Developmental Problems of the Preschool Child
advertisement

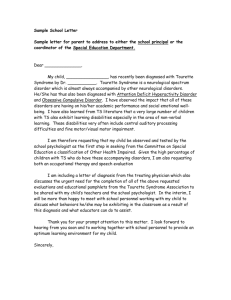
Developmental & Disruptive Disorders of Childhood and Adolescence January 18, 2012 Will Beyer, LSPE-HSP, LPC-MHSP The ADHD/LD Clinic of Tennessee 731-660-2850 willbeyerlpe@gmail.com There is nothing new under the sun. (Solomon- Book of Ecclesiasties) “You will never accomplish greatness without loving what you do. Steve Jobs- CEOApple Computers. “Stay Hungry, Stay Foolish” Where is happiness not found? Alcohol or drugs Sex, food, or money Education or knowledge Power or position Any “Thing” In the past or in the future In “Control” Where do we find happiness? Healthy Relationships Special Moments Practicing Forgiveness Regularly engaging in acts of kindness In Healthy Living In our Spiritual Lives The Words and Wisdom of Forrest Gump “I may not be a smart man, but I know what love is.” “Sometimes there just aren’t enough rocks.” “I could run like the wind blows!” “I gave Bubba’s mother his share. I had to keep my promise.” “You can sit here.” Jenny “I love to beat up on Notre Dame!” (I don’t recall where this is in the movie, but I’m kinda sure it is in there somewhere.) Keymakers Some people see a closed door and turn away. Some people see a closed door, try the knob and if the door doesn’t open, turn away. Some people see a closed door, try the knob, and if the door doesn’t open, they find a key, and if the key doesn’t fit they turn away. A rare few see a closed door, try the knob and if it doesn’t open, find a key, and if the key doesn’t fit… they make one! What Have I Learned About Kids? All children need and desire love and approval. “Tell them you care and want to help. Be real, and don’t fake it.” Most children with anger problems have been deeply hurt and are grieving. “Acknowledge their losses and comfort them.” Children with anger problems have difficulty seeing a future. They often feel helpless and hopeless. “Give them hope and help them regain a vision for the future.” Human behavior is complicated. Do not oversimplify behavior. “Think like a scientist, use methodology, study hard and ask lots of questions.” All children need safety in times of “storm and stress”. “Provide a safe haven.” Programs do not change people-Relationships do! Self-control begins with self-talk. “When what they say to you and what they say to themselves is the same, trust has been established.” If we punish or scare children into compliance, we increase the need for supervision and decrease their self-control and individual initiative. 8 What I have learned about kids, cont., Treat the child with fairness, consistency and respect while clearly communicating expected behavior, reasonable consequences and reward for success. Take them from where they are, not where they should be. Parent’s generally love their children, but they may not understand why their child is having problems, nor how to help. Therefore, treat the parent with respect and seek to form a collaborative relationship. Children themselves may not understand why they are are struggling with self-control. Tantrums represent a signal of helplessness and a test to assert one’s own independence. Violence demands that people listen. It empowers the person. 9 Sequence of Topics for this Program Brain Development and etiological factors Observing and interviewing for developmental problems/Biological mechanisms in psychopathology ADHD Oppositional Defiant Disorder The Angry/Aggressive Child Effects of Divorce Abuse/ Maltreatment/Trauma/R.A.D. Mental Retardation/Developmental Delay Learning Disabilities Tic Disorders/Tourette’s/Impulse Control Disorders Autism/Pervasive Developmental Disorders Fear and Anxiety/PTSD Childhood Depression Neurogenetic Disorders DSM-IV Disorders of Infancy, Childhood or Adolescent Mental Retardation Learning Disorders (Reading, Math, Written Language Motor Skills Disorders, Development al coordination Communicati on Disorders (expressive languagemixed recepexpres, phonological disorders) Pervasive Development al Disorders (Autistic, Rett’s Asperger’s) ADHD and Disruptive Behavior Disorders (ODD, C.D.) Feeding and Eating Disorders (Pica, etc.) Tic Disorders (Tourette’s, Chronic vocal or Motor Tic, Transient Tic) Elimination Disorders (Encopresis, Enuresis Other: Selective Mutism, RAD, etc. DSM-V Revisions • • • • • • • • • • • • • Intellectual Developmental Disorder/ IDD or Global Developmental Delay-NOS (not M.R.) Bi-Polar Disorder- More stringent criteria for children Gender Dysphoria (Moved out of sexual disorders) Hypersexual Disorder Oppositional Defiant Disorder- (Angry/Irritable Mood/Headstrong Behavior, and Vindictiveness) Behavioral Addictions-gambling New Suicidal Scales to determine risk. Temper dysregulation with Dysphoria (TDD) Communication Disorders (Language, Speech, Social Communication) Autism Spectrum Disorder (inclusive of PDD & Aspergers) Deleting specific categories of Schizophrenia Attention Deficit Hyperactivity Disorder-Age change and number of criteria required. Specific Learning Disability Case Study 13 year old female, African-American/Professional parents recently relocated/private school. Not paying attention in class/ Acted like she had a hearing problem. Previously diagnosed ADD and prescribed meds. Not much help. Headaches, impaired appetite/obese, Ringing in ears Flattened affect- looked depressed/spacing out Speech and language had diminished/slow talking. Expressive language was impaired. Slow writing and weak motor movement. *Not athletic/poor balance. Case Study… Cont., Elevated scores on ADHD checklist consistent with ADD I.T. Clinically significant scores on Child Depression Inventory Underachieving in school. Complained of body aches/Didn’t feel good. Daydreamed/lost in her own thoughts/slept excessively/Schizoid features/Poor Socialization WISC-IV: VCI = 78, PRI =84, WMI = 72, PSI = 68 WIAT-III- Reading Comp- 78 Adaptive: 88 Emotionality: P-MACI= Elevated -Somatization, ADD, GAD. OCD Differential Diagnosis? ADHD-Inattentive Type Borderline Intellectual functioning Learning Disability/Language Disorder Adjustment Disorder Dysthymia or Mood Disorder Selective Mutism Early somatization symptoms Early onset schizophrenia or psychosis Then I noticed…. A few café au lait splotches on her legs and arms. Small subcutaneous bumps starting under her skin, swollen joints. I remembered Tinnitis symptoms, headache, balance problems, flattened affect in face (paralysis). Hypotonicity in arm and leg strength *Then I had a “House” moment… what if she has….? NF-1 Neurofibromatosis-Type 1 Long arm q of chromosome 17 Encodes for the protein (neurofibromin) which is a tumor suppressor (usually benign). Subcutaneous tumors begin to grow and café au lait clusters with neurological symptoms emerging. (headache, lethargy, depression, attention deficits, facial paralysis, learning disabilities, etc.) NF-2 is chromosome 22q- Case Study: Timmy Tornado Development: Born 10 weeks premature, mother used methamphetamine in utero and heavy smoker. Emergency C-Section/fetal distress Age 9: Hasn’t spoken, Makes sounds, extremely hyperactive, PICA, Lives in old house, self-injuriousbites, hits, head butts, younger sibling in the home. Timmy Cont., 2-3 simple gestures Meds: Seroquel, Trileptal, Ambien, Risperdal, Melatonin, (Has been on Haldol, Ritalin, Neurontin, and Depakote in the past) *Only seen Physician Assistant. *Severe PICA: Feces, balloons, pins, glass, buttons, teeth, toys, insects, rocks, etc. etc. Impaired Social Interaction, Motor Movement, impaired communication, restricted or repetitive patterns of behavior. Discuss: Assessments and Treatment Plan 1. Initial diagnostic Impression? 2. What assessments may prove useful? 3. Where do you start? 