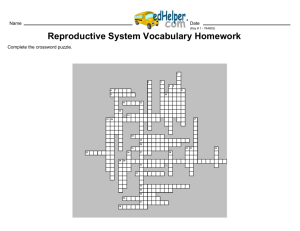
ch28 outline
advertisement

CHAPTER 28 LECTURE OUTLINE I. INTRODUCTION A. Sexual reproduction is a process in which organisms produce offspring by means of germ cells called gametes. B. The organs of reproduction are grouped as gonads (produce gametes and secrete hormones), ducts (transport, receive, and store gametes), and accessory sex glands (produce materials that support gametes). C. Gynecology is the specialized branch of medicine concerned with the diagnosis and treatment of diseases of the female reproductive system. Urology is the study of the urinary system but also includes diagnosis and treatment of diseases and disorders of the male reproductive system. Andrology is the study of only male reproductive diseases. II. MALE REPRODUCTIVE SYSTEM A. The male structures of reproduction include the testes, a system of ducts (ductus epididymis, ductus deferens, ejaculatory duct, urethra), accessory sex glands (seminal vesicles, prostate gland, bulbourethral glands), and several supporting structures, including the penis (Figure 28.1). B. Scrotum 1. The scrotum is a cutaneous outpouching of the abdomen that supports the testes; internally, a vertical septum divides it into two sacs, each containing a single testis (Figures 28.2). 2. The reproduction and survival of spermatozoa require a temperature that is lower than normal core body temperature. The temperature of the testes is regulated by the cremaster muscle, which elevates them and brings them closer to the pelvic cavity or relaxes, causing the testes to move farther from the pelvic cavity. C. Testes 1. The testes, or testicles, are paired oval-shaped glands (gonads) in the scrotum (Figure 28.3). 2. The testes develop high on the embryo’s posterior abdominal wall and usually begin their descent into the scrotum through the inguinal canals during the latter half of the seventh month of fetal development. 3. The testes contain seminiferous tubules (in which sperm cells are made) (figure 28.4). 4. Embedded among the spermatogenic cells in the tubules are large Sertoli cells or sustentacular cells (Figure 28.4). a. The tight junctions of these cells form the blood-testis barrier that prevents an immune response against the surface antigens on the spermatogenic cells. b. The sustentacular cells also nourish spermatocytes, spermatids, and spermatozoa; mediate the effects of testosterone and follicle stimulating hormone on spermatogenesis; phagocytose excess spermatids cytoplasm as development proceeds; control movements of spermatogenic cells and the release of spermatozoa into the lumen of the seminiferous tubule; and secrete fluid for sperm transport and the hormone inhibin. c. The Leydig cells or interstitial endocrinocytes found in the spaces between adjacent seminiferous tubules secrete testosterone (Figure 28.4). 5. Failure of the testes to descend is called cryptorchidism, involving one or both testes. (Clinical Connection) 6. Spermatogenesis is the process by which the seminiferous tubules of the testes produce haploid sperm. a. It begins in the diploid spermatogia (stem cells). They undergo mitosis to reserve future stem cells and to develop cells (2n primary spermatocytes) for sperm production (Figure 28.5). b. The diploid primary spermatocytes undergo meiosis I forming haploid secondary spermatocytes. c. Meiosis II results in the formation of the haploid spermatids. The spermatids are connected by cytoplasmic bridges. d. The final stage of spermatogenesis is spermiogenesis which is the maturation of the spermatids into sperm. e. The release of a sperm from its connection to a Sertoli cell is known as spermiation. 7. Sperm a. Mature sperm consist of a head, midpiece, and tail (Figure 28.6). They are produced at the rate of about 300 million per day and, once ejaculated, have a life expectancy of 48 hours within the female reproductive tract. Their function is to fertilize a secondary oocyte. D. Hormonal Control of the testes 1. At puberty, gonadotropin releasing hormone stimulates anterior pituitary secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH). FHS initiates spermatogenesis, and LH assists spermatogenesis and stimulates production of testosterone. Figure 28.7 summarizes the hormonal relationships of the hypothalamus, pituitary gland, and testes. 