Kaplan Medical Template Design
advertisement
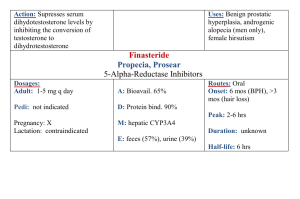
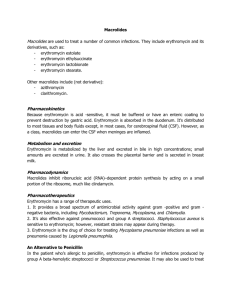
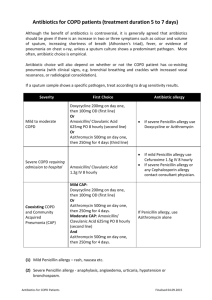
NAPLEX ANTIMICROBIAL AGENTS Selecting Appropriate Antimicrobial Agents PG 52 Empiric therapy Identify the causative organism Test the sensitivity of the organism to antimicrobial drugs Identify important host factors: Site of infection-CNS, bone, prostate, UTI Susceptibility to toxicity Patient allergies Mechanisms of Action of Antimicrobial Agents Interference with cell wall synthesis penicillins, cephalosporins Inhibition of protein synthesis macrolides, clindamycin, tetracyclines, quinolones Interference with enzyme unique to bacterial cell sulfonamides Interference with the permeability of microbial cell membranes PG 52 amphotericin B Sulfonamides PABA dihydrofolic acid (DHFA) Sulfa PG 53 tetrahydrolfolic acid (THFA) General considerations - Sulfonamides Mechanism of action : competitive antagonism of PABA in enzyme system essential for bacteria growth. For ophthalmic use, sulfa sodium salt solutions are very alkaline (i.e., pH 10+). The only sodium salt suitable for ophthalmic use is sulfacetamide sodium (solutions have pH of about 7.4). Sulfas are eliminated renally unchanged. Makes them good for UTIs. Sulfas are less soluble in acid urine. This is one cause of crystalluria. Stevens-Johnson syndrome is associated with sulfa use. PG 53 General considerations – Sulfonamides (cont’d) Combinations of sulfamethoxazole and trimethoprim (Bactrim, Septra, etc.) are less likely to result in bacterial resistance. Sulfasalazine (Azulfidine) is used in treating inflammatory bowel disease and RA. Watch for sulfa allergy, salicylate allergy, and urine discoloration. - GI side effects, dose is titrated upward slowly, monitor blood counts – dyscrasias If a patient cannot use sulfasalazine because of sulfa sensitivity, use mesalamine products, i.e., Asacol, Pentasa, Rowasa. – various dosage forms Remember that silver sulfadiazine (Silvadene) and mafenide (Sulfamylon) are used topically for treatment of serious burns. PG 53 Penicillins PG 54 General Considerations – Penicillins Mechanism of action: interfere with bacterial cell-wall synthesis (bactericidal) Note that all penicillins have a beta lactam ring and thiazolidine ring. Possible cross-sensitivity with other beta lactam antimicrobials (e.g., cephalosporins). - percent cross-sensitive ranges from 5-7% PG 54 Structure Activity Relationships: AMino penicillins – AMpicillin, AMoxicillin, bacAMpicillin NOX penicillins – penicillinase (beta lactamase) resistant penicillins: Nafcillin, OXacillin, clOXacillin (PO), diclOXacillin(PO)----MSSA (vanco alternative) MEZPCT penicillins – antipseudomonal penicillins: MEZlocillin, Piperacillin, Carbenicillin, Ticarcillin (combo with aminoglycosides, not in the same IV) Therapy problems with penicillins: PG 55 Acid Resistance Beta-lactamase (penicillinase) resistance (combo products; Zosyn, Timentin, Augmentin) Hypersensitivity Which of the following is an adverse effect associated with use of aminopenicillins? a. polydipsia b. hemolytic anemia c. cholelithiasis d. tardive dyskinesia e. angina Which of the following is an adverse effect associated with use of aminopenicillins? a. polydipsia b. hemolytic anemia c. cholelithiasis d. tardive dyskinesia e. angina Cephalosporins PG 56 General considerations Contains beta-lactam ring. Therefore, may have cross-sensitivity with penicillins. As you go from 1st generation to 4th generation, you get: PG 56 increased gram-negative activity decreased gram-positive activity increased resistance to beta-lactamase destruction