4. To whom do you refer and why? 5. *Complication: Indigent family/TN Care only. To get it right we may need.. • • • • • • • • • • Direct Observations Rating Scales Hearing, Vision, Speech and Language Play Based Assessments Functional Assessments Occupational Therapy Physical Therapy Intellect and Achievement Developmental Inventories Adaptive Behavior Brain Development • • • • • • Begins in week three with neuroectoderm and forms the neural plate Cell Proliferation-Neural plate-neural tube-brain and spinal cord Cell Migration-neurons move to specific regions to their final positions Cell Differentiation- segmenting Cell Death (apoptosis) (Pruning) (Stress, nutrition, drugs, chemical contaminants, hypoxia, gene expression, etc.) Neurodevelopmental Disorders-Etiology • Deprivation • Genetic • Immune Dysfunction • Infectious Disease • Metabolic Disorders • Nutrition • Trauma • Toxic and Environmental Factors Common Neurotoxins to the Fetal Brain Affect the transmission of chemical signals between the neurons: Lead, Mercury, Toluene, Dioxins, PCB’s, Arsenic, Alcohol There are both presynaptic and postsynaptic effects such as interfering with production of transmitters, to conduction of action potentials, transmitter storage, transporter molecules and transmitter metabolism Biological Mechanisms involved in Psychopathology Severe Maltreatment-(3 million cases per year/one-third between ages 3 and 7.) Disease (CNS infections (cytomegalovirus, toxoplamosis, rubella, herpes simplex, HIV, HIB meningitis) Nutrition Accidental Injury Genetics: (ADHD, Fragile X, PKU, etc.) Exposure to Toxins: Lead, ETOH, cocaine, etc. In utero: Stroke, hemorrhage, anoxia, etc. Most Common Causes of Neurological Insult Prenatal (includes genetic), 80-85% Perinatal (most often asphyxia), 5-10% Postnatal- 5-10% Testing for hypothyroidism (1 in 4000) and Phenylketonuria (1 in 12,000) has reduced M.R. Most common chromosomal-Down’s-1 in 700, Fragile X, 1 in 800 males, Trisomy 18-1 in 4000. (Prader-Willi syndrome, Wilson’s Disease) Medical Assessments • Genetic Studies • Brain Image Studies ( MRI, FMRI, CT, EEG, SPECT, PET, etc.) • Metabolic Screens (blood and urine- for how the child metabolizes food. • Lead Chelation (Pica) Drugs that affect the fetus Tobacco Vaccines Vitamins Alcohol Narcotics Anti Cancer Agents Anti Seizure Antibiotics Sex hormones Barbituates Stimulants Designer Drugs Aspirin Anti Anti Coagulants Psychotics The Mental Health of the Child begins in Utero Low Birth Weight Precipitous Birth Exposure to Toxins/drugs Tobacco STD’s Poor Nutrition Absence of Prenatal Care The Relationship between AOD Use and Psychiatric Symptoms and Disorders AOD can mask psychiatric symptoms and disorders. AOD can worsen the symptoms of psychiatric disorders. AOD withdrawal can cause psychiatric symptoms and mimic psychiatric disorders. Psychiatric disorders and AOD disorders can co-exist. Psychiatric disorders can mimic behaviors associated with AOD abuse. AOD can cause psychiatric symptoms and mimic psychiatric disorders. 30 Environmental Factors Pre or postnatal Acute or Chronic Single or Additive or multiplicative Biochemical or Social (Parenting style, family interaction, peer interaction, education, culture, community) Prevention of Childhood Disorders Good prenatal care. Targeting low income teenage mothers linking to community services. Character Development in early years Protect against abuse and neglect. Targeting caregivers/Increase Training Opportunities. Environmental change. Enhance educational opportunity. Target 5th-7th grade males at risk for delinquency. Protect against accidental head injury or Neurological Insult Educating Parents About Risks Drowning- Pools, 5 Bicycle helmets/ car gallon buckets, bathtub, etc. Suffocation-dry cleaner bags, coins, toys, refrigerators, ropes, hanging, chemical, ageappropriate foods Burns- matches, gasoline, etc. seats Toxic chemicals Child Safety gates Bars on upstairs windows. Child resistant containers *Safety walkthrough/checklist Birth Psychology- What have we learned? The placenta doesn’t always protect the prenate. (Pollution-solvents, metals, radiation, pesticides) Ubiquitous exposure to adults-nicotine, caffeine, aspirin affect growth and development. Prenates are learning: voices, music, stories Brain growth spurt-Beginning of third trimester to age 2. R.H. maturation- once and for all opportunity. The effects of nutrients: folic acid, taurine, etc. The importance of attachment. Chromosomes Humans normally have 46 chromosomes in each cell, divided into 23 pairs. Each parent contributes 23. Changes in genomic imprinting disrupt the regulations of genes resulting in inaccurate copying from either the paternal or maternal copy. A missing piece of the chromosome is called a “deletion” (p) Is the short arm for petit. (q) Is the long arm (next letter in the alphabet) Behavioral Genetics 100,000 genes in human genome. Tens of thousands of genes contribute to neuroanatomical and neurophysiological substrates in the CNS. The expression of a gene depends on the genetic milieu in which it is placed and the interaction with the environment. Chromosome 11 Chromosome 11 contains 134 million DNA building blocks (base pairs) and represent 4 percent of the total DNA in cells. Chromosome 11 Disorders include: Beckwith-Widemann (p) short arm JacobsenSyndrome (q) long arm Neuroblastoma/Leukemias/lymphomas Ewing Sarcoma ( (t) fuses Chromosome 11 and 22) Genetically Determined Disorders of Cognition • Chromosome 11 q-syndrome • Down’s Syndrome- 1/1000 • Fragile X Syndrome- 1/1250 males • • • • and 1/ Kleinfelter Syndrome 1/1000 males Turner Syndrome-1/2500 females Prader-Willi Syndrome Phenylketonuria- 1/10,000 Classification of Neurogenetic Disorders • • • • • • Autosomal Recessive Disorders- (Ex. PKU, Tay-Sachs) Autosomal Dominant Disorders-(Ex. Huntingdon’s Disease) Sex-Linked Disorders (Ex. Fragile X, Turner’s Syndrome) Genetic Deletion Disorders- (Ex. Prader-Willi Syndrome, Monosomy 21) Multifactorial Chromosomal Abnormalities (Dyslexia, Schizophrenia, Parkinson’s, Tourette’s, Alzheimer’s, Depression) Extra Genetic Material DisordersKlinefelter’s Syndrome XXY, Jacob Syndrome XYY Developmental Delay D.D. is more appropriate when cognitive ability and adaptive behavior are significantly below average. Used when clear-cut data is not available to diagnose mental retardation. Parent or pediatrician may first raise concerns that the child “seems behind”. Motor skills, speech, language, cognition, social, emotional delays Human Behavior is defined as…Vt=Vg +Ve+Vg+Ve Phenotype: The observable physical or biochemical characteristics of an organism, as determined by both genetic and environmental influence. Genotype is the genetic makeup of a cell (the combnation of allele makeup of the individual) Vt, the total phenotype variance, equals Vg, the component of variance due to genetic factors plus Ve, the component of phenotypic variance due to environmental factors, plus a component of variance which reflects specific geneenvironmental interactions. Restriction Fragmentation Length Polymorphism (RFLP) DNA is cut by a restriction enzyme The DNA fragments are separated by electrophoresis The fragments are transferred to a membrane by the Southern blot procedure Hybridization of the membrane to a labeled DNA probe Each fragment is considered an allele 43 Genotyping is the process of elucidating the genotype of an individual with a biological assay. Restriction fragment length polymorphism (RFLP) Terminal restriction fragment length polymorphism (t-RFLP) Amplified fragment length polymorphism (AFLP) Multiplex ligation dependent probe amplification (MLPA) Chromosome 18q-Syndrome Deletion of long arm of (q) of chromosome. Symptoms: short stature, hypotonia, abnormalities of skull, face, deeply seated eyes, prominent ears, visual/hearing abnormalities, heart defects, malformations of hand and feet. Carp shaped mouth, *Lots of variability in severity of symptoms. Not always low functioning. Rett Syndrome Normal pre-perinatal development through first 5 months (boys), first 28 months (girls). Decelerated head growth from age 5 to 48 months (neurodegenerative disorder) MECP2 gene (Seizures, gastrointestinal problems, No verbal skills, Progressive loss of motor, then cognitive skills. *Hand movements, stereotypic hand movements such as hand wringing and poorly coordinated gait. Mental retardation. *Severe to Profound. Down’s Syndrome Down’s Syndrome-Trisomy 21. Increasing risk with maternal age. Mean IQ = 47-50. 