2. Testosterone controls the growth, development, functioning, and maintenance of sex organs; stimulates bone growth, protein anabolism, and sperm maturation; and stimulates development of male secondary sex characteristics. Negative feedback systems regulate testosterone production (Figure 28.8). 3. Inhibin is produced by sustentacular (Sertoli) cells. Inhibition of FSH by inhibin helps to regulate the rate of spermatogenesis. III. Reproductive System Ducts in Males A. The duct system of the testes includes the seminiferous tubules, straight tubules, and rete testis. B. Epididymis 1. The epididymis is a comma-shaped organ that lies along the posterior border of the testis (Figure 28.3). 2. Sperm are transported out of the testes through the efferent ducts in the epididymis which empty into a single tube called the ductus epididymis. 3. The ductus epididymis is lined by stereocilia and is the site of sperm maturation and storage; sperm may remain in storage here for at least a month, after which they are either expelled or degenerated and reabsorbed. C. Ductus Deferens 1. The ductus (vas) deferens, or seminal duct, stores sperm and propels them toward the urethra during ejaculation (Figures 28.3 and 28.9). D. Spermatic cord 1. The spermatic cord is a supporting structure of the male reproductive system, consisting of the ductus deferens, the testicular artery, autonomic nerves, veins that drain the testes, lymphatic vessels, and the cremaster muscle (Figure 28.2). 2. The principle method of sterilization of males is a vasectomy in which both ductus deferens are cut and tied. .This results in no sperm entering the ejaculate(Clinical Connection) E. Ejaculatory ducts 1. The ejaculatory ducts are formed by the union of the ducts from the seminal vesicles and ducti deferens; their function is to eject spermatozoa into the prostatic urethra (Figure 28.9). F. Urethra 1. The male urethra is the shared terminal duct of the reproductive and urinary systems which serves as a passageway for semen and urine. The male urethra is subdivided into three portions: prostatic, membranous, and spongy (cavernous) (Figures 28.1). G. Accessory Sex Glands 1. The seminal vesicles secrete an alkaline, viscous fluid that contains fructose, prostaglandins, and clotting proteins (Figure 28.9). a. The alkaline nature of the fluid helps to neutralize acid in the male urethra and female reproductive tract. b. The fructose is for ATP production by sperm. c. Prostaglandins contribute to sperm motility and viability. d. Semenogelin is the main protein that causes coagulation of semen after ejaculation. 2. The prostate gland (Figure 28.9) secretes a milky, slightly acidic fluid that contains: (1) citric acid, which can be used by sperm for ATP production; (2) acid phosphatase; and (3) several proteolytic enzymes, such as prostate-specific antigen (PSA), pepsinogen, lysozyme, amylase, and hyaluronidase which liquefy coagulated semen. 3. The bulbourethral (Cowper’s) glands secrete mucus for lubrication and an alkaline substance that neutralizes acid (Figure 18.9). H. Semen (seminal fluid) is a mixture of spermatozoa and accessory sex gland secretions that provides the fluid in which spermatozoa are transported, provides nutrients, and neutralizes the acidity of the male urethra and female vagina. 1. Semen contains an antibiotic, seminal plasmin, and prostatic enzymes that coagulate and then liquefy semen to aid in its movement through the uterine cervix. 2. Once ejaculated, liquid semen coagulates within 5 minutes due to the presence of clotting proteins from the seminal vesicles. 3. After about 10-20 minutes, semen reliquifies because PSA and other proteolytic enzymes produced by the prostate gland break down the clot. I. Penis 1. The penis is the male organ of copulation that consists of a root, body, and glans Penis. It is used to introduce spermatozoa into the vagina (Figure 28.10). 2. Covering the glans penis is the loosely fitting prepuce, or foreskin. Circumcision is a surgical procedure in which part of the entire prepuce is removed (for either religious or hygienic reasons). There is no consensus among physicians regarding the need for circumcision or the use of anesthesia during the procedure (Clinical Connection). 3. Expansion of its blood sinuses under the influence of sexual excitation is called erection; ejaculation, propulsion of semen from the urethra to the exterior, is a sympathetic reflex. 