Is Methylene Blue Safe In Patients With Methemoglobinemia And
advertisement

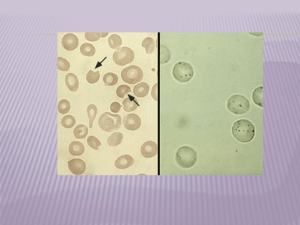
Is Methylene Blue Safe In Patients With Methemoglobinemia And Glucose 6-phosphate Dehydrogenase (G6PD) Deficiency? Bob Hoffman New York City Poison Center, NY, USA Overview • • • • Review of G6PD deficiency Review of methemoglobinemia (very brief) Review of methylene blue (MB) (brief) Attempt to answer the question – Expert opinion – Case reports – In Vitro data Introduction • G6PD deficiency – one of the most common inherited disorders, 400 million people affected – Largely in tropical and subtropical countries • Selection advantages – Against Plasmodium falciparum infection • Most affected individuals asymptomatic, but the risk of acute hemolysis is well known Frequency of G6PD deficiency Genetics • > 400 variants described • Different electrophoretic mobility, kinetic properties. • 5 classes according to the residual enzyme activity based (WHO). • Mediterranean and African (A-) variants – The most clinically significant. • Activity scarcely detectable in the Mediterranean type but close to normal in the African variant. Inheritance of G6PD Deficiency What Do We Need G6PD For? • Phosphogluconate pathway • Pentose phosphate pathway • Hexose monophosphate pathway • Hexose monosphosphate shunt G6PD Catalyzes the first step in the pentose phosphate pathway Regulatory enzyme The enzyme is highly specific for NADP+; the Km for NAD+ is 1000 greater than for NADP+. Pentose Phosphate Yields • Ribulose (ribose) 5-phosphate – Essential nucleotide in biosynthesis leading to: • DNA • RNA • Various cofactors –CoA, FAD, SAM, NAD+/NADP+ Glutathione reductase uses NADPH as a cofactor to reduce GSSG back to two moles of GSH. G6PD Deficiency • G6PD deficiency is not the absence of G6PD, it is a decreased activity – Many cells express G6PD – Red cells are the only important cell line because they lack a nucleus – Activity of G6PD highest (normal) in young erythrocytes and decreases with aging – Oxidants preferentially destroy senescent red blood cells Response to Oxidants Oxidant Response • If not reduced: – Some produce hemolysis • Oxidation of the hemoglobin chain – Some produce MetHb • Oxidation of iron – Some produce both? Physiology • Direct reduction of the oxidant Oxidant Glutathione Sulfhydryls Ascorbate Catalase Reduced Oxidant RBCs with Heinz Bodies • Precipitation of hemoglobin due to disulfide bond formation between Hb molecues • Upper photo shows distorted RBCs with large Heinz bodies • Bottom photo shows RBC stained with methylene blue Methemoglobin Definition • Oxidation of the iron molecule in hemoglobin from its normal Fe2+ to Fe3+ N N Fe histidine N N O H Methemoglobin H O2- Oxyhemoglobin C O COHb Physiology The oxidant is reduced by Hb (forming MetHb) • Then MetHb is reduced back to Hb MetHb NADH MetHb reductase (67%) Ascorbate (15%) Reduced Hb Glutathione (12%) NADPH Met Hb reductase (5%) Can You Use Methylene Blue In Patients with G6PD Deficiency? Famous Textbook Quotes • Methylene blue remains the first line therapy even in patients with known G6PD deficiency – Brent • Should never be administered to someone with known G6PD deficiency – Shannon • Should be used cautiously in patients with G6PD deficiency – Dart • • • • • • • • 28 year old man Ingested 60-120mL of 18% aniline MetHb 11 gm/dL (70-80%) 75 mg methylene blue given Didn’t get better G6PD screening showed deficiency (A-) Given ascorbate Hemolyzed, Hb fell, recovered – Rosen PJ: Failure of methylene blue treatment in toxic methemoglobinemia. Association with glucose-6-phosphate dehydrogenase deficiency. Ann Intern Med 1971;75:83-6 What happened between the 0 and 4 hour levels? • • • • • 26 month, 9.8-kg boy with G6PD deficiency Ingested 90 mL of nitroethane – MetHb 23.3% MetHb rises to 37%, then over 40% Cyanotic, in respiratory failure, intubated Two doses of methylene blue (2mg/kg) given “without response” • No hemolysis • Finally treated with exchange transfusion – Golden PJ: Treatment of high-risk, refractory acquired methemoglobinemia with automated red blood cell exchange. J Clin Apher 1998;13:28-31. • 74 G6PD deficient men • 3 day regimen – Chloroquine 1500 mg – Methylene blue 780 mg (mg/kg PO BID) • No hemolysis occurred – Mandi G: Safety of the combination of chloroquine and methylene blue in healthy adult men with G6PD deficiency from rural Burkina Faso. Trop Med Int Health. 