increased ability to enter cerebrospinal fluid Which of the following antimicrobial agents has effective coverage of streptococcus pneumoniae? I. amoxicillin II. doxycycline III. gentamicin a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following antimicrobial agents has effective coverage of streptococcus pneumoniae? I. amoxicillin II. doxycycline III. gentamicin Gram + Non-DRSP a. I only b. III only c. I and II only d. II and III only e. I, II, and III General considerations (cont’d) First generation (generally start with CEPH): Good for surgical prophylaxis Second generation (generally start with CEF): Good for otitis, sinusitis and respiratory tract infections Third generation (generally end with IME or ONE): ● Good for meningitis, CAP, gram-negative bacilli, gonorrhea, Proteus, Salmonella, Klebsiella ● Cefixime (suprax), cefotaxime (claforan), ceftriaxone (rocephin) Fourth generation (cefepime) Maxipime: ● PG 57 Good antipseudomonal activity Tetracyclines PG 58 General Considerations Products: Tetracycline HCI (Achromycin V, Sumycin, Robitet, Panmycin) Minocycline (Minocin) Doxycycline (Vibramycin, Doxy 100, Doxychel, Vibra-Tabs) These are bacteriostatic antimicrobials. They interfere with protein synthesis. Broad spectrum antimicrobials. Work against many gram-positive and gram-negative organisms. - also effective against atypical organisms mycoplasma and chlamydia pneumoniae, useful for patients allergic to penicillin b/c gram + coverage PG 58 General Considerations Not for use in children under age 8. May cause discoloration of developing tooth enamel. Not for pregnant women. May adversely affect fetal development. Most have the potential for causing phototoxicity. Drug interaction with divalent (Mg, Ca, Fe) or trivalent (Al) compounds and tetracyclines may result in complexation and impaired absorption. Do not use together. Broad spectrum activity can lead to thrush or vaginal candidias PG 58 Macrolides General Considerations: Bacteriostatic – inhibit protein synthesis May be good for patients who are hypersensitive to beta-lactam antimicrobials. Good respiratory coverage. CAP caused by S.pneumo, M.cat, H.flu or atypicals (mycoplasma, legionella, and chlamydia) PG 59 Erythromycin Oral Products Erythromycin base (E-Mycin, Ery-Tab, PCE, Eryc) Coating used on most products Administer on an empty stomach Erythromycin stearate (Erythromycin Stearate, Wyamycin S) Better absorbed than erythromycin base PG 59 Erythromycin (cont’d) Erythromycin esolate (Ilosone) Associated with cholestatic hepatitis Better absorbed than erythromycin base Erythromycin ethylsuccinate (eryPed, E.E.S.) Most well absrobed Available in liquid form 400 mg of EES = 250 mg of erythromycin base Parenteral Products Erythromycin lactobionate Erythromycin glucepate Drug Interactions: Mainly due to enzyme inhibition of erythromycin – (3A4) PG 59 Clarithromycin (Biaxin) Usually used BID. XL form used once daily. Prodrug: May be given with or without meals Used in combination with a proton pump inhibitor for H. pylori treatment. Metallic taste PG 60 Azithromycin (Zithromax) More gram-negative activity than erythromycin or clarithromycin Once-daily dosing, usually for five days after otitis media (e.g., Z-Pack) Available as suspension, tablets, IV Suspension should not be taken with food or antacids. Dirithromycin (Dynabac) Prodrug Once-daily dosing PG 60 Lincosamides General considerations Watch for pseudomembranous enterocolitis (Clostridium difficile). •Treat clostridium with metronidazole (Flagyl) or oral vancomycin. Good in gram positive (staph) and gram-negative infections, particularly anaerobes Lincomycin (Lincocin, Lincorex) Morbilliform rash possible; DC drug if it happens Clindamycin (Cleocin) Available in topical form for acne PG 61 Which of the following antibiotics has bacteriostatic activity? a. amoxicillin b. ciprofloxacin c. erythromycin d. penicillin e. cephalexin Which of the following antibiotics has bacteriostatic activity? a. amoxicillin (cell wall) b. ciprofloxacin (inhibits DNA gyrase) c. erythromycin (protein synthesis) d. penicillin (cell wall) e. cephalexin (cell wall) Aminoglycosides General Considerations Glycosides – poorly absorbed from the GI tract Bactericidal Good for serious gram-negative pathogens (pseudomonas, proteus, etc.) Frequently administered with extended-action penicillin (IV incompatible) - dosed q8h or q24h (conc. dependant kill) Eliminated by glomerular filtration; Watch for ototoxicity Monitor peaks and troughs – peaks 30 min after infusion, trough 30 minutes before next dose. peak = 4-10ug/ml trough = 0.5-2, adjust dose if CrCl < 60ml/min. hearing test if prolonged therapy PG 61 Which of the following antimicrobial agents is available for parenteral use only? I. cefaclor II. tobramycin III. ticarcillin a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following antimicrobial agents is available for parenteral use only? I. cefaclor II. tobramycin III. ticarcillin a. I only b. III only c. I and II only d. II and III only e. I, II, and III Parenteral use Reference Peak Range Streptomycin sulfate Kanamycin sulfate (Kantrex) Gentamicin sulfate (Garamycin (4mcg-10mcg/ml) Tobramycin sulfate (Nebcin) (4mcg-10mcg/ml) Amikacin sulfate (Amikin) (15mcg-25mcg/ml) Netilmicin sulfate (Netromycin) PG 61 Which of the following antibiotics requires monitoring of serum levels? a. penicillin b. ceftazidime c. azithromycin d. gentamicin e. cephalexin Which of the following antibiotics requires monitoring of serum levels? a. penicillin b. ceftazidime c. azithromycin d. gentamicin e. cephalexin Oral use Not for systemic action Neomycin sulfate (Mycifradin) - Used for bowel prep prior to surgery , treat diarrhea caused by e.coli, neomycin also binds ammonia, use in patients w/hepatic encephalopathy, watch for absorption interactions Tobramycin (TOBI) – inhaled product for CF patients PG 62 Fluoroquinolones General Considerations - Inhibits DNA-Gyrase May cause phototoxicity Not for patients under 18 – affects growth Do not use within 2-4 hours of antacids; iron – also inhibits CYP1A2 (increased levels of theophylline and caffeine) Generally useful for UTI, lower respiratory infections, gonorrhea, prostatitis – older agents have more gram -, less gram + coverage, newer agents have broader gram + [moxifloxacin, gatifloxacin] All end in -oxacin PG 62 Names Second generation Norfloxacin (Noroxin) – high urine levels - UTIs Ciprofloxacin (Cipro)- renal elimination: reduce dose Ofloxacin (Floxin) Third generation Levofloxacin (Levaquin) – renal elimination: reduce dose Sparfloxacin (Zagam) – reports of prolongation of QT interval (D/C) Gemifloxacin (Factive) – renal elimination: reduce dose, skin rash Fourth generation Moxifloxacin (Avelox) – Multi-drug resistant Streptococcus pneumonia (MDRSP) PG 62 MISCELLANEOUS ANTIMICROBIAL AGENTS Antibacterials Mupirocin (Bactroban) – topical use for impetigo, intranasal for staph Vancomycin (Vancocin) – associated with red man syndrome (must be infused slowly, over min of 30 minutes); reserved for serious/resistant gram + infections (MRSA, enterococcus) – rapid drop in BP accompanied by rash in neck or chest area - Monitoring – 1 hour before and 1 hour after - Peak – 25-40mcg/dl & Trough 5-12mcg/dl Metronidazole (Flagyl) – active against gram-negative organisms