4. Premature ejaculation results from anxiety, other psychological factors and an over sensitive glans. (Clinical Connection). IV. FEMALE REPRODUCTION SYSTEM A. The female organs of reproduction include the ovaries (gonads), uterine (Fallopian) tubes, uterus, vagina, vulva, and mammary glands (Figure 28.11). B. Ovaries 1. The ovaries are paired glands that are homologous to the testes. 2. The ovaries are located in the upper pelvic cavity, on either side of the uterus. They are maintained in position by a series of ligaments (Figure 28.12). 3. The histology of the ovary is illustrated in Figure 28.13. a. The germinal epithelium covers the surface of the ovary but does not give rise to ova. It is followed by the tunica albuginea, ovarian cortex (contains ovarian follicles), and ovarian medulla (contains blood vessels, lymphatics, and nerves). b. Ovarian follicles, in various degrees of development, lie in the cortex and contain oocytes at different stages of gametogenesis (Figure 28.14) c. A mature (Graafian) follicle expels a secondary oocyte by a process called ovulation. d. A corpus luteum contains the remnants of an ovulated follicle and produces progesterone, estrogens, relaxin, and inhibin until it degenerates into a corpus albicans. 4. Oogenesis and follicular development a. Oogenesis occurs in the ovaries. It results in the formation of a single haploid secondary oocyte. b. The oogenesis sequence includes reduction division (meiosis I), equatorial division (meiosis II), and maturation (Figure 28.15). c. While oogenesis is occurring, the follicle cells surrounding the oocyte are also undergoing developmental changes (Figure 28.15). The sequence of follicular cell changes is: primordial, primary, secondary, and mature (Graffian) follicles, and corpus luteum and corpus albicans. d. Table 28.1 summarizes the events of oogenesis and follicular development. e. Ovarian cysts , fluid filled sacs in the ovary, are relatively common and usually not cancerous. (Clinical Connection) C. Uterine Tube 1. The uterine (Fallopian) tubes transport ova from the ovaries to the uterus and are the normal sites of fertilization (Figure 28.16). 2. Histologically the uterine tubes are composed of three layers: the internal mucosa, the middle muscularis, and the outer serosa (Figure 28.17) 3. Ciliated cells and peristaltic contractions help move a secondary oocyte toward the uterus. D. Uterus 1. The uterus (womb) is an organ the size and shape of an inverted pear that functions in the transport of spermatozoa, menstruation, implantation of a fertilized ovum, development of a fetus during pregnancy, and labor (Figure 28.16). 2. Anatomical subdivisions of the uterus include the fundus, body, isthmus, and cervix. 3. The uterus is normally held in position by a series of ligaments. 4. Uterine prolapse is a downward displacement of the uterus. It has many causes and may be characterized as first degree (mild), second degree (marked), or third degree (complete). The treatment depends on the degree of prolapse (Clinical Connection). 5. Histologically, the uterus consists of an outer promethium, middle myometrium, and inner endometrium (Figure 28.18). a. The myometrium consists of three muscle layers. b. The endometrium is divided into the stratum functionalis (shed during menstruation) and the stratum basalis (gives rise to a new stratum functionalis after each menstruation). 6. Blood is supplied to the uterus by the uterine arteries and their numerous branches and is drained by the uterine veins (Figure 28.19). 7. Secretory cells of the mucosa of the cervix produce a cervical mucus (a mixture of water, glycoprotein, serum-type proteins, lipids, enzymes, and inorganic salts) which, when thin, is more receptive to sperm and which, when thick, forms a cervical plug that physically impedes sperm penetration. a. The cervical mucus supplements the energy needs of the sperm. b. Both the cervix and the mucus serve as a sperm reservoir, protect sperm from the hostile environment of the vagina, and protect sperm from phagocytes. c. The cervix and the mucus also play a role in capacitation. 8. Hysterectomy refers to surgical removal of the uterus and is the most common gynecological operation (Clinical Connection). E. Vagina 1. The vagina functions as a passageway for spermatozoa and the menstrual flow, the receptacle of the penis during sexual intercourse, and the lower portion of the birth canal (Figures 28.1, 28.19). 