Slides - Safe Surgery 2015
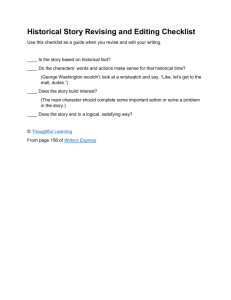
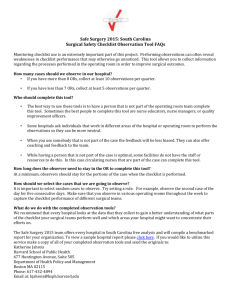
advertisement

Call 2: Evidence Supporting the Use of the Checklist and The Importance of the Checklist Implementation Team Topics Covered on the Last Webinar • Checklist Development and Background. • Why South Carolina? • The impact of the Safe Surgery 2015: South Carolina on surgical safety globally. • Going beyond the “Time Out”. Meet the Team Lorri Gibbons, RN, BSN, CPHQ VP, Quality & Patient Safety SCHA Poll 1 • Are you using a surgical checklist that requires the surgical team to stop and discuss critical items at three points of time (Before Induction of Anesthesia, Before Skin Incision, and Before the Patient Leaves the Room)? – Yes – No • If you answered yes, what percentage of surgical cases are using this type of checklist routinely? – <50% – >50% – It is used for every patient undergoing surgery Today’s Topics • A full review of articles that have been written about the impact of the checklist. • The importance of data to physicians and how to talk to physician’s about data. • Building a Checklist Implementation Team: – Poll – The role that this team plays – Who should be on the team – How often the team should meet – How to find the “right” people to lead this work A Full Review of Evidence Haynes et al. A Surgical Safety Checklist to Reduce Morbidity and Mortality in a Global Population. New England Journal of Medicine. 2009 Jan 29; 360(5):491-9. International Pilot Study 8 Evaluation Sites - Nearly 8,000 Patients PAHO I Toronto, Canada EURO EMRO London, UK Amman, Jordan WPRO I Manila, Philippines PAHO II Seattle, USA WPRO II AFRO Ifakara, Tanzania SEARO New Delhi, India Auckland, NZ Results – All Sites Baseline Checklist P value Cases 3733 3955 - Death 1.5% 0.8% 0.003 Any Complication 11.0% 7.0% <0.001 SSI 6.2% 3.4% <0.001 Unplanned Reoperation 2.4% 1.8% 0.047 Survey of Attitudes to Checklist Use Among Clinicians at Study Site (n=229) The checklist was easy to use 78.6% The checklist improved operating room safety 79.0% The checklist took a long time to complete 18.3% Communication was improved through use of the checklist The checklist helped prevent errors in the operating room If I were having an operation, I would want the checklist to be used 84.3% 78.2% 92.6% Haynes, A et al. Changes in safety attitude and relationship to decreased postoperative morbidity and mortality following implementation of a checklist- Based surgical safety intervention. BMJ Qual Saf 2011;20:102-107 Additional Evidence de Vries EN, et al. Effect of a Comprehensive Surgical Safety System on Patient Outcomes. N Engl J Med 2010; 363:1928-1937 SURPASS Checklist The Netherlands • 100 item checklist implemented in 6 high performing hospitals • Compared to controls the test hospitals had a greater than one-third reduction in complications and achieved an almost 50% reduction in deaths (from 1.5% to 0.8%) (N=7,580) de Vries EN, et al. Effect of a Comprehensive Surgical Safety System on Patient Outcomes. N Engl J Med 2010; 363:1928-1937 Neily J, Mills PD, et al. Association Between Implementation of a Medical Team Training Program. JAMA. 2010 Oct 20;304(15):1693-700 Veterans Health Affairs • Implemented a surgical team training program incorporating a modified version of a surgical checklist in the operating theatres of 74 facilities • Experienced initial mortality reduction of 18%1 • One year later, facilities that participated in the program experienced a risk-adjusted morbidity reduction of 17% versus 6%2 1. Neily J, Mills PD, et al. Association Between Implementation of a Medical Team Training Program. JAMA. 2010 Oct 20;304(15):1693-700. 2. Young,Xu Y, et al. Association Between Implementation of a Medical Team Training Program and Surgical Mortality. Arch Surgery. 2011. Dec; 146(12):1368-73. van Klei WA et al. Effects of the Introduction of the WHO “Surgical Safety Checklist” on In-Hospital Mortality. Annals of Surgery. 2012 Jan 1; 255(1):44-9. University Medical Center Utrecht, The Netherlands • 25,513 adult patients undergoing non-day surgery. • Used hospital administrative data and patient medical records. • Crude mortality decreased from 3.13% to 2.85%. • Measured checklist compliance and found that mortality was significantly lower in patients with completed checklists. van Klei WA et al. Effects of the Introduction of the WHO “Surgical Safety Checklist” on In-Hospital Mortality. Annals of Surgery. 2012 Jan 1; 255(1):44-9. Takala, R.S.K. et al. A pilot study of the implementation of WHO Surgical Checklist in Finland: improvements in activities and communication. Acta Anaesthesiol Scand. 