10% are institutionalized. Physical characteristics-high cheek bones, microcephaly, large tongue, small round ears, hypertonic muscles. Prone to congenital heart defects, infections, and injury. Temperament is typically friendly and love music. Huntington’s Disease (Chorea) Chromosome 4 (CAG Repeat) Huntingtin gene (HTT) codes for protein Huntingtin Trinucleotide repeat (CAGCAGCAG) Cytosin-adenineguanine) Symptoms: Behavioral disturbance, hallucinations, irritability, restlessness, psychosis, facial movements, unsteady gait, anxiety, speech impairment, “prancing” walk, etc. (basal ganglia in striatum) 250,000 Americans have H.D. Symptoms can begin anytime but usually begin between 3544 years of age. *Search youtube (The Real Huntington’s Disease The Sequel) Dopamine blockers may slow progression, possible coenzyme Q10, Amantadine may help. Sydenham’s chorea Etiology: Infection with Group A betahemolytic streptococcus. (basal ganglia and corpus striatum) Occurs in 20-30% with acute rheumatic fever. (youtube: Syndenham’s chorea: Rebekah Everest May occur 6 months after infection. Symptoms: chorea, slowed cognition, facial grimacing, hypotonia, hand milking, (Not PANDAS) 50% recover in 6 months. What are the needs of the children I serve? Self-Control (Impulse, aggression, etc.) Mood Stability Cognitive (Reasoning, Problem Solving) Self-care skills (hygiene, cleanliness) Social skills: (Conflict Resolution) Academic: (Reading, Writing, Arithmetic) Motor skills: (fine & gross motor) Language/Communication skills Virtues and Character Development Intelligence Fluid-strong heritability, independent of education and experience. Matrices, figural relations, abstract, non-verbal. Crystallized-increases with experience and education. Verbal Comprehension, Arithmetic, Vocabulary, Knowledge of facts, Deductive Reasoning, Associative memory Substance Abuse in those with Intellectual Deficiency 2.6% with I.D. have S.A. (Slater, 2010) Start drinking a couple years later than peers. Less likely to be Caucasian. Less likely to seek help and less likely to receive it when sought. More likely to be prescribed medication. Greater risk of accidental overdose. More likely to have legal issues. More likely to have another co-morbid mental illness. Poor reading skills limit access to materials and programming. Functional Delay “A continuous, significant delay in intellectual functioning and achievement which adversely affects the students ability to function in the general school program, but adaptive behavior in the home or community is not significantly impaired. Significantly impaired intellectual functioning two or more standard deviations from the mean. B. Deficient academic achievement below the 4th percentile in two areas: basic reading, reading fluency, reading comprehension, math problem solving, math calculation, written expression. C. Home or school adaptive behavior above that for intellectual deficiency. A. Diagnosis of Mental Retardation Intelligence 70 or below (SEM = 3) Adaptive Behavior- In at least two areas: Communication, self-care, etc. Not a single disease, syndrome or symptom, but rather a state of cognitive impairment that is identified by the behavior of the individual. Not always readily identifiable. They can look, act, and talk normally. Diagnosis of M.R. cont. May be classified as M.R. at one time during their lives and not at another. Etiology is varied and complex. May include both genetic and environmental factors. IQ’s of 70 to 84 are considered borderline intelligence. Category of Mental Retardation Mild = 50-55 to 69 Moderate = 35-40 to 50-55 Severe = 20-25 to 35-40 Profound = below 20 Adaptive Deficits Self-care Leisure Communication Health Safety Academic Skills Self-direction Home living Social Interpersonal Tests: Vineland Use of Community Resources Adaptive Behavior Scales and Adaptive Behavior Evaluation Scales Social Skills The ability to communicate and interact with peers and adults in an appropriate manner. The ability to adapt to new environments. The ability to interact in groups and conform to expected social behaviors. Basic knowledge of facts and social judgment. The ability to solve conflicts. Teaching Strategies to promote skill acquisition Check frequently for understanding. Teach students to use self-talk. Use the skill in several different learning environments to promote generalization. Prompt to focus attention. Prompts-Natural, Visual, Verbal, Modeling, Physical Guidance Methods for teaching students with low cognitive functioning Break task down into small steps. Demonstrate/model Positive reinforcement of desired behavior Shaping-Operant Conditioning Community Based instruction Individualized instruction Self-contained classrooms/LRE Curriculum for Students with MR Basic academics- Accepting reading, math, writing. Math- counting, telling time, measurement. Reading- functional vocabulary Social Skills Life Skills Making choices, decisions responsibility Safety Issues Self-determination Legal issues Conflict Resolution Health issues Vocational Assessing Motor Skills Eye Tracking Balance in seat with Palm Rotation feet and arms extended Number Recognition (1,3,9) Skipping Touch finger with arm extended. Resistance Hand grip Finger to thumb Balance on one foot Heel to toe- Front and back. Draw a circle, line, square, triangle Coordination Disorder Delays in achieving motor milestones, e.g. walking, crawling, sitting) dropping things, clumsiness, poor performance in sports, handwriting, etc. Additional problems may include: cerebral palsy, hemiplegia, muscular dystrophy. To Improve Disorganization Reinforce organization Is the task too difficult? efforts. Use a peer model. Provide time for organization. Provide storage space Evaluate: Is the length of time to complete the task appropriate? Increase prompting and cueing. Demonstrate and rehearse procedure. Establish routine. Use color coded organizational system. Minimize needed materials. Autism/PDD Impairment in Communication- Receptive skills tend to be better than expressive.*Loudness, intonation, rhythm, stress. *Echolalia Social impairments- eye contact, facial expressions, gestures, (how skillful does the child relate to peers) Difficulty in imitation, affective expression. Stereotypic Motor Movements. Lower intellectual ability *Significant heterogeneity *Six symptoms across two categories, with at least two symptoms in the social category and one in the restrictive/repetitive behavior category. Interesting Facts about Autism 20-33% have seizures Elevated Serotonin Frequent levels (also in first degree relatives) Fragile X is present in 8% of individuals with autism. Higher rate in monozygotic than dizygotic twins complications in pregnancy Occurs more often with viral infections. Difficulty with autonomic arousal Asperger’s Syndrome *May be high functioning autism. Higher cognitive and language ability. Clear social impairments: Social awkwardness, motor clumsiness, idiosyncratic or engrossing interest. *Absence of deficits in intellect, adaptive, or language abilities. Communication Disorders Expressive Language Receptive Language Mixed Expressive-Receptive Language Phonological (articulation) Stuttering Dyslexia, Dysgraphia Sex Errors of the Body • • • • • Triple X Syndrome XXX- Increased M.R. Turner Syndrome: X (Short stature, missing ovaries or testicles, low IQ, Klinefelter Syndrome XXY- male, insuffient masculination, sterility, low sex drive, learning problems Androgen Insensitivity Syndrome- Male hermaphroditism, defective gene on x chromosome (Sex assignment is female) Remove testicles and female hormone replacement) Congenital adrenal hyperplasia- female hermaphrodistism- female internal organs, male external organs Gender Identity Disorder *(1) Strong and persistent crossgender identification, as manifested in a desire to be or belief that one is the opposite sex, preferences for stereotypical cross-gender clothing, etc. (2) Persistent discomfort with one’s own sex in