Skeletal Organization
advertisement

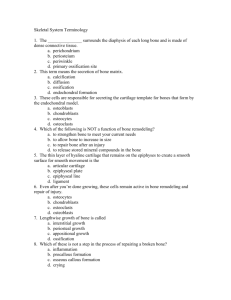
Skeletal Organization • Typically there are about 206 bones in the human skeleton • For convenience the skeleton is divided into the: • Axial skeleton • Appendicular skeleton 1 Divisions of the Skeleton Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Axial Skeleton • Skull • Spinal column • Ribs • Sternum • Hyoid bone Cranium Skull Face Hyoid Clavicle Scapula Sternum Humerus Ribs Vertebral column Vertebral column Hip bone Carpals Sacrum Radius Coccyx Ulna Femur Metacarpals • 80 bones Phalanges Patella Tibia Fibula Tarsals Metatarsals Phalanges (a) (b) 2 Divisions of the Skeleton Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Cranium Skull Face Hyoid Clavicle Scapula Sternum Humerus Ribs Vertebral column • Appendicular Skeleton • Upper limbs • Lower limbs • Shoulder girdle • Pelvic girdle Vertebral column Hip bone Carpals Sacrum Radius Coccyx Ulna Femur Metacarpals Phalanges Patella Tibia Fibula • 126 bones Tarsals Metatarsals Phalanges (a) (b) 3 7.3: Bone Development and Growth • Before week 8, the human embryonic skeleton is made of fibrous membranes and hyaline cartilage. • After week 8, bone tissue begins to replace the fibrous membranes and hyaline cartilage. – The development of bone from a fibrous membrane is called intramembranous ossification. Why? – The replacement of hyaline cartilage with bone is known as endochondral ossification. Why? Intramembranous Bones • Intramembranous Ossification • These bones originate within sheet-like layers of connective tissues (mesenchyme) • They are the broad, flat bones • Ex: Skull bones (except mandible), the facial bones, the clavicles, the pelvis and the scapulae 5 Endochondral Bones • Endochondral Ossification •Begins in the second month of development •Requires breakdown of hyaline cartilage prior to ossification •Bones begin as hyaline cartilage • Form models for future bones •These are most bones of the skeleton 6 Endochondral Ossification • Hyaline cartilage model • Primary ossification center • Secondary ossification centers • Epiphyseal plate • Osteoblasts vs. osteoclasts Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Cartilaginous model Developing periosteum Remnants of epiphyseal plates Secondary ossification center Compact bone developing Spongy bone Epiphyseal plates Blood vessel Calcified cartilage (a) (b) Medullary cavity (c) Medullary cavity Compact bone Medullary cavity Remnant of epiphyseal plate Epiphyseal plate Primary ossification center Secondary ossification center (d) Articular cartilage Spongy bone Articular cartilage (e) (f) 7 Endochondral Ossification 8 Osteogenesis - 10 week fetus Osteogenesis - 16 week fetus Video http://www.youtube.com/watch?v=78RBpWSOl08 Video http://www.youtube.com/watch?v=0dV1Bwe2v6c Lab Skull Lab Exercise 13 Catalyst Catalyst Catalyst Catalyst Criteria for SUCCESS!!! I will be able to: 1. Identify and describe the functions of the four layers of cells involved in growth at the epiphyseal plate. 2. List the steps in the process of bone reabsorption. 3. List the steps in the process of bone deposition. 4. List the steps in the process of appositional growth. 5. Identify 3 nutritional needs to maintain bone growth/maintenance. 6. List the effects of 4 hormones on bone growth. 7. Describe the causes and effects of two types of homeostatic imbalance disorders in bone. Growth at the Epiphyseal Plate Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • First layer of cells Bone tissue of epiphysis • Closest to the end of epiphysis • Resting cells • Anchors epiphyseal plate to epiphysis 1 Zone of resting cartilage 2 Zone of proliferating cartilage 3 Zone of hypertrophic cartilage • Second layer of cells 4 Zone of calcified cartilage • Many rows of young cells • Undergoing mitosis Ossified bone of diaphysis (a) (b) b: © The McGraw-Hill Companies, Inc./Al Telser, photographer 19 Growth at the Epiphyseal Plate Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. • Third layer of cells Bone tissue of epiphysis • Older cells • Left behind when new cells appear • Cells enlarging and becoming calcified 1 Zone of resting cartilage 2 Zone of proliferating cartilage 3 Zone of hypertrophic cartilage • Fourth layer of cells 4 Zone of calcified cartilage • Thin • Dead cells • Calcified extracellular matrix Ossified bone of diaphysis (a) (b) b: © The McGraw-Hill Companies, Inc./Al Telser, photographer 20 Homeostasis of Bone Tissue • Bone Resorption – action of osteoclasts via stimulation from parathyroid hormone (PTH) • Bone Deposition – action of osteoblasts and via stimulation from calcitonin Copyright © The McGraw-Hill Companies, Inc. Permission required for reproduction or display. Developing medullary cavity Osteoclast 21 © Biophoto Associates/Photo Researchers, Inc. Animation: Bone Growth in Width Please note that due to differing operating systems, some animations will not appear until the presentation is viewed in Presentation Mode (Slide Show view). You may see blank slides in the “Normal” or “Slide Sorter” views. All animations will appear after viewing in Presentation Mode and playing each animation. Most animations will require the latest version of the Flash Player, which is available at http://get.adobe.com/flashplayer. 