2011. Sep 26 (55): 1206-1214. Finland Study Four Teaching Hospitals • Implemented a modified version of the WHO Checklist • Studied the impact on communication and processes by surveying surgical teams pre and post implementation Discussion of Critical Events Pre Operatively Pre Implementation P < 0.001 Post Implementation Anesthesiologist Surgeon Anesthesiologist Surgeon 22% 35% 43% 46% N=1,748 Takala, R.S.K. et al. A pilot study of the implementation of WHO Surgical Checklist in Finland: improvements in activities and communication. Acta Anaesthesiol Scand. 2011. Sep 26 (55): 1206-1214. Bliss LA, et al. Thirty-Day Outcomes Support Implementation of a Surgical Safety Checklist. J Am Coll Surg. 2012 Aug 27. 600-Bed Tertiary Care Facility in the Northeast US • Three 60 minute team training sessions • Use of checklist in high-risk general surgery cases (73 cases) • Checklist completion rate >90% • Checklist use was correlated with decrease in all measured areas of 30-day morbidity Bliss, LA et al. Thirty-Day Outcomes Support Implementation of a Surgical Safety Checklist. J Am Coll Surg. Available online August 30, 2012. Stanford University, United States • O/E Mortality declined from .88 to .8 • The total number of reported events rose; however, those that were attributed to errors/complications decreased from 35.2% to 24.3% • Mean OR start to incision time was shorter • There was improvement in the belief (SAQ) that all personnel take responsibility for patient safety (N=12,247) Tsai, Thomas et al. Does a surgical safety checklist improve patient safety culture and outcomes? [Abstract]. In: American College of Surgeons Annual Clinical Congress. 2010 October 3-7; Washington D.C. Journal of American College of Surgeons. Truran et al. Does using the WHO surgical checklist improve compliance to venous thromboembolism prophylaxis guidelines? The Surgeon 9 ( 2 0 1 1 ) 3 0 9e3 1 1 Semel, ME et al. Adopting a surgical safety checklist could save money and improve the quality of care in U.S. hospitals. Health Aff (Millwood). 2010 Sept; 29 (9);1593-9 Shauna L. et al. Implementing a surgical checklist: More than checking a box. Surgery, 2012 Sep; 152. 331-6. What Does the Evidence Mean to Physicians? There Will Never Be The Perfect Study Evidence “Driven” Behavior Believing Physician Engagement Observed During a Surgical Checklist Implementation Building an Implementation Team Poll 2 • Are you listening to the call as a group or an individual? – Group – Individual Make an Implementation Team • Administrator/Quality Improvement Officer • Anesthesiologists and/or CRNA • Circulating Nurse • Scrub Tech • Surgeon • Others (Perfusionists, PA’s, Biomedical Engineers, Anesthesia Techs, Pre-op nursing, etc) Find Clinical Champions • The nurses will know. • Pick those who are respected and who will be supportive. • The support of “formal” leadership is absolutely necessary but those leaders are often not the ones who should guide this effort directly. Recommendations on How Often and When to Meet as A Team • Meet regularly. • Choose someone to organize the meeting schedule and be a point of contact for people in your hospital and our team. • A good time to meet together would be following each webinar. • It is better to meet with part of the group than not at all. • Your physician champions don’t have to be part of every meeting. What Should You Tell Checklist Implementation Team Members This team will be responsible for the following tasks: – Administering the culture survey – Modifying and customizing the checklist – Guiding small scale testing of the checklist – Devising the implementation plan – Educating and training clinicians to use the checklist – Coaching teams on continued use of the checklist – Regularly report progress to hospital administration Homework • Think about who you are going to have on your checklist implementation team. • Please contact Katie Jahreis to administer the culture survey kjahreis@hsph.harvard.edu. Questions Next Webinar: November 29th, 2012 2:00-3:00 • An in depth discussion of why each item is on the South Carolina Checklist Template. • Overview of what is to come in Part II and upcoming events. Office Hours: Wednesday 2:00-3:00 We Will Be Sending You An Email With: • A comprehensive bibliography of all of the evidence that has been published on the checklist. • An article that is a literature review of how the checklist has been shown to improve teamwork and communication in the OR. • A link to watch the recording of today’s webinar and to download today’s slides. Resources Website: www.safesurgery2015.org Email: safesurgery2015@hsph.harvard.edu