aversion to one’s own genitalia or sex typed behavior, activities or clothing. Homosexuality *Not a mental disorder. *Possible genetic basis: Twin studies concordance rate is 52% for MZ and 22% for DZ, 11% for adopted brothers, and 9% for sons of homosexual fathers. Possible prenatal hormonal influence Possible Maternal immune response Differential socialization Identification with opposite-sex parent Intrauterine Causes Fetal Alcohol Syndrome- 1 in 600, flat cheeks, short nose, thin upper lip, flat filtrum, growth retardation, weak cognitive abilities, hyperactivity, attention deficits Fetal Alcohol Effected- 1 in 200-300, ADHD, lower IQ, math deficits, Asphyxia- maternal hypertension, toxemia, placenta previa, etc. Learning Disabilities Learning disabilities is a generic term that refers to a heterogeneous group of disorders manifested by significant difficulty in the mastery of one or more of the following: Listening, speaking, writing, reasoning, mathematical, reading, etc. Even though it may occur concomitantly with emotional disturbance, cultural differences, environmental influences, sensory impairment, etc. it is not the direct result of the conditions of influences. Subtypes of L.D. BASIC NONVERBAL LEARNING PHONOLOGICAL DISABILITY PROCESSING Neuropsychological DISORDER Deficits: visual/tactile Neuropsychological perception/visual Deficits: auditory memory/concept attention/auditory formation perception/verbal Early graphomotor memory/word deficits decoding/spelling/R.C. Tests commonly utilized when testing for learning disabilities: Intellectual: (WISC-IV, WAISIV,SBIV, WJ) Achievement: (WIAT-III, WJ) Rating Scales: (Vanderbilt, Conner’s, etc.) Teacher Observations: (Auditory, Visual, Behavior) Language Functioning: Recognizing Tics Simple Motor: Eye Blinking Neck Jerking Shoulder Shrugging Facial Grimacing Complex Motor: Facial Gestures Jumping Simple Vocal: Barking Coughing Grunting Hitting Throat Biting Clearing Stamping Sniffing Smelling Snorting objects Complex Vocal: Echolalia Coprolalia Palilalia Tourette’s Syndrome A tic is defined (DSM-IV-TR) as a “sudden, rapid, recurrent, nonrhythmic, stereotyped motor movement or vocalization. Three times more males than females. Co-morbid with OCD, ADHD, and LD TS requires at least two motor tics and one vocal tic. Must occur several times a day and be present for one year or longer. Coprolalia occurs in about 60%- clicks, grunts, yelps, barks, sniffs, snorts, coughs. Stereotypic Movement Disorders Head banging, body rocking, self-biting, self picking at skin, self-hitting, mouthing of objects. 3.5 times more often in boys than girls. In a study of 60 children under 10 years of age referred for EEG testing, 40% had pseudoseizures consisting of rhythmic movements or staring episodes. May be related to avoidance of aversive consequences. *Higher rates in abused children. Teeth Grinding/Bruxism Habitual gnashing, grinding, clicking, or clenching of the teeth. (male to female 3:1) May occur nocturnally or diurnally. Etiology: Learned behavior related to response to stress./ Malocclusion, rough teeth, oral infections Treatment: Bite block, psychotherapy, biofeedback, anxiety reduction Thumb Sucking Sucking of one or both thumbs, but may also include finger or fist sucking. Incidence: 45% of 2 year olds, 42% of 3 year olds, 36% of 4 year olds, 20% of 5 year olds, 5% of 11 year olds. Tends to occur when hungry, sleepy, frustrated, fatigue. May suck a blanket, rub a cheek with a pillow or blanket. Etiology: Tension Reduction Treatment: Aversion-nagging, gloves, splints, bandages, palital crib, pacifiers, foul tasting liquids PICA (307.52) *Commonly associated M.R. *Potential risk of lead, toxoplasmosis, hair balls, intestinal perforation. *For at least one month of eating non-nutritive substances inappropriate to developmental level. Obsessive-Compulsive Disorder Incidence: 0.2 % Obsessions: Irrational thoughts (fear, anxiety, need to avert perceived danger) “It doesn’t feel right.” Compulsions: Irrational behaviors (counting, checking, cleaning, etc.) Frequently co-morbid with ODD, ADHD, Anxiety disorders, phobias, learning disabilities (reading or language delays) Etiology: Unknown (PANDAS) Treatment: Psychodynamic, behavioral, family, pharmacotherapy Posttraumatic Stress Disorder Constellation of symptoms associated with trauma: A. Reexperiencing symptoms B. Avoidance C. Hyperarousal Intrusive thoughts, images, distressing dreams, detachment, Stressors associated with PTSD Parental Conflict, Family Deaths or Separation or Divorce Witnessing or learning of a traumatic event Child Physical or Sexual Abuse Serious Accident Serious Illness Natural DisasterTornado, Hurricane, Flooding, Earthquake, etc. Frequent Moveschanges in schools Victim of Assault Symptoms of PTSD Hypervigilance Difficulty sleeping Restricted Emotions Irritability or Anger Exaggerated Startle Avoidance of Response Nightmares Intrusive, distressing thoughts Flashbacks activities associated with the trauma: “I’m not going back to school.” Disruption of routine Detachment PTSD Continued Prevalence: 5-13 % following exposure to hurricanes, burns, physical abuse, cancer treatment. 43-70% following sexual abuse, schoolyard sniper attack, war trauma. Etiology: Cognitive,Behavioral, Neurobiological Treat 7-14 days after exposure. Individual and family therapy; medication, co-morbid problems. Trauma and the Brain Activation of higher cortisol levels. Chronic pain, digestive problems, weakened immune response. Hyper-vigilance (higher adrenal output) Changes in brain arousal level (dopamine, norepinephrine) Problems in shifting (serotonergic) controlling thoughts. Brain atrophy in multiple areas: amygdala, hippocampus, prefrontal, striatal, etc. 87 When working with trauma victims … Men do not disclose their histories of sexual and physical abuse easily. Victims fear being judged, feelings minimized, labels, being medicated, disbelief of others. Understand the power of threat.. “If you tell I will kill your sister.” *If you go there… you better have the skills to help! Do no harm! 88 Differential Response to Threat (Matthew Perry, Ph.D. www.childtraumaacademy.com) DISSOCIATION HYPERAROUSAL Detached Alarm Response Numb Flight-Panic Compliant Fight-Terror Suspension of Time Anxious Brief Psychosis Reactive Fainting Hypervigilance Freeze-Fear 89 Brain Plasticity Brain Plasticity means the brain changes because of experience. Neural connections occur because of learning. The brain becomes thicker and denser with learning. Depression may result in brain atrophy. Drug use results in neurochemical dysfunction. Mental Health Goals Reduce self-injurious behaviors Reduce agitation and aggression/Improve Self- control. Reduce anxiety/phobic behavior Reduce defiance/Improve Compliance Reduce psychotropic use. Reduce distractibility/Improve Attention to Task Reduce impulsivity/Improve Executive Functioning Symptoms of Depression in Children Depressed mood Irritability or Diminished interest in oppositionality Decreased energy or motivation Psychomotor retardation or agitation *2 weeks duration-5 or more symptoms. activities Sleep disturbance Weight loss or gain Inability to concentrate (attention problems) Assessment of Depression Self-Report Questionnaires: Child Depression Inventory, Reynolds Child Depression Scale, Beck Depression Inventory-II, Child Behavior Checklist, K-SADS (Co-morbid: learning disabilities, PTSD, ODD, ADHD, etc.) Rule-out: PDD, Anemia, PCS, Disease, Substance Abuse Meds for Adolescent Depression Avoid Tricyclic (cardiac/lethality) Avoid MAOI’s Avoid St. John’s Wort SSRI’s and SSNI are most commonly used. Some use of heterocyclics such as wellbutrin (bupropion) Consider- fish oils, melatonin, Vitamin D, B-12, B-6 Dysthymic Disorder Depressed Mood, most of the day, more days than not, for at least one year. *Two or more of the following: Poor appetite or overeating Low energy or fatigue Low self-esteem Poor concentration or difficulty making decisions Feelings of hopelessness The Delineation of Causation Predisposition Initiation Perpetuation Exacerbation 96 DSM-IV-TR Disorders of Childhood ADHD/ADD Autism PDD, Rett’s Childhood Disintegrative Disorder Asperger’s Oppositional Defiant Disorder Mental Retardation Reactive Attachment Disorder Tourette’s Learning Syndrome/ Disabilities Tic Disorders Disorders of Communication Depression Mood Dis. Motor Skills Disorder Separation Anxiety Selective Mutism, Conduct Disorder Feeding and Adjustment Eating Disorders Disorders PostTraumatic Stress Disorder Elimination Disorders Interviewing Children Use Age-Appropriate language: Children are are not likely to point out words they don’t understand. Avoid words such as, “guilty, depressed, anxious, disappointed”. They do understand “mad, sad, glad, and scared.” Sharing a snack or drink may build rapport. Be observant: activity level, physical appearance, mood/affect, parentchild interaction, coordination, etc. The Role of Attachment Children rely on a parents availability to provide comfort, safety and support. Insecurely attached children ignore their caretakers when distressed and have difficulty being soothed. RAD develops out of a pattern of parental psychopathology, abuse, neglect, etc. RAD tends to predict increased rates of aggression and mood lability. 