2. The mucosa of the vagina is continuous with that of the uterus and lies in a series of transverse folds called rugae. a. Mucosa dendritic cells are APCs (antigen-presenting cells) that participate in the transmission of viruses, such as HIV, to a female during intercourse with an infected male. b. The mucosa contains large stores of glycogen which decompose into organic acids which set up a hostile acid environment for sperm. Alkaline components of semen neutralize the acidity and increase sperm viability. 3. The vaginal orifice is often partially covered by a thin fold of vascularized mucous membrane called the hymen. If the orifice is completely covered, this imperforate hymen must be surgically opened to permit menstrual flow (Figure 28.20). F. Vulva 1. The term vulva, or pudendum, refers to the external genitalia of the female (Figure 28.20). 2. It consists of the mons pubs, labia majora, labia minora, clitoris, vestibule, vaginal and urethral orifices, hymen, bulb of the vestibule, and the paraurethral (Skene’s), greater vestibular (Bartholin’s), and lesser vestibular glands (Figure 28.21). 3. Table 28.2 summarizes the homologous structures of the male and female reproductive systems. G. Perineum 1. The perineum is the diamond-shaped area between the thighs and buttocks of both males and females that contains the external genitals and anus (Figure 28.21). 2. during childbirth the emerging fetus may cause excessive stretching and tearing of the perineum. A physician may make a surgical incision (episiotomy) in this region to prevent excessive, jagged tears (Clinical Connection). H. Mammary Glands 1. The mammary glands are modified sudoriferous (sweat) glands that lie over the pectoralis major and serratus anterior muscles (Figure 28.22). 2. Milk-secreting cells, referred to as alveoli, are clustered in small compartments (lobules) within the breasts. 3. Myoepithelial cells surround the glands and promote milk expression. 4. The essential functions of the mammary glands are synthesis of milk, secretion and ejection of milk, which constitute lactation. 5. pBreast augmentation is a procedure in the breast size is increased. Breast reduction involves removal of breast tissue (Clinical Connection) 6. Fibrocystic disease is the most common cause of a breast lump in which one or more cysts (fluid-filled sacs) and thickening of alveoli (clusters of milk-secreting cells) develop (Clinical Connection). V. THE FEMALE REPRODUCTIVE CYCLE A. The general term female reproductive cycle encompasses the ovarian and uterine cycles, the hormonal changes that regulate them, and cyclical changes in the breasts and the cervix. 1. The ovarian cycle is a series of events associated with the maturation of an ovum. 2. The uterine (menstrual) cycle involves changes in the endometrium to prepare for the reception of a fertilized ovum. B. Hormonal Regulation of the Female Reproductive Cycle 1. The menstrual and ovarian cycles are controlled by GnRH from the hypothalamus, which stimulates the release of FSH and LH by the anterior pituitary gland (Figure 28.23). a. FSH stimulates the initial development of ovarian follicles and secretion of estrogens by the ovaries. b. LH stimulates further development of ovarian follicles, ovulation, and the secretion of estrogens and progesterone by the ovaries. c. At least six different estrogens have been isolated from the plasma of human females, with three in significant quantities: beta-estradiol, estrone, and estriol. d. Estrogens have several important functions: 1. Promotion of the development and maintenance of female reproductive structures, secondary sex characteristics, and the breasts. 2. Increase protein anabolism and build strong bones. 3. Lower blood cholesterol. 4. Moderate levels of estrogens in the blood inhibit the release of GnRH by the hypothalamus and secretion of LH and FSH by the anterior pituitary gland. e. Progesterone works with estrogens to prepare the endometrium for implantation and the mammary glands for milk synthesis. f. A small quantity of relaxin is produced monthly to relax the uterus by inhibiting contractions (making it easier for a fertilized ovum to implant in the uterus). During pregnancy, relaxin relaxes the pubic symphysis and helps dilate the uterine cervix to facilitate delivery. g. Inhibin inhibits secretion of FSH and GnRH and, to a lesser extent, LH. It might be important in decreasing secretion of FSH and LH toward the end of the uterine cycle. C. Phases of the Female Reproductive Cycle 1. The female reproductive cycle may be divided into four phases (Figure 28.24). a. The menstrual cycle (menstruation) lasts for approximately the first 5 days of the cycle. 