and protozoa, (anaerobes) Avoid alcohol. May darken urine. PG 63 MISCELLANEOUS ANTIMICROBIAL AGENTS (cont’d) Carbapenems •broad spectrum; used for resistant gram +/– organisms, pseudomonas, MRSA, enterococcus, anaerobes •similar to penicillins (cross-sensitivity) but b-lactamase resistant •Risk of seizures and renal adjustment Imipenem/cilastatin (Primaxin) – cilastatin is a renal dipeptidase inhibitor Meropenem (Merrem)---lacks good pseudomonas coverage Doripenem (Doribax) Ertapenem (Invanz) ----Aztreonam (Azactam)---monobactam, ok with PCN allergy PG 63 Which of the following antibiotic is classified as a macrolide? a. telithromycin b. tobramycin c. azithromycin d. doxycycline e. kanamycin Which of the following antibiotic is classified as a macrolide? a. telithromycin b. tobramycin c. azithromycin d. doxycycline e. kanamycin MISCELLANEOUS ANTIMICROBIAL AGENTS (cont’d) VRE and MRSA drugs Quinupristin / dalfopristin (Synercid) – Linezolid (Zyvox) –……oral dosing available Tigecycline (Tygacil) – Chloramphenicol (Chloromycetin) – for typhoid fever; may cause aplastic anemia and gray baby syndrome PG 63-64 Pneumonia Organisms: Treatment: --Comorbidities: Chronic obstructive pulmonary disease (COPD), diabetes, chronic renal failure, chronic liver failure, heart failure (HF), cancer, asplenia, immunosuppressed Pneumonia Treatment: --Risk factors for MDR organisms: recent antibiotic therapy (in last 90 days), hospitalized ≥ 5 days, resistance in environment, nursing home resident, chronic dialysis, home infusion therapy, immunosuppressed Meningitis Organisms: Treatment: Urinary Tract Infection Organisms: Treatment: STDs Organisms: Treatment: Antitubercular Drugs R I P E S PG 64 rifampin isoniazid pyrazinamide ethambutol streptomycin Antitubercular Drugs Isoniazid (Nydrazid, Laniazid) May cause B6 deficiency – supplement malnourished, alcoholics, kids Used for prophylaxis or in combo with other drugs for active disease 6 months of prophylaxis if +PPD; For treatment used in combo with rifampin for at least 6 months Metabolized by acetylation (slow versus rapid acetylators) monitor for hepatoxicity Rifampin (Rifadin, Rimactane) Potent enzyme inducer (potential drug interactions with many drugs) Potentially hepatotoxic; Use may result in discoloration of virtually all body fluids (urine and tears----watch contact lenses) PG 64 Antitubercular Drugs (cont.) Ethambutol (Myambutal) – for treatment of MAC and drug-resistant Tb as part of combination therapy - optic neuritis is a rare but serious side effect - monitor with eye exams Pyrazinamide – used in combination therapy; potentially hepatotoxic - may increase uric acid levels Steptomycin- can be used as fourth drug in regimen instead of pyrazinamide PG 65 Antimalarials Quinine sulfate (Quinamm) – also used for muscle cramps; no longer used due to hematologic adverse effects Doxycycline – tetracycline; possible phototoxicity and binding interactions Melfoquine HCl (Lariam) – may cause neuropsychiatric adverse effects; once- weekly dosing Atovaquone/proguanil (Malarone) – newer product; once daily; do not use if renally impaired PG 65 Antimalarials Chloroquine (Aralen) – may worsen psoriasis symptoms Hydroxychloroquine sulfate (Plaquenil Sulfate) – may worsen psoriasis symptoms - also used as a DMARD for RA; phototoxicity, hematological side effects, ocular and ototoxicity Primaquine phosphate – take with food to reduce GI upset; may be used for PCP PG 66 HIV Antiretroviral Therapy Therapy initiated based on CD4 count, viral load and presence of symptoms Initial regimen in treatment naive patients: • NNRTI + 2 NRTIs • PI + 2 NRTIs PG 69 Learn drug class