99 Social Learning Exposure to aggression results in vicarious learning experiences. (Television, video games, role-models) Delinquent behavior can be learned through direct observation. Delinquent behavior can be reinforced and maintained by operant conditioning (affiliation, acceptance, reward) 100 Assessing Minority Children Guard against Inappropriate Generalizations: There is no monolithic black, HispanicAmerican, Native American, or Asian-American subculture. This can include lower-socioeconomic children. We must check for our own bias and prejudices as we assess. The Disruption of Community Abandonment Hostility/Fear Hopelessness Degradation Abuse/Neglect Poverty 102 Endocrinatic Influences Pituitary: Produces growth hormone Regulates Endocrine system Testes: Thyroid: Produces thyroxingrowth/brain development metabolism TestosteroneDifferentiation of male reproductive system and male sexual maturation Estrogen Progesterone Regulates menstrual cycle metabolism Ovaries: Adrenal Gland: Stimulates growth Pubescence Observing for Visual Impairments Rubs eyes constantly Shuts or covers one eye, tilts head, or thrusts head forward. Squints eyelids together or frowns Crossed eyes, inflamed or watery eyes Eyes itch, burn or feel scratchy Blurred vision, dizziness, headaches Observing for Hearing Impairments Frequent earaches/Sinus congestion Seasonal allergies Problems understanding spoken language. Inattention or lost in daydreaming. Often appears distracted or confused. Speech is loud. Turning head to hear. Frequent misunderstanding instructions. Observing for Language Impairments Articulation problems Fluency problems- abnormal rate and rhythm (stuttering & cluttering) Phonology problems-construction of word forms. Problems: listening, speaking, writing, reading. Loudness/Quality/Pitch (disorders of phonation/resonance Observing for Social/Emotional Impairments Externalizing- Aggressive, acting out Internalizing-Immature, Withdrawn Behavior Encopresis/Enuresis Self-stimulation: rocking, twirling, hand flapping, staring Language Deviations: echolalia Cognitive Impairments Lacks of Daily Living Skills Self-Injurious Behaviors Observing for Giftedness Exceptional Academic Achievement Exceptional Creativity Existence of Special Talents Insight-A qualitative difference in reasoning and thinking. Abstract thought High task commitment Alcoholism & Giftedness “Higher childhood mental ability was related to alcohol problems and higher alcohol intake in adult life.” 2008 American Journal of Public Health “For every 15 point increase in IQ there was a 1.27 times increase for alcohol abuse. Gifted teens tend to be more adapt at hiding their alcohol or drug abuse. Alcoholism in professional women is growing at exponential rates. A Primer on Regional Brain Functioning and Behavior •NEURONS: Cell body- Axon, Synaptic bulb, Synapse, Reuptake, Dendrite •PREFRONTAL CORTEX: Executive functioning, neural braking, inhibition, gating, linking, (Dopaminergic) •LIMBIC SYSTEM: Cingulate- shifting, Hippocampus- memory, Amygdalarecognition of emotional affect. (Serotonergic) •BASAL GANGLIA: "idle speed", (Noradrenergic) •TEMPORAL: Memory, temper Dopamine Effects • Working Memory • Shifting • Cognitive Set • Movement • Motivation • Too high dopamine may produce tics (basal ganglia pushed too far) 111 Serotonin Effects • • • • • Response Inhibition- (Holding back the action) Mediates Mood Stabilization Reduce obsessive/intrusive thoughts (Ventromedial Cortex) Reduce binges of (eating, sex, drugs, etc.) *Assigning value to stimulus. *Orbitofrontal Cortex Integrates smell, touch, sight, texture 112 What is ADHD? “ADHD is a common neurobiological disorder affecting 5-7% of the school age population. 80% will persist into adolescence and 50% into adulthood. It is characterized by deficits in executive functioning including: inhibition failure, working memory, sense of time, self-regulation of affect/motivation/arousal resulting in impaired rulegoverned behavior.” The Problem of Attention Old as Mankind- Attention is the heart of self-control. It bridges time. Inattention and Impulsivity of childhood connects excessive impropriety of adulthood and feeds addictions. Attention rides on a genetic and environmental substrate. To understand human weakness and strength we must understand Attention. 114 Etiology Of ADHD •Genetics: DRD2, D4RD, DAT-1 These gene patterns are overrepresented. Twin studies-The concordance rate for ADHD is 81% for MZ twins and 29% for DZ twins. •Diminished arousal in the prefrontal cortex as demonstrated through SPECT and PET scans. •FMRI's have smaller right hemisphere plana temporal than control group children. •Environmental Toxins: (alcohol, drugs, tobacco) •Pre/perinatal history (intraventricular bleeding, eclampsia, toxemia, precipitous birth/low birth weight etc.) •Diet, child-rearing, and common environmental toxins have been effectively ruled out as providing credible explanations for the etiology of ADHD. DSM-IV CRITERIA INATTENTION: Six or more (for six months) must be maladaptive and inconsistent with the child’s developmental level. (a) Often fails to give close attention to details or makes careless mistakes (b) Often has difficulty sustaining attention in tasks (c) Often doesn’t listen when spoken to directly (d) Often has difficulty organizing tasks and activities (e) Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (f) Often doesn’t follow through on instructions (g) Often loses things (h) Is often easily distracted (i) Is often forgetful DSM-IV Criteria, cont., Hyperactivity: Six or more for six months to a degree that is maladaptive and inconsistent with the child’s developmental level. (A) Often fidgets with hands or feet or squirms in seat. (B) Often leaves seat in which remaining seated is expected. (C) Often runs about or climbs excessively in situations where inappropriate. (D) Often has difficulty playing or engaging in leisure activities quietly. (E) Is often “on the go” or acts as if “driven by a motor”. (F) Often talks excessively. DSM-IV- Criteria, cont., IMPULSIVITY: (G) Often blurts out answers before the questions have been completed. (H) Often has difficulty awaiting turn. (I) Often interrupts or intrudes on others. B. Some hyperactive-impulsive or inattentive symptoms that caused impairment were present before age 7 years. C. Some impairment from the symptoms is present in two or more settings. D. There must be clear evidence of clinically significant impairment in social, academic or occupational functioning. E. Not better explained by PDD, or other disorders. The stimulant/abuse controversy “It is certainly true, for example, that some children with ADHD-many of whom are taking stimulant medication or have taken it some time in the past-become involved with substance abuse. It is even probable that a higher percentage of children with ADHD experiment