met. She was aware of the effects of steroid therapy on her blood sugar levels. In fact, NM clearly verbalized her understanding on the use of steroids, their effects on increasing blood sugar levels and the importance of meal planning especially around carbohydrates. This was more of a motivating factor for her to continue monitoring her diet on discharge. SUMMARY From this study, I learned how very serious COPD is. It was once explained to me some time ago that COPD was like a gradual suffocating in a pillow. Seeing NM experiencing shortness of breath during the interviews or when speaking to me during the interviews made me realize that even the slightest amount of energy requires oxygen. Imagine not being able to breathe to conduct the simplest activities of daily living! In addition to other medical issues as NM had, it made me realize how important nutrition energy is needed for healing. BIBLIOGRAPHY 1. Mahan LK, Escott-Stump S, Raymond JL. Krause’s Food, Nutrition and Diet Therapy, 13th Edition, Philadelphia, Pa: Elsevier; 2012 2. Nelms M, Sucher KP, Lacey K, Roth SL. Nutrition Therapy and Pathophysiology, 2nd Edition. Cengage Learning, Inc: 2010. 3. Chatila WM, Thomashow BM, Make BJ. Comorbidities in Chronic Obstructive Pulmonary Disease. Journal of the American Thoracic Society. 2008 May 1; 5(4): 549-555 4. Centers for Disease Control. Chronic Obstructive Pulmonary Disease (COPD) Data and Statistics. Available at: http://www.cdc.gov/copd/data.htm. Accessed December 29, 2013. 5. American Society for Parenteral and Enteral Nutrition. Disease-Related Malnutrition and Enteral Nutrition Therapy. Available at: http://www.nutritioncare.org/index.aspx?id=5696. Accessed January 5, 2014. 6. Mayo Clinic. Disease and Conditions: COPD. Available at: http://www.mayoclinic.org/diseasesconditions/seo/basics/symptoms/con-20032017. Accessed January 8, 2014. 7. National Institutes of Health: National Heart Lung and Blood Institute. How Is COPD Treated? Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/copd/treatment.html. Accessed January 8, 2014. 8. British Lung Foundation. Steroids. Available at: http://www.blf.org.uk/Page/Steroids. Accessed December 29, 2013. 9. MedlinePlus: A service of the U.S. National Library of Medicine From the National Institutes of HealthNational Institutes of Health. Drugs and Supplements. Available at: http://www.nlm.nih.gov/medlineplus/druginfo/drug_Ca.html 10. U.S. National Library of Medicine. Drug Information from the National Library of Medicine. Available at: https://www.nlm.nih.gov/learn-about-drugs.html. Accessed January 8, 2014. 11. Optifast. Product Information. Available at: http://www.optifast.com/Pages/index.aspx. Accessed Januery 7, 2014. Images 1. http://sciencelife.uchospitals.edu/2013/05/07/qa-dr-christopher-wigfield-on-the-future-of-lungtransplantation/ 2. http://www.nlm.nih.gov/medlineplus/ency/imagepages/19376.htm 3. http://www.cdc.gov/copd/data.htm 4. http://www.optifast.com/Pages/index.aspx