representatives and major toxicities Which HIV drug is correctly matched with its mechanism of action? a. Lamivudine - nucleoside reverse transcriptase inhibitor b. Enfuvirtide - protease inhibitor c. Stavudine - binds to human CCR5 receptor d. Didanosine – protease inhibitor e. Indinavir – blocks virus entry into human cells and subsequent viral replication Which HIV drug is correctly matched with its mechanism of action? a. Lamivudine - nucleoside reverse transcriptase inhibitor b. Enfuvirtide - protease inhibitor c. Stavudine - binds to human CCR5 receptor d. Didanosine – protease inhibitor e. Indinavir – blocks virus entry into human cells and subsequent viral replication NNRTIs non-nucleoside reverse transcriptase inhibitors (vir in the middle) Delavirdine (rescriptor) (rash, LFTs) Efavirenz (Sustiva) Drug of choice Category X, vivid dreams Nevirapine (Viramune) Rash (Steven Johnson Syndrom) Liver metabolism PIs Protease inhibitors (vir at the end) Exception – darunavir, tenofovir, raltegravir, abacavir Metabolized through the liver (commonly 3A4) • potential for significant drug interactions Low dose of ritonavir frequently used to enhance the concentrations of coadministered PIs Adverse effects: GI intolerance, hyperglycemia, dyslipidemia, lipodystrophy, LFT alterations PG 72 NRTIs nucleoside reverse transcriptase inhibitors (all the others) Exception – maraviroc All NRTIs (except abacavir) are excreted renally; require dose adjustment but few drug interactions Most common ADRs – GI intolerance, typically subsides in first couple of weeks - High risk for perpheral neuropathy Black Box warning: Risk of lactic acidosis with hepatic steatosis PG 69 AIDS – Opportunistic Infections PCP / PJP (pneumocystis carninii pneumonia) CMV retinitis Macrolide + ethambutol Cryptococcus neuformans meningitis PG 74 Ganciclovir MAC / MAI (mycobacterium avium complex) trimethoprim-sulfamethoxazole Amphotericin B +/- flucytosine Fluconazole used for maintenance Drugs for influenza M2 inhibitors Amantadine, rimantidine Effective for influenza A virus only Begin within 48h of symptom onset; continue 2-5 days Neuroaminidase inhibitors Oseltamivir (Tamiflu) Zanamivir (Relenza) Effective for influenza A and B viruses Begin with 48h of symptoms onset; continue 5 days PG 74 Drugs for herpes simplex and herpes zoster (shingles) Acyclovir (Zovirax) – for herpes simplex types 1 and 2 - dosed 5x/day for 10 days, 5 days if recurrence Penciclovir (Denavir) – topical treatment for herpes labialis (cold sores) Valacyclovir HCl (Valtrex) – for herpes simplex and herpes zoster; acyclovir prodrug Famcyclovir (Famvir) for herpes simplex and herpes zoster (shingles); penciclovir prodrug - begin therapy as soon as first sign of lesion Docosanol (OTC-Abreva) topical cream PG 75 Anthelmintic drugs of choice Nematodes (roundworm) Mebendazole (Vermox)—do not use in pregnancy – blocks glucose uptake Albendazole (Albenza) – degeneration of cytoplasmic microtubules intestinal cells of helminths Piperazine citrate Preg B – blocks affect of ACH Pyrantel pamoate (Antiminth) Trichuriasis (whipworm) Mebendazole (do not use in pregnancy) Hookworm – mebendazole (do not use in pregnancy) PG 75 Which of the following medication(s) can cause nephrotoxicity? I. II. III. Ganciclovir Foscarnet Gentamicin a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following medication(s) can cause nephrotoxicity? I. II. III. Ganciclovir Foscarnet Gentamicin a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following agents inhibits the HIV enzyme reverse transcriptase? I. zanamivir II. ritonivir III. didanosine a. I only b. III only c. I and II only d. II and III