with illegal substances than children who do not have ADHD. After all people with this disorder are among the most impulsive in our society, and many have been extremely unsuccessful in school and life in general. These are the factors that can lead to drug abuse. In fact, the evidence indicates that effective treatment of ADHD, which includes the use of stimulants in many cases, improves self-esteem and makes substance use less likely. Likewise a sizable proportion of the inmates of juvenile detention centers and prisons have a history of ADHD, and many of them have, at one time or another, been treated with Ritalin. However, the probability is that early treatment of these patients is more likely to prevent criminal activity than lead to it.” 119 “We now have the first statistical evidence that the treatment of ADHD in childhood Is protective against substance abuse in adolescence.” Joseph Biederman, Professor of Psychiatry at Harvard Medical School and Chief of Pediatric Psychopharmacology at Massachusetts General Hospital 120 International Consensus Statement January, 2002 1. ADHD is recognized as a valid disorder by: The U.S. Surgeon General, The American Medical Association, The American Academy of Child and Adolescent Psychiatry, The American Psychological Association, The American Academy of Pediatrics, among others. 2. ADHD is not a benign disorder. It can cause devastating problems including interfering with educational attainment, family functioning, social impairment, contributing to antisocial activities, increased use of tobacco and drugs, increased teen pregnancy, increased accident history, increased depression and personality disorders. 3. Neuro-imaging studies find metabolic differences. Twin studies indicated genetic contribution. It is not the result of poor parenting. 4. The media has misled the public by distorting scientific evidence about the disorder suggesting the disorder is not real or consists of trivial affliction. The debate continues… Do children become addicted to stimulant medication? The truth is that when stimulant medications are used to treat ADHD, there is no evidence that patients develop any addictive syndrome. Stimulant medication is a replacement that normalizes brain chemistry based upon PET scans. They do not get “high”, nor do they need ever increasing doses to achieve the same effect. Rather, the dose very often remains the same or may even diminish as the child gets older. Children on medications frequently skip the medication over the weekend or holidays. These children are not pilfering medication or whining for extra pills. Some children may “rebound” when the medication is wearing off with some increased irritability, but this is a minor side effect. Stimulant medications have remained a first line treatment of ADHD since the 1940’s with no evidence of serious side effects. Why then does the controversy continue? ADHD children have long-lasting and profound problems. To blame stimulant medication for the problems of ADHD children is like blaming insulin for the long-term sequelae of diabetes. (Thomas Spencer, M.D., Harvard Medical School) 122 COMORBIDITY AND ADHD TIC D. C.D. ADHD O.D.D. Aggres. Behavioral Inhibition Stop, Delay, Think, Analysis, Synthesis, Act. Hindsight/Forethought/ Time Awareness/ Self-awareness Reasoning/Create Rules/ (Inhibiting a Prepotent Response) Stop an ongoing response. *Interrupt Interference Control A New Theory of ADHD DEFICITS IN: INTERNALIZED SPEECH EMOTIONAL CONTROL WORKING MEMORY CREATIVE PROBLEM-SOLVING COMORBIDITY AND ADD Depress OCD ADD Anxiety L.D. WORKING MEMORY Holding events in mind. Retrospective functioning (hindsight) Prospective functioning (forethought) Sense of time Imitation of complex behavioral sequences Self-awareness Identified Deficits by Research Poor Persistence of Effort Perseveration of Responding- (Inflexibility) Impaired Behavioral Inhibition Deficits in Performance, not in knowledge or skill Planning, Sequencing, time conceptualization Greater Variability in work performance Less mature self-directed speech Less efficient mental calculation Reading comprehension Differential Diagnosis Tourette Learning Fragile X Syndrome Disability OCD Low IQ TBI PDD/Auti Anxiety Social Anxiety sm/Asp. Disorder/ADD ICD-NOS Depression/ A&D Dysthymia Abuse Physical Illness(Mono) PTSD Personality Disorders Conduct Disorder ODD Implications For Understanding ADHD It is more commonly a trait, than a pathology. It interferes with “free-will”. It is a disorder of performance, not lack of skill. It requires long spans of time to become fully evident to others. It creates great stress on the family. The family will look dysfunctional, but improves when the child is absent. It is contextually dependent. It becomes more complex over time due to the development of comorbid conditions such as ODD, CD, SA, LD, etc. It may not be a disadvantage in every situation. Evaluating for ADHD Clinical history: Genetic co-morbidity Screen for other neurological, psychological disorders Age of onset Severity of symptoms Setting DSM-IV criteria A brief measure of intellect- working memory, Rating scales. Achievement. Rule-out…odd, PDD, Tourettes, adjustment, etc. *TOVA, WCS, FD may give false positives or false negatives. Effects on the Family Increased marital tension. A. More disagreements. B. More supervision is required. C. More criticism by family members. D. More difficult to get babysitters. Negative Parental Feelings Associated with Parenting the ADHD Child Frustration Guilt Shame Fatigue Anger Helpless Denial Grief Fear Isolation Exhaustion Loneliness Confusion Sadness Anxiety Worried Parenting Principles for the ADHD Child Practice Forgiveness Keep a Disability Perspective Use Positive Reinforcement Make Rules External Vacation Away From Your Child Join a Support Group Increase the Immediacy of Consequences Stay Away from Unproven Treatments Parenting Principles, Cont., Choose your fights carefully Don’t neglect your spouse and other children. Modify expectations Grieve your loss of normalcy. Use token systems Learn about medication Become an advocate for your child. Educational Management Allow some restlessness. Be animated, theatrical. Create compliance opportunities. Increase prompting and cueing. Have access to rewards several times a day. Increase immediacy of consequences/Reward throughout the task. Increase frequency of consequences More frequent changes in consequences Maintain a disability perspective Don’t use multiple commands Educational Management Use token systems. 3 step command- Command-count 5, Warning-Count 5 (Raise voice), Time-out After time-out reward next good behavior. Use occasional exercise periods. Teach “Think-aloud” approach Sit child close to teachers desk Act Don’t Yak! Stop repeating your commands Avoid lengthy reasoning over misbehavior. Have child pre-state goals or rules. “Turtle Technique” “The evidence for drug efficacy and the side effects are so benign, that to refuse medication for the child with ADHD is tantamount to malpractice.” John Werry, M.D. Professor Emeritus of Child Psychiatry REWARD DEFICIENCY SYNDROME 1. 1954 James Olds discovered the ability to produce a reward sensation by activation of the mesolimibic dopamine pathways. (the medial hypothalamus) 2. Gerald McLearn produced an in-bred mouse (the C57) strain that bred true for a preference for alcohol, suggesting that alcoholism could have a genetic basis. 3. Dopaminergic and opiodergic reward pathways are critical for survival. They provide pleasure drives for eating, love and reproduction. These pathways can be reached by ‘unnatural rewards’ such as alcohol, cocaine, nicotine, and other drugs, and by compulsive activities such as sex, gambling, and eating. Activation of these pathways produce an agents addictive properties. 139 4. The primary neurotransmitter for reward is dopamine, however norepinephrine, serotonin, GABA, Cannabinoid, and Opioid neurons modify metabolism. 5. Dopamine influences mood and affect along with inhibition and executive functioning thus influencing motivation. 