1. During this phase, small secondary follicles in each ovary begin to develop. 2. Also during this phase, the stratum functionalis layer of the endometrium is shed, discharging blood, tissue fluid, mucus, and epithelial cells. b. The preovulatory phase, or proliferative phase, is the time between menstruation and ovulation. This phase is more variable in length that the other phases, lasting from days 6-13 in a 28-day cycle. 1. During this phase, primary follicles develop into secondary follicles and a single secondary follicle (occasionally more than one) develops into a vesicular ovarian (Graafian) follicle, or mature follicle. This follicle produces a bulge on the surface of the ovary (Figure 28.13). 2. The dominant follicle continues to increase its estrogen production under the influence of an increasing level of LH (Figure 28.25). 3. During this phase, endometrial repair occurs. c. Ovulation is the rupture of the vesicular ovarian (Graafian) follicle with release of the secondary oocyte into the pelvic cavity, usually occurring on day 14 in a 28-day cycle. 1. The high levels of estrogen during the last part of the preovulatory phase exert a positive feedback on both LH and GnRH to cause ovulation (Figure 28.26). i. GnRH promotes release of FSH and more LH by the anterior pituitary gland. ii. The LH surge brings about the ovulation. d. Following ovulation, the vesicular ovarian follicle collapses (and blood within it forms a clot) to become the corpus hemorrhagicum (Figure 28.25). The clot is eventually absorbed by the remaining follicle cells. In time, the follicular cells enlarge, change character, and form the corpus luteum, or yellow body, under the influence of LH. Stimulated by LH, the corpus luteum secretes estrogens and progesterone. e. The postovulatory phase is the most constant in duration and lasts from days 15-28 in a 28-day cycle, the time between ovulation and onset of the next menstrual period. 1. With reference to the ovaries, this phase of the cycle is also called the luteal phase, during which both estrogen and progesterone are secreted in large quantities by the corpus luteum. f. if fertilization and implantation do not occur, the corpus luteum degenerates and becomes the corpus albicans, or white body. The decreased secretion of progesterone and estrogens then initiates another menstrual phase (uterine and ovarian cycle). g. If fertilization and implantation do occur, the corpus luteum is maintained until the placenta takes over its hormone-producing function. During this time, the corpus luteum, maintained by human chorionic gonadotropin (hCG) from the developing placenta, secretes estrogens and progesterone to support pregnancy and breast development for lactation. Once the placenta begins its secretion, the role of the corpus luteum becomes minor. 1. With reference to the uterus, this phase is also called the secretory phase because of the secretory activity of the endometrial glands as the endometrium thickens in anticipation of implantation. h. Figure 28.26 summarizes the hormonal interactions during the ovarian and uterine cycles. i. Women athletes who train intensively may develop three conditions which disrupt their reproductive cycle. This is known as female athlete triad and consists of amenorrhea, disordered eating, and premature osteoporosis (Clinical ) VI. BIRTH CONTROL METHODS A. Several methods of birth control are available, each with advantages and disadvantages. B. The only method of preventing pregnancy that is 100% reliable is total abstinence, avoidance of sexual intercourse. C. Methods of birth control discussed in the text include 1. surgical sterilization (vasectomy, tubal ligation) 2. hormonal methods (oral contraception, the Norplant implant, Depo-Provera injection, the vaginal ring) 3. intrauterine devices (IUDs) 4. spermacides, barrier methods (condom, vaginal pouch, diaphragm, cervical cap) 5. periodic abstinence (rhythm method, sympto-thermal method) 6. coitus interruptus (withdrawal) 7. induced abortion (including the drug RU 486, or mifepristone). D. A summary of methods of birth control is presented in Table 28.3. VII. DEVELOPMENT OF THE REPRODUCTIVE SYSTEMS A. The gonads develop from intermediate mesoderm and are differentiated into ovaries or testes by about the seventh week of fetal development (Figure 28.27). B. The external genitalia develop from the genital tubercle (Figure 28.28). VIII. AGING AND THE REPRODUCTIVE SYSTEMS A. Puberty refers to the period of time when secondary sexual characteristics begin to develop and the potential for sexual reproduction is reached. B. In females, the reproductive cycle normally occurs once each month from menarche, the first menses, to menopause, the last menses. 1. Between the ages of 40 and 50 the ovaries become less responsive to the stimulation of gonadotropic hormones from the anterior pituitary. As a result, estrogen and progesterone production decline, and follicles do not undergo normal development. 2. In addition to the symptoms of menopause, such as hot flashes, copious sweating, headache, vaginal dryness, depression, weight gain, and emotional fluctuations, with age females also experience increased incidence of osteoporosis, uterine cancer, and breast cancer. C. In males, declining reproduction function is more subtle, with males often retaining reproductive capacity into their 80s or 90s. 1. In males, decreasing levels of testosterone decrease muscle strength, sexual desire, and viable sperm. 2. Prostate disorders are increasingly common with age, particularly benign hypertrophy. IX. DISORDERS: HOMEOSTATIC IMBALANCES A. Reproductive System Disorders in Males 1. Testicular cancer originates in the sperm-producing cells. a. It occurs most commonly in young men between the ages of 15 and 34. b. An early sign is a mass in the testis, often associated with pain or discomfort. All males should perform regular testicular self-exams. 2. Prostate Disorders a. In acute prostatitis, the prostate gland becomes swollen and tender. b. In chronic prostatitis, one of the most common chronic infections in men of the middle and later years, the gland feels enlarged, soft, and very tender with an irregular surface outline. c. Prostate cancer is the leading cause of cancer deaths in men in the United States. 1. A blood test can measure the level of prostate-specific antigen (PSA) in the blood. 2. The amount of PSA increases with the enlargement of the prostate gland and may indicate infection, benign enlargement, or prostate cancer. d. Treatment for prostate cancer may involve surgery, radiation, hormonal therapy, or chemotherapy. 3. Erectile dysfunction, previously termed impotence, is the consistent inability of an adult male to ejaculate or to attain or hold an erection long enough for sexual intercourse B. Reproductive System Disorders in Females 1. Premenstrual syndrome (PMS) refers to severe physical and emotional distress that occurs during the postovulatory (luteal) phase of the female reproductive cycle. 2. Endometriosis is characterized by the growth of endometrial tissue outside the uterus. a. The tissue enters the pelvic cavity via the open uterine tubes and may be found in any of several sites - on ovaries, rectouterine pouch, surface of the uterus, sigmoid colon, pelvic and abdominal lymph nodes, cervix, abdominal wall, kidneys, and/or urinary bladder. b. Symptoms include premenstrual pain or unusual menstrual pain. 3. Breast cancer is the second-leading cause of death from cancer in United States women. a. It is seldom seen before age 30, but its occurrence rises rapidly after menopause. b. Two genes increase susceptibility to breast cancer: BRCA1 (breast cancer 1) and BRCA2. Mutation of BRCA1 also confers high risk for ovarian cancer. c. Early detection - especially by breast self-examination and mammography is still the most promising method to increase the survival rate for breast cancer. d. The factors that increase the risk of breast cancer development include family history of breast cancer, especially in a mother or sister; never having a child or having a first child after age 35; previous cancer in one breast; exposure to ionizing radiation, such as x-rays; excessive alcohol intake; and cigarette smoking. e. Treatment for breast cancer may involve hormone therapy, chemotherapy, radiation therapy, lumpectomy (removal of just the tumor and immediate surrounding tissue), a modified or radical mastectomy (removal of part or all of the affected breast, along with underlying pectoral muscles and the axillary lymph nodes in the latter case), or a combination of these. Radiation treatment and chemotherapy may follow the surgery. 