2005;10:32-8. • 3 case reports • Intraamniotic methylene blue given for PROM (2); IV for maternal MetHb (1) – Dose varied • All developed elevated bilirubin • Only 2 G6PD deficient – Gauthier TW: Methylene blue-induced hyperbilirubinemia in neonatal glucose-6-phosphate dehydrogenase (G6PD) deficiency. J Matern Fetal Med. 2000;9:252-4. • • • • • • • Neonate, known G6PD deficiency Multiple cardiac abnormalities Undergoes surgical repair on day 28 of life Requires nitroglycerin IV Develops MetHb: 75% Given low dose (0.1 mg/kg) methylene blue Has mild hemolysis requiring no therapy – Middali MM: Postoperative methemoglobinemia with associated G-6-P-D deficiency in infant cardiac surgery--enigmas in diagnosis and management. Paediatr Anaesth 2005;15:334-7. • 59-year-old man with metastatic renal cell CA • Trial of 3-aminopyridine-2-carboxaldehyde thiosemicarbazone (3-AP; Triapine) • Developed MetHb 35% • Given 3 doses (1 mg/kg) methylene blue • MetHb fell to 10%, then 6.5 % • Masive hemolysis • Severe G6PD deficiency confirmed later – Foltz LM: Recognition and management of methemoglobinemia and hemolysis in a G6PDdeficient patient on experimental anticancer drug Triapine. Am J Hematol 2006;81:210-1. • • • • • • • • • Metoclopramide 10 mg administered twice Cyanosis and dyspnea; 28 hours later MetHb was 43% Ascorbic acid 150 mg and methylene blue 60 mg given Consciousness deteriorated Methylene blue 40 mg was repeated at 2 hours Deteriorated rapidly and he died 12 hours Blood taken a before death was hemolysed Postmortem: b5R and severely G6PD deficient – Karadsheh NS: Metoclopramide-induced methemoglobinemia in a patient with co-existing deficiency of glucose-6-phosphate dehydrogenase and NADH-cytochrome b5 reductase: failure of methylene blue treatment Haematologica 2001;86:659 • 25 year old man; large dermal exposure to aniline • 5 hours later – MetHb 51% • Methylene blue 40mg IV improved symptoms • MetHb fell to 2.1% • Developed significant hemolysis • G6PD deficient • Recovered (transfused) – Liao YP: Hemolytic anemia after methylene blue therapy for aniline-induced methemoglobinemia. Vet Hum Toxicol. 2002;44:19-21. In Vivo Summary • Does Methylene blue fail? – Often works – Usually slowly • Does methylene blue cause hemolysis – It can, and it can be severe – Especially when hemolysis is present prior to therapy Beutler E: Methemoglobin Reduction: Studies of the interaction between cell popluations and of the role of methylene blue. Blood 1963;22:323-333 • Incubated human RBCs with nitrite to induce MetHb • Treated with methylene blue and glucose • Observed rates of fall – Normal cells – G6PD cells (A-) – Mixture of cells Implications • G6PD deficient cells clear MetHb slowly in response to methylene blue • Either NADPH or leukomethylene blue can move from healthy cells to deficient cells • This effect is more pronounced at lower levels of MetHb – Young cells and reticulocytes are G6PD present – Role of transfusion (fresh blood)? Summary (1) • Data on the use of methylene blue in patients with G6PD deficiency are limited – Most support some degree of efficacy – Significant risk of hemolysis • Would administer methylene blue in: – Patients with no history of G6PD deficiency – Patients with known G6PD deficiency and lifethreatening MetHb • Ascorbate, Exchange transfusion, HBO, NAC Summary (2) • Withhold methylene blue in: – Patients with known severe variant G6PD deficiency (Mediterranean) not significantly ill – Patients with known or suspected G6PD deficiency and marginal indications for treatment – Patients with significant active hemolysis in addition to MetHb Summary (3) • If giving methylene blue to patients with a known or suspected history of G6PD deficiency – Keep the first dose small (1 mg/kg) – Recheck the MetHb often – Do not repeat if unsuccessful – Observe closely for hemoylsis