only e. I, II, and III Which of the following agents inhibits the HIV enzyme reverse transcriptase? I. zanamivir (Neuroaminidase inhibitors) II. ritonivir (protease inhibitor) III. didanosine (nucleoside reverse transcriptase inhibitors) a. I only b. III only c. I and II only d. II and III only e. I, II, and III DERMATOLOGIC STUDY OUTLINE Acne Pathophysiology— abnormal keratinization leads to obstruction of the follicle and accumulation of sebum to form a closed comedo or “white-head” Goal of therapy is to unblock follicles PG 146 Normal Pore Inflamed Pore Dermatologic Study Outline PG 146 Dermatologic Study Outline Isotretinoin (Accutane) Effective therapy option for the treatment of severe, inflammatory acne, or more moderate forms that have been refractory to other treatment options pregnancy category X two forms of contrception, iPLEDGE program Oral Antimicrobials • Tetracycline • Erythromycin • Clindamycin PG 146 Psoriasis Pathophysiology — exact mechanism unknown. May be due to defects in epidermal cell cycle, AA metabolism, immunologic mechanisms, environmental triggers Treatment modalities • Emollients (e.g., petrolatum) • Ultraviolet light • Coal tars (typically compounded) • Topical corticosteroids • Systemic corticosteroids (pulse dosing) • Antineoplastic agents (methotrexate, hydroxyurea) • Psoralens (pulse dosing) • Immunosuppressant agents (Etanercept, Efalizumab) • Retinoids (pulse dosing) PG 146 Which of the following psoriasis medications is not pregnancy category X? I. Dovonex II. Methotrexate III. Soriatane A. B. C. D. E. I only III only I and II only II and III only I, II and III Which of the following psoriasis medications is not pregnancy category X? I. Dovonex II. Methotrexate III. Soriatane A. B. C. D. E. I only III only I and II only II and III only I, II and III A patient presents to the pharmacy with obvious mild acne, which of the following cannot be recommended without a prescription? a. Benzoyl peroxide 2.5% cream b. Sulfur soap c. Benzamycin gel d. Salicylic acid wash e. Benzoyl peroxide 10% lotion A patient presents to the pharmacy with obvious mild acne, which of the following cannot be recommended without a prescription? a. Benzoyl peroxide 2.5% cream b. Sulfur soap c. Benzamycin gel d. Salicylic acid wash e. Benzoyl peroxide 10% lotion Fungal Infections Tinea corporis – body surface Tinea capitis – scalp Tinea cruris – groin (“jock itch”) Tinea pedis – feet (“athlete’s foot”) Onychomycosis – nails PG 67-68 and 147 Therapy Prophylaxis. Keep skin dry; frequent changes and thorough cleaning of clothing; and avoid likely areas of contamination. Active: Dusting powders (medicated versus nonmedicated), wet compresses Topical drug therapy • Fatty acids (undecylenic acid) • Tolnaftate (Tinactin, Aftate) • Haloprogin (Halotex) • Miconazole (Micatin,Monistat) • Clotrimazole (Lotrimin) • Oxiconazole (Oxistat) • Sulconazole (Exelderm) • Butenafine (Mentax) Nystatin (Mycostatin, Nilstat) – good for superficial candida (thrush) Systemic drug therapy for topical fungal disorders • Griseofulvin (microsized versus ultramicrosized) • Terbinafine (Lamisil) • Avoid corticosteroids PG 147 Antifungal Drugs (cont’d) Miconazole (Monistat, Micatin) – broad-spectrum antifungal agent available as powder, aerosol, cream, and suppository; may be used topically or vaginally Clotrimazole (Lotrimin, Mycelex) – broad-spectrum antifungal available as cream, lotion, suppositories, and troches (OTC use for 2 weeks after infection clears) Ketoconazole (Nizoral) – for superficial and systemic fungal infections; also available as OTC shampoo for dandruff; enzyme inhibitor Itraconazole (Sporanox) – for oral