Reproductive organs, gametogenesis, fertilization (for email)
advertisement
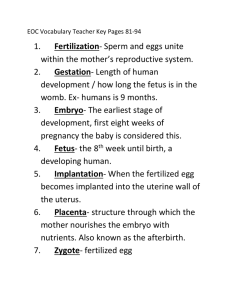
Sexual Organs, Gametogenesis and Fertilization Lecture 1 Cellular Division: Mitosis Cellular Division: Mitosis • Interphase – active stage of cellular function • DNA replication occurs here • Prophase • Centrosomes replicate and migrate to opposite poles, forms spindle fibers and asters to join with the chromatids • Nuclear envelope disintegrates • Chromatin chromosome chromatids • Metaphase • Starts when sister chromatids start to migrate and ends when the chromosomes are lined up at the metaphase plate. Cell Division: Mitosis • Anaphase • Starts when sister chromatids splits into independent chromosomes • Ends when chromosomes just prior to reaching the centrosomes • Telophase • When chromosomes are at each pole and nuclear envelope begins to form • Appearance of cleavage furrow and cytokinesis begins 1st Meiotic Division • Prophase I • Leptotene stage: Chromosomes divide into identical chromatids • Zygotene stage: Sister chromosomes (1 chromosome has 2 chromatids each) join together through synapsis. • Pachytene stage: sister chromosomes (bivalent pairs) thicken thru coiling • Diplotene stage: portions of bivalent chromosomes overlap one another thru chiasmata, called crossing-over, and separating of the sister chromosomes at the synaptinemal complex. • Diakinesis stage: moving of chiasmata to the terminal ends of the chromosomes called terminalization. 1st Meiotic Division • Metaphase I • Tetrads line up along the metaphase plate • Anaphase I • Paired chromatids (1 chromosome) move to opposite poles • Chiasmata separate • Telophase I • Nuclear membranes form • Cleavage furrow 2nd Meiotic Division • Similar to mitosis, but without DNA replication • Chromatids separate into each daughter cell Trisomy 21 Trisomy 21 Reproductive Organs Spermatogenesis Histology Spermatogonium Primary spermatocyte (1) Secondary spermatocytes (2) Spermatids (4) Spermatozoa Meiotic Events Chromosomal Complement DNA replication complete 2N, 4C First meiotic division in progress Second meiotic division 2N, 4C 1N, 2C Immature haploid 1N, 1C gametes Release of residual bodies 1N, 1C Supportive cells • Sertoli Cells • Target cells for FSH • Synthesizes androgen-binding proteins to maintain a high level of testosterone in the seminiferous tubules • Blood testis barrier • Degrading residual bodies for recycling • Interstitial cells/Leydig cells • Produce testosterone • Spermatogenesis in humans = 64-74 days Passage of sperm • Seminiferous tubules tubuli recti rete testis efferent ductules (ductuli efferentes) epididymis ductus or vas deferens ejaculatory duct urethra • Epididymis = area of storage and further maturation of sperm cells • Seminal vesicles: produce fructose and seminal fluid • Prostate: alkaline secretions of seminal fluid • Bulbourethral glands or Cowper’s gland: alkaline fluid and lubrication • Glands of Littre: mucus for lubrication Semen analysis Semen Normal Values Volume 1.5-5.5mL (Ave. 2.5mL) Sperm concentration 20,000,000/mL or more Motility >50% Forward progression 2 (scale of 1-4) Morphology >30% WHO normal forms Liquefaction Within 20-60min (30min) Collection time 2-3 days of abstinence Oogenesis Age Histology Meiotic Event Oogonium Chromosomal complement Fetal period No follicle Fetus Primordial follicle Primary oocyte 2N, 4C After birth Primary follicle 2N, 4C Puberty Secondary follicle Primary oocyte 2N, 4C Tertiary follicle Secondary oocyte + polar body 1N, 2C Ovulated ovum Secondary oocyte (arrested in metaphase II) 1N, 2C Fertilized ovum Ovum + polar body 1N, 1C + sperm Primary oocyte, arrested in prophase I (diplotene stage) 2N, 2C Oogenesis • First Phase • Primary follicle surrounded by squamous follicular cells • Follicular cells form several layers of cuboidal cells which are now called granulosa cells with a membrane between the oocyte called the zona pellucida Primary follicle Oogenesis • Second Phase • Growth of oocyte and surrounding granulosa cells • Formation of theca folliculi (interna and externa) outside the granulosa cells, with a basement membrane separating the two cell types. • Progresses to secondary follicle with formation of antrum • Theca cells develop LH receptors and produce testosterone, and the granulosa cells convert testosterone to estrogen via aromatase enzyme Secondary follicle Oogenesis • Third Phase • Further growth of follicle and selection of the dominant follicle • Dominant follicle is stimulated by FSH to mature to the Graafian follicle • The egg cell covered by granulosa cells now become the cumulus oophorus cells • The single layer of granulosa cells that is immediately surrounding the secondary oocyte is the corona radiata = produces hormones and makes the egg cell larger to facilitate transport along the fallopian tube • Egg cell is at metaphase II stage Ovulation • Egg cell ruptures from ovary • Stigma = area where Graafian follicle meets wall of ovary until it ruptures to the fallopian tube. • Formation of corpus luteum • Granulosa and theca cells • Secretes both estrogen and progesterone to prepare zygote for implantation in the uterus • If fertilization occurs, the embryo secretes beta-HCG to maintain the corpus luteum of pregnancy • If no fertilization occurs, the corpus luteum degenerates and becomes the corpus albicans Sexual or estrous cycle • 4 phases • 1. Period of preparedness: • only a short time for reproduction, ovulation and increased sexual desire • 2. Period of regression • Postestrum or metestrum • 3. Period of rest • Diestrum • 4. Period of active preparation • Proestrum Sexual or estrous cycle • Monoestrous – one breeding season a year • Polyestrous – multiple breeding seasons in a year • Anestrous – period of dormancy between estrous cycles Hormonal Regulation • Hypothalamus = GnRH • Pituitary = FSH and LH • Gonadal axis • Male • Female Fertilization 1. 2. 3. 4. 5. 6. Initial membrane contact between egg and sperm Entry of sperm Prevention of polyspermy Metabolic activation of egg Completion of meiosis by the egg Fusion of male and female pronuclei Fertilization • Site of insemination = upper 1/3 of fallopian tube • Barriers to insemination: acidity of vaginal canal, cervix and isthmus of fallopian tube • Contractions of vagina and uterus to propel sperm to the fallopian tubes • Cilia in the fallopian tube propel the egg cell towards the uterus, and the sperm are guided by swimming against a current (egg cell also contains sperm attracting properties) • Capacitation = process of making sperm cell able to fertilize egg cells Fertilization • Sperm enters egg cell through enzymes in the acrosome cap • Hyaluronidase = penetration through corona radiata • Acrosin = penetration through zona pellucida • Prevention of Polyspermy • Fast block = electrical barrier • Depolarization of egg’s plasma membrane by Na+ influx • Slow block = water barrier • Cortical granules fuse with plasma membrane to create a vitelline membrane (filled with water and hyaline) • Produce substances which kills other sperm attached Viability of gametes • Egg cell = 24 hours • Sperm cells = 1-2 days able to fertilize (3-5 days motile) Contraceptive Methods • Natural • Calendar method • Billing’s method • Withdrawal • Artificial • Hormonal • Barrier methods + spermicides • Surgical procedures