6. Heroin increases the neuronal firing rate of dopamine cells. Cocaine inhibits the reuptake of dopamine. Combined these two drugs produce even more intensive dopamine activation. (speed-ball) 7. Repeated drug use produces neuroadaptive changes causing normal rewards to lose their motivational significance. (motivational toxicity)/ Sensitization occurs. 140 The effects of a dopamine agonist on recovery for the A2/A2 as compared to the A1/A1 141 Types Of Medications STIMULANTS- Ritalin, Dexedrine, Adderall, Metadate, Concerta, Focalin, Vyvanse, Daytrana, Methylyn, etc. (Enhance dopamine release and concentration in the synapse.) Improves inhibition, attention, memory storage and retrieval, time management, self-regulation of affect, improved internalization of speech, fine-motor control, improved reasoning. ANTIHYPERTENSIVES- Clonidine, Tenex (reduces arousal, improves sleep, improves frustration tolerance, decreases aggression) ANTICONVULSANTS-Tegretol, Depakote (may reduce aggression) ANTIDEPRESSANTS: (Tricyclics)- Tofranil, Norpramine (may improve self-regulation of affect) (SSRI’s)- Prozac, Celexa, Paxil, Zoloft, Effexor (May improve inhibition and control of affect) NEUROLEPTICS: Risperdal, Zyprexa, (may improve reality orientation, decrease aggression) Medication In Special Populations SUBSTANCE ABUSE: Stimulant mediation use decreases rather than increases the risk for drug abuse in adolescence and adulthood. Stimulant medication may even reduce the risk of relapse of substance abusers after treatment. CONDUCT DISORDER: Symptom severity appeared reduced in the shortterm. MINORITIES: African-Americans are 2.5 times less likely to receive methylphenidate than Caucasian youths. HEAD INJURY: MPH appears to be an effective treatment for post TBI cognitive and behavioral sequelae in the brain injured child. Speed of mental processing appears improved while motor speed is unaffected. TOURETTES: Both anti-hypertensive and stimulants have been used successfully in the treatment of Tourette’s. Diagnostic Criteria for Oppositional Defiant Disorder A. A pattern of negativistic, hostile, and defiant behavior lasting at least six months, during which four (or more) of the following are present. 1. Often loses temper 2. Often argues with adults 3.often actively defies or refuses to comply with adults’ requests or rules. 4.Often deliberately annoys people. 5. Often blames others for his or her mistakes or misbehavior. 6. Is often touchy or easily annoyed by others 7. Is often angry and resentful 8. Is often spiteful or vindictive. Diag. Criteria for ODD Cont., B. The disturbance in behavior causes clinically significant impairment in social, academic, or occupational functioning. C. The behaviors do not occur exclusively during the course of Psychotic or Mood Disorder. D. Criteria are not met for Conduct Disorder, and if the individual is 18 years or older, criteria are not met for Antisocial Personality Disorder. ASSOCIATED FEATURES: Depressed mood, Learning Problems, Hyperactivity, Addiction What Do You Believe Discipline Is? Influencing Controlling Training, coaching Correcting Tutoring, guiding Governing Informing, preparing Punishing, rebuking Familiarizing, Reproving, containing Enlightening Restraining, managing Encouraging Supervising Harnessing Diagnostic Criteria for Conduct Disorder A. A repetitive and persistent pattern of behavior in which the basic rights of others or major age-appropriate societal norms or rules are violated, as manifested by the presence of three (or more) of the following criteria in the past 12 months, with at least one criterion present in the past six months. AGGRESSION TO PEOPLE AND ANIMALS 1. Often bullies, threatens, or intimidates others 2. Often initiates fights 3. Has used a weapon that can cause serious physical 147 harm. C.D. Criteria Cont., 5. Has been physically cruel to animals. 6. Has stolen while confronting a victim. 7. Has forced someone into sexual activity. DESTRUCTION OF PROPERTY 8. Has deliberately engaged in fire-setting with the intention of causing serious damage. 9. Has deliberately destroyed others’ property DECEITFULNESS OR THEFT 10. Has broken into someone else’s house, building, or car. 11. Often lies to obtain goods 148 or favors or to avoid obligations Conduct Disorder TYPE ONE TYPE TWO Uncontrolled Derives affective aggression Generalized anxiety Depression Worried Frustrated Reactive reinforcement from aggressive acts. Predatory Unexcited when engaging in aggressive acts. Deliberate More likely to progress to antisocial 149 Best Practice for Conduct Disorder Treat the co-morbid disorder (ADHD, SUD, M.R.) Family interventions- Treat parental pathology Individual & Group psychotherapy. Psychopharmacology Other: juvenile justice, social services, community resources, out of home placement, school interventions, independent living skills. 150 Why are kids so angry today? Major Losses Mistreatment Abuse Lack of Opportunity Devaluation Crushed Dreams Pain Discrimin ation Mental Illness Lack of guidance Violence in the Media Loss of Family of Origin Relocation Increasing Demands Victims of Bullying Loss of Community Increased Academic access to Demands drugs/alcohol Parents out of touch with reality Fear Loss of Childhood/In nocence Loss of emotional Support Adult Roles Loss of Religious Guidance Lack of Boundaries Character Education is lacking Lack of time with responsible adults Lack of access to medical/ment al health professionals 151 Work Demands Neglect EXPLANATIONS FOR DEFIANCE Co-Morbid Problem such as ADHD Bad Role Models Frustration/Stress Neglect/Social Skill Deficits Mood Disturbance/Temperament Maltreatment/Abuse-Pain Ineffective Discipline/Inconsistent Grief & Loss Low Cognitive Functioning Brain Injury *Other mental health disorders To Restrain or Not? The problem with The problem of not restraint is it risks injury to the client or staff. restraining is it risks injury to the client or staff. 153 “There is no national standard for the use of seclusion and restraint. Thus, there is considerable variability including potentially dangerous and unsafe practices.” 154 Agree or Disagree? (1) Restraints keep people safe. Staff know how to recognize potentially violent situations Restraints are therapeutic. Seclusion encourages self-control. Most who have been restrained see it as a helpful experience. There are national standards for restraining children. Seclusion and restraint reflect treatment failure. 155 Agree or Disagree? There is no such thing as “the right way” to intervene. If you believe there is a “right way”, what is it? There is such a thing as “the wrong way” to intervene. If there is a wrong way to intervene, what is it? You can be following protocol and procedure and still be wrong. If you don’t follow protocol and procedure, it is guaranteed you are wrong. 156 Potential Effects of Reinforcers in Behavioral Interventions Student Reinforcers Sense of Empowerment Peer Attention Anxiety Reduction Victim Image Peer Sympathy Escape from boredom Opportunity to be aggressive. 157 Staff Reinforcers Ends the Acting out Restores safe environment. Sense of empowerment. Peer Recognition Retribution-Frustrationelicited aggression Important Considerations before Seclusion and Restraint Consider the cognitive age of the child, not merely the chronological age. Consider the sexual development of the child and staff supervision or intervention. Consider medical diagnosis (particularly cardiac, epilepsy, brain injury, asthma, etc.) Consider substance or medication issues. Consider mental health diagnosis. Are staff CPR trained? Is safety equipment available? (ventilation bag & mask?) Has each child been screened for appropriateness or hazards to restraint? 158 What happens next….? If a child dies while in or following a restraint? If a limb is dislocated, a broken rib punctures a lung, a concussion occurs from falling on a concrete floor, an asthma attack from dust in the carpet) *Could the staff quickly determine if these have occurred and how would they respond? If a staff member is seriously or critically injured or is killed during a restraint? 