or topical treatment of superficial or systemic fungal disorders; enzyme inhibitor. - hepatotoxicity; take w/ food and avoid antacids PG 67 Antifungal Drugs (cont’d) Terbinafine (Lamisil) – used orally for onychomycosis of fingernail or toenail. Used topically for superficial tinea infections (OTC use for 1 week). Monitor for hepatoxicity with oral use. Ciclopriox (Penlac) – applied topically once daily for treatment of onychomycosis. – requires long-term therapy PG 67 Antifungal Drugs (cont’d) Griseofulvin (Grisactin, Grifulvin V, Fulvicin) For tinea only Duration of therapy • depends on type: corporis: 2-4 wks.; capitis: 4-6 wks., pedis: 4-8 wk Regular versus microsized versus ultramicrosized • ultra is better absorbed; take w/ fatty meal • causes induction interactions PG 67 Antifungal Drugs (cont’d) Other Azoles Posaconazole (Noxafil) Voriconazole (Vfend) • Reserved for severe invasive fungal infections (asperigillosis) PG 68 Echinocandins (less DI, but monitor LFTs) Anidulafungin (Eraxis) Caspofungin (Cancidas) Micafungin (Mycamine) Ampho B and related Lipid products nephrotoxicity NAPLEX Sample Questions Which of the following antibiotics does not have a significant drug interaction with warfarin? A. B. C. D. E. ciprofloxacin azithromycin TMP-SMZ Metronidazole Nafcillin Which of the following antibiotics does not have a significant drug interaction with warfarin? A. B. C. D. E. ciprofloxacin azithromycin TMP-SMZ Metronidazole Nafcillin Which of the following medications is the best treatment option for an uncomplicated urinary tract infection? A. B. C. D. E. penicillin cefuroxime levofloxacin gentamicin clarithromycin Which of the following medications is the best treatment option for an uncomplicated urinary tract infection? A. B. C. D. E. penicillin cefuroxime levofloxacin gentamicin clarithromycin Which of the following antimicrobial agents is available for parenteral use only? I. II. III. piperacillin aztreonam rifampin A. I only B. III only C. I and II only D. II and III only E. I, II and III Which of the following antimicrobial agents is available for parenteral use only? I. II. III. piperacillin aztreonam rifampin A. I only B. III only C. I and II only D. II and III only E. I, II and III Which of the following agents is a non-nucleoside reverse transcriptase inhibitor? A. B. C. D. E. didanosine delavirdine stavudine zidovudine lamivudine Which of the following agents is a non-nucleoside reverse transcriptase inhibitor? A. B. C. D. E. didanosine delavirdine stavudine zidovudine lamivudine Which of the following agents may be utilized in combination with other medications for H. pylori eradication? A. B. C. D. E. tetracycline azithromycin penicillin fluconazole cefuroxime Which of the following agents may be utilized in combination with other medications for H. pylori eradication? A. B. C. D. E. tetracycline azithromycin penicillin fluconazole cefuroxime Peripheral neuropathy is associated with which one of the following agents: A. B. C. D. E. nevirapine delavirdine Saquinavir Stavudine tenofovir Peripheral neuropathy is associated with which one of the following agents: A. B. C. D. E. Nevirapine (NNRTI) Delavirdine (NNRTI) Saquinavir (PI) Stavudine (NRTI) do not use with AZT (zidovudine) Tenofovir (NRTI) Administration of calcium or iron must be separated by at least 2 hours if antibiotics in this category are prescribed: I. II. III. Macrolides Tetracyclines Fluroquinolones A. I only B. III only C. I and II only D. II and III only E. I, II and III Administration of calcium or iron must be separated by at least 2 hours if antibiotics in this category are prescribed: I. II. III. Macrolides