4. Ovarian cancer is the sixth most common form of cancer in females. a. It is difficult to detect before it metastasizes beyond the ovaries. b. Risk factors include age (usually over age 50); race (white are at greatest risk); family history of ovarian cancer; never having children or first pregnancy after age 30; high-fat, low-fiber, vitamin A-deficient diet; and prolonged exposure to asbestos or talc. c. Early ovarian cancer has no symptoms or only mild ones associated with other common problems. d. Later-stage signs and symptoms include an enlarged abdomen, abdominal and/or pelvic pain, persistent gastrointestinal disturbances, urinary complications, menstrual irregularities, and heavy menstrual bleeding. 5. Cervical cancer starts with cervical dysplasia and can be diagnosed in its earliest stages with a Pap smear. a. There is some evidence linking cervical cancer to the virus that produces genital warts (papilloma virus). b. Other risk factors are increased incidence associated with an increased number of sexual partners, young age at first intercourse, and cigarette smoking. 6. Vulvovaginal candidiasis is the most common form of vaginitis and is caused by the yeast like fungus Candida albicans. a. Candidiasis is characterized by severe itching; a thick, yellow, cheesy discharge; a yeasty odor; and pain. b. The disorder, experienced at least once by about 75% of females, is usually a result of proliferation of the fungus following antibiotic therapy for another condition 7. Sexually transmitted diseases (STDs) are disease spread by sexual contact and include chlamydia, gonorrhea, syphilis, and genital herpes. a. Chlaymdia is a STD caused by the bacterium Chlamydia trachomatis. At present chlamydia is the most prevalent and one of the most damaging of the STDs. 1. In most cases, the initial infection is asymptomatic and difficult to recognize clinically. 2. In males, urethritis is the principal result. 3. In females, urethritis may spread through the reproductive tract and develop into inflammation of the uterine tubes, which increases the risk of ectopic pregnancy and sterility. b. Gonorrhea (“clap”) is an infectious STD that affects primarily the mucous membrane of the urogenital tract, the rectum, and occasionally the eyes. The disease is caused by the bacterium Neisseria gonorrhoreae. 1. Males usually suffer inflammation of the urethra with pus and painful urination. 2. In females, infection may occur in the urethra, vagina, and cervix, and their may be a discharge of pus. However, infected females often harbor the disease without any symptoms until it has progressed to a more advanced stage. If the uterine tubes become involved, pelvic inflammation may follow, often causing sterility and occasionally causing peritonitis. 3. If the bacteria are transmitted to the eyes of a newborn in the birth canal, blindness can result. Administration of a 1% silver nitrate solution or penicillin or erythromycin in the neonate’s eyes prevents infection. c. Syphilis is an STD caused by the bacterium Treponema pallidum. 1. It is acquired through sexual contact, exchange of blood, or transmitted through the placenta to a fetus. 2. The disease progresses through several stages: primary, secondary, latent, and tertiary. 3. During the primary stage, the chief symptom is a painless open sore, called a chanker. 4. A skin rash, fever, and aches in the joints usher in the secondary stage: a systemic infection. 5. The tertiary stage occurs when signs of organ degeneration appear. d. Genital herpes is an incurable STD caused by the type II herpes simplex virus (HSV-2). 1. HSV-2 causes genital infections such as painful blisters on the prepuce, glans penis, and penile shaft in males and on the vulva or sometimes high up in the vagina in females. 2. The blisters disappear and reappear in most patients, but the virus itself remains in the body. X. MEDICAL TERMINOLOGY - Alert students to the medical terminology associated with the reproductive systems.