159 Disorders Associated With Rage or Aggression Oppositional Defiant Disorder Conduct Disorder Intermittent Explosive Disorder Impulse Control Disorder-NOS Bi-Polar Disorder Disorders of delirium Traumatic Brain Injury Substance Abuse Disorders Reactive Attachment Disorder Mental Retardation Personality Disorders 160 Helping the Explosive Child 1. Use “No” sparingly. Choose your battles wisely. 2. Ignoring will likely make the child worse. 3. Ask, “Why can’t my child think his way through frustration.” Complexity increases with age. Seek a thorough evaluation. 4. Therapy should involving learning new strategies and PRACTICING new strategies experientially. 5. Most children with severe anger problems have a comorbid disorder that must be treated simultaneously. 6. Multiple disciplines (Psychological, Educational, Medical, must communicate with each other.) Helping the Explosive Child, Cont., 7. Learn about medication management. Be especially aware of serious side effects of antipsychotics and anti-seizure medications. 8. Do not protect your child from appropriate consequences and use his diagnosis as an excuse for irresponsible behavior. Holding the child accountable is essential to change! 9. Seek an experienced and skilled clinician. Complexity increases over the development of the child. Seek to correctly identify etiology. 10. Are the behaviors related to a character disorder, neurological disorder, or psychological disorder? Helping the Explosive Child., Cont. 11. Remember, remorse doesn’t keep an angry-impulsive child from being impulsive. Be aware that the angry-impulsive child is at greater risk of suicide than the depressed child. 12. Assess lethality towards family members as well as suicidal behavior. Are behaviors threatening and predatory? Does this child belong in the household? 13. Rule-out brain injury: Look carefully at the neurological history of the child. Children with evidence of brain injury have 5 times the number of serious behavior disorders and generally require medication for stability. 14. Provide a predictable, organized, warm environment. Reducing Aggressive Behavior in Children Use storytelling that Assist parents in emphasizes nonaggressive solutions. Praise students for non-aggressive solutions for difficult problems. Model non-aggressive behavior. developing behavior plans and reducing corporal punishment. Daily character development: “forgiveness, compassion, understanding, tolerance, etc. De-escalation Techniques Communicate with Become aware of calmness and clarity. Do not challenge, threaten, or demand compliance! Approach at an angle and identify a path of escape Avoid a threatening posture obstacles or dangers. Listen accurately and restate/reflect. Show compassion and understanding. Do not become argumentative, insulting, demeaning, inciting, or intimidating. De-escalation cont., Keep hands free and in a non-threatening manner. Maintain good eye contact, but do not stare. Seek to redirect or change the setting to a more safe setting. If attacked or threatenedmake others immediately aware. Follow your gut feeling about when to get help. Use the person’s name. Avoid body contact. Do not touch for reassurance! If possible give him and you a path of escape. Move outside an office into a common area. Seek to involve others in decision making and deescalation. The Child’s Response To Divorce Emotional distress, sadness, anger Regression- 6 months to 1 year After the initial disequilibrium there is a 2-3 year adjustment period. The divorce interferes with the child’s ability to inhibit anger/aggression. It serves as a stimulus for catharsis. The Influence/Impact of Divorce Separating or Children feel helpless divorcing adults are significantly distressed. Children are exposed to unhappy, possibly depressed or anxious parents. and frightened and often view unhappy scenes. Parents are consumed with their own emotional reactions and often neglect the child’s reactions Parental Conflict During Divorce High conflict between parents exacerbate the child’s emotional problems. Children should not be witness to displays (including phone calls) of name-calling, yelling, threatening, or other aggressive behavior. Divorce and the school-age child Resents the strict schedule often imposed upon him. The visitation schedule often disrupts the child’s developmental and social needs. The child of divorce often resents the loss of control over their lives compared to their peers. There is often a downward economic shift after divorce. The child often doesn’t fully understand this and resentments increase towards both parents. Post-Divorce Issues Parents must agree on issues of transition arrangements School choices Access to information Discussion regarding relocations. Vacations and holidays Significant others/Remarriage Both parents should agree upon disciplinary plans and behavior management. Additional Concerns with Divorce Depends upon the parents ability to demonstrate self-control. Visitation is often irregular. The relationship with the father changes significantly. The father often begins dating or remarriage. There is often geographical isolation. Post-Divorce Issues -Cont., Fathers assist in valuing her femininity. Low feminine self-esteem resulting in more negative attitudes towards self and conflicts with her father. Early childhood divorce is linked to oppositional behavior, anxiety, and hyperactivity. Mother Custody 84% of children reside with their mother. Most divorced women work full time. Placement in day-care facilities often result in increased illnesses the first year. There is often less affection, more coercion, less communication, and less consistency in control and monitoring. Children are often expected to “mature faster” and take on greater responsibility for self. Joint Custody It encourages the active involvement of both parents. Encourages child support payments because of this involvement. Provides relief from child care for both parents, thus improving quality of life. Emotionality in Preschool Children They may be fearful or anxious. They have emotional meltdowns. Become aware of where they have been, how they were treated, where they are, and where they are going. Low Frustration Tolerance Difficulty Delaying Gratification Generally impulsive Assessing for Child Maltreatment Aggression Clinging Behavior Social Somatic Withdrawal Complaints NonEnuresis/En Affective Compliance copresis Symptoms Overeating/ Undereating Sleep Poor Disturbance Hygiene Sexual Acting out Inadequate Dress The Effects of Fatherlessness 71% of high school 85% of all youths in dropouts come from fatherless homes. 80% of rapists come from fatherless homes. 85% of children with behavioral disorders come from fatherless homes. 90% of homeless and runaway children come from fatherless homes. prison are from fatherless homes. 70% of youths identified delinquent are from fatherless homes. Children from a fatherless home are: 5 times more likely to commit suicide. 32 times more likely to run away. 20 times more likely to have behavioral disorders. 14 times more likely to commit rape. 10 times more likely to abuse chemical substances. 9 times more likely to end up in state custody 20 times more likely to end up in prison. Psychological Maltreatment TERRORIZING SPURNING: Threatening to Verbal Battery; kill or abandon the child. Exposing the Calling Names child to violence Humiliation ISOLATING: WITHHOLDING CARE Physical health, education, behavioral, etc. EMOTIONAL NEGLECT: EXPLOITING Exposure to pornography, modeling and teaching criminal behavior. Refusing family interaction. Locking the child up for an extended period of time. Refusing affection, absence of love, caring. Munchausen’s Syndrome by Proxy *Frequent unexplained illnesses in child. *Excessive trips to E.R. or physician. *Child may appear overmedicated. *Parent may act appropriately around others. *Parentally induced symptoms. Thank you for your attendance here today! For questions please contact me at willbeyerlpe@gmail.com Or 731-217-1358 or 731-660-2850