22 Check out the mechanism of remodeling on the right! Why might you suspect someone whose been a powerlifter for 15 years to have heavy, massive bones, especially at the point of muscle insertion? Astronauts tend to experience bone atrophy after they’re in space for an extended period of time. Why? Long Bone Growth and Remodeling Figure 6.10 Nutritional Effects on Bone • Normal bone growth/maintenance cannot occur without sufficient dietary intake of calcium and phosphate salts. • Calcium and phosphate are not absorbed in the intestine unless the hormone calcitriol is present. Calcitriol synthesis is dependent on the availability of the steroid cholecalciferol (a.k.a. Vitamin D) which may be synthesized in the skin or obtained from the diet. • Vitamins C, A, K, and B12 are all necessary for bone growth as well. Hormonal Effects on Bone • Growth hormone, produced by the pituitary gland, and thyroxine, produced by the thyroid gland, stimulate bone growth. . Hormonal Effects on Bone • At puberty, the rising levels of sex hormones (estrogens in females and androgens in males) cause osteoblasts to produce bone faster than the epiphyseal cartilage can divide. This causes the characteristic growth spurt as well as the ultimate closure of the epiphyseal plate. • Estrogens cause faster closure of the epiphyseal growth plate than do androgens. • Estrogen also acts to stimulate osteoblast activity. At puberty, growth in bone length is increased dramatically by the combined activities of growth hormone, thyroid hormone, and the sex hormones. •As a result osteoblasts begin producing bone faster than the rate of epiphyseal cartilage expansion. Thus the bone grows while the epiphyseal plate gets narrower and narrower and ultimately disappears. A remnant (epiphyseal line) is visible on X-rays (do you see them in the adjacent femur, tibia, and fibula?) Calcitonin • Released by the C cells of the thyroid gland in response to high blood [Ca2+]. • Calcitonin acts to “tone down” blood calcium levels. • Calcitonin causes decreased osteoclast activity which results in decreased break down of bone matrix and decreased calcium being released into the blood. • Calcitonin also stimulates osteoblast activity which means calcium will be taken from the blood and deposited as bone matrix. Notice the thyroid follicles on the right. The arrow indicates a C cell Factors Affecting Bone Development, Growth and Repair • Deficiency of Vitamin A – retards bone development • Deficiency of Vitamin C – results in fragile bones • Deficiency of Vitamin D – rickets, osteomalacia • Insufficient Growth Hormone – dwarfism • Excessive Growth Hormone – gigantism, acromegaly • Insufficient Thyroid Hormone – delays bone growth •Physical Stress – stimulates bone growth 30 Animation: Bone Growth in Width Please note that due to differing operating systems, some animations will not appear until the presentation is viewed in Presentation Mode (Slide Show view). You may see blank slides in the “Normal” or “Slide Sorter” views. All animations will appear after viewing in Presentation Mode and playing each animation. Most animations will require the latest version of the Flash Player, which is available at http://get.adobe.com/flashplayer. 31 Homeostatic Imbalances Homeostatic Imbalances • Rickets – Bones of children are inadequately mineralized causing softened, weakened bones – Bowed legs and deformities of the pelvis, skull, and rib cage are common – Caused by insufficient calcium in the diet, or by vitamin D deficiency Homeostatic Imbalances Homeostatic Imbalances • Osteoporosis – Group of diseases in which bone reabsorption outpaces bone deposit – Spongy bone of the spine is most vulnerable – Occurs most often in postmenopausal women – Bones become so fragile that sneezing or stepping off a curb can cause fractures Animation: Osteoporosis Please note that due to differing operating systems, some animations will not appear until the presentation is viewed in Presentation Mode (Slide Show view). You may see blank slides in the “Normal” or “Slide Sorter” views. All animations will appear after viewing in Presentation Mode and playing each animation. Most animations will require the latest version of the Flash Player, which is available at http://get.adobe.com/flashplayer. 34