Tetracyclines Fluroquinolones A. I only B. III only C. I and II only D. II and III only E. I, II and III Which of the following antimicrobial agents has effective coverage for M. pneumoniae? A. B. C. D. E. amoxicillin erythromycin metronidazole cefotriaxone clindamycin Which of the following antimicrobial agents has effective coverage for M. pneumoniae? A. B. C. D. E. amoxicillin erythromycin metronidazole cefotriaxone clindamycin Which of the following regimens is most appropriate for C. difficile eradication? A. B. C. D. E. Clarithromycin 500 mg PO q 12 hours Clindamycin 300 mg IV q 6 hours Vancomycin 125 mg PO q 6 hours Doxycycline 100 mg PO q 12 hours Vancomycin 1000 mg IV q 12 hours Which of the following regimens is most appropriate for C. difficile eradication? A. B. C. D. E. Clarithromycin 500 mg PO q 12 hours Clindamycin 300 mg IV q 6 hours Vancomycin 125 mg PO q 6 hours Doxycycline 100 mg PO q 12 hours Vancomycin 1000 mg IV q 12 hours Which agent is available in both a topical and an oral product for the treatment of acne? I. II. III. clindamycin erythromycin doxycycline A. I only B. III only C. I and II only D. II and III only E. I, II and III Which agent is available in both a topical and an oral product for the treatment of acne? I. II. III. clindamycin erythromycin doxycycline A. I only B. III only C. I and II only D. II and III only E. I, II and III Which of the following drugs represents first (primary) agents in the treatment of TB? A. B. C. D. E. Ethambutol + PASA Ciprofloxacin + PASA Isoniazid + rifampin Cycloserine + streptomycin Penicillin + Benemid Which of the following drugs represents first (primary) agents in the treatment of TB? A. B. C. D. E. Ethambutol + PASA Ciprofloxacin + PASA Isoniazid + rifampin Cycloserine + streptomycin Penicillin + Benemid Which of the following antibiotics is considered first line treatment for a gonorrhea infection? A. B. C. D. E. Ampicillin Ciprofloxacin Doxycycline Penicillin Tetracycline Which of the following antibiotics is considered first line treatment for a gonorrhea infection? A. B. C. D. E. Ampicillin Ciprofloxacin (also..ceftriaxone, cefixime) Doxycycline (chlamydia) Penicillin Tetracycline Which of the following groups of antibiotics may be prescribed for a gravid patient with gonorrhea? I. II. III. cephalosporins fluoroquinolones tetracyclines A. I only B. III only C. I and II only D. II and III only E. I, II and III Which of the following groups of antibiotics may be prescribed for a gravid patient with gonorrhea? I. II. III. cephalosporins fluoroquinolones tetracyclines A. I only B. III only C. I and II only D. II and III only E. I, II and III A gravid patient with a Chlamydia infection is likely to be prescribed which of the following antibiotics? A. B. C. D. E. Ampicillin Levofloxacin Doxycycline Erythromycin Penicillin A gravid patient with a Chlamydia infection is likely to be prescribed which of the following antibiotics? A. B. C. D. E. Ampicillin Levofloxacin Doxycycline Erythromycin Penicillin Which of the following is the BEST treatment for a patient with herpes zoster? A. B. C. D. E. Cidofovir Famciclovir Ganciclovir Penciclovir Tenofovir Which of the following is the BEST treatment for a patient with herpes zoster? A. B. C. D. E. Cidofovir Famciclovir Ganciclovir Penciclovir Tenofovir Which of the following medications would be appropriate for the treatment of Pseudomonas aeruginosa? a. b. c. d. e. Ampicillin Cefepime Ceftriaxone Erythromycin Clindamycin Which of the following medications would be appropriate for the treatment of Pseudomonas aeruginosa? a. b. c. d. e. Ampicillin Cefepime Ceftriaxone Erythromycin Clindamycin