2) Examine her hands and wrists.
advertisement

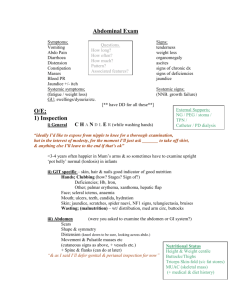
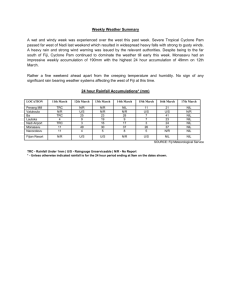
Case 1 - For Candidate Mrs. Felty has been having increasing problems moving the joints in her hands and wrists. 1) Take a psychosocial history. 2) Examine her hands and wrists. Case 1 - For Assessor/Patient Question for Candidate Mrs. Felty has been having increasing pain and stiffness in her hands and wrists. 1) Take a psychosocial history. 2) Examine her hands and wrists. History Name: Mrs. Annette Felty Psychosocial History Age: 50 Smoking: nil Presenting Complaint Alcohol: 1-2 glasses on wine on the 6 weeks ago - first noticed some weekend swelling in BOTH your wrists and the Recreational Drugs: nil MCP joint of your thumb. Occupation: Suit Tailor - working Wrists also feel stiff and are difficult frequently with very small needles, to move until you 'warm them up' buttons etc. The stiffness is a real which usually takes 45-60 mins. concern as you have just taken out a In the last month you have also been loan to start your own tailoring having a dull aching pain in both your business. wrists (Was 1/10 before but recently Husband runs his own plumbing 3 or 4/10 severity). business - works long hours. Pain, stiffness and swelling are all Home: Live with husband only. Two worst in the morning. daughters (20 and 25 y.o) both Pain improves slightly with Panadol moved out and live far away. and after moving the joints for a Love to knit and sew at home - joint morning. problems have stopped you recently. No joint locking/giving way or other systemic symptoms. Main Concern: Past Medical History Your main concern is that you may Childhood asthma have rheumatoid arthritis like your One previous hospital admission for a grandmother and scared that you will fractured radius during early 20s. have deformed hands like her and it Medications and Allergies will "ruin your life". Nil prescription medications. Allergic to eggs. Family History Grandmother with rheumatoid arthritis. Poorly controlled, severely deformed hands and wrists at end of her life. Your mother and your children at still all alive and well. Father died last year (age 78) from stroke. Case 1 - For Assessor/Patient Question for Candidate Mrs. Felty has been having increasing pain and stiffness in her hands and wrists. 1) Take a full psychosocial history. 2) Examine her hands and wrists. History Name: Mrs. Annette Felty Psychosocial History Age: 50 Smoking: nil Presenting Complaint Alcohol: 1-2 glasses on wine on the 6 weeks ago - first noticed some weekend swelling in BOTH your wrists and the Recreational Drugs: nil MCP joint of your thumb. Occupation: Suit Tailor - working Wrists also feel stiff and are difficult frequently with very small needles, to move until you 'warm them up' buttons etc. The stiffness is a real which usually takes 45-60 mins. concern as you have just taken out a In the last month you have also been loan to start your own tailoring having a dull aching pain in both your business. wrists (Was 1/10 before but recently Husband runs his own plumbing 3 or 4/10 severity). business - works long hours. Functional status: unable to sew and Home: Live with husband only. Two knit anymore daughters (20 and 25 y.o) both Pain, stiffness and swelling are all moved out and live far away. worst in the morning. Love to knit and sew at home - joint Pain improves slightly with Panadol problems have stopped you recently. and after moving the joints for a morning. Main Concern: No joint locking/giving way or other Your main concern is that you may systemic symptoms. have rheumatoid arthritis like your Past Medical History grandmother and scared that you will Childhood asthma have deformed hands like her and it will "ruin your life". One previous hospital admission for a fractured radius during early 20s. Medications and Allergies Nil prescription medications. Allergic to eggs. Family History Grandmother with rheumatoid arthritis. Poorly controlled, severely deformed hands and wrists at end of her life. Your mother and your children at still all alive and well. Father died last year (age 78) from stroke. Examination of the Hands and Wrists o o Position/Exposure Make sure that any jewellery or watches are removed. Patient should be exposed beyond the elbows and forearms on a pillow. Inspection Look on the dorsal surface and then palmar surface for: MCP positioning and alignment (knuckles) Muscle wasting o Easily seen at hypothenar and thenar eminences - can ask patient to turn hands onto palmar side and extend fingers. Swellings and deformities Scars (e.g. carpal tunnel release on wrist) Skin colour changes and nail abnormalities Asymmetry testing: Praying position - normal is ~90° Inverted pray position - normal is ~90° Look at the dorsum of the patients arms at the elbow Fleshy nodules may be present in RA Psoriatic lesions o Palpation and Movement Wrist Palpate bimanually Flex and extend passively Look for radial/ulnar deviation. MCPs Squeeze MCP joints from the side Palpate each joint individually for tenderness etc Assess passive movements of flexion and extension as you go PIPs/DIPs Palpate and move IP joints passively o Functional Assessment Grip Strength - get patient to squeeze two of your fingers in each hand Pincer Grip - thumb and index finger - try to force apart Opposition Strength - thumb and little finger - try to force apart Practical Test - undo a button/write with a pen Viva Questions: Can you tell me the normal range of movements of each hand and wrist joint? o Wrists Flexion/Extension - 75°; Radial/Ulnar Deviation - 20° o MCPs Flexion - 90°; Extension - 30°; Adduction/Abduction - 25° o PIPs - Flexion - 120°; DIPs - Flexion - 90° Do you think Mrs. Felty's history is more consistent with rheumatoid arthritis or osteoarthritis? What clinical features would you expect to find in the hands of someone with RA vs OA? RA OA Soft, boggy swellings of the wrists, MCPs and Hard, bony swelling of the PIPs, DIPs and 1st PIPs, with sparing of DIPs CMC Boutonniere's and Swan Neck Deformity Heberden's nodes (DIP) Z deformity of the thumb Bouchard's nodes (PIP) MCP ulnar deviation and palmar subluxation Osteophytes Case 2 - For Candidate DJ is applying for a job at Coles but must go through a check-up first. 1) Perform a checkup of DJ 2) Examine the oral cavity 3) Examine the lymph nodes of his head and neck, and state the appropriate landmarks. Case 2 - For Patient Question for Candidate DJ is applying for a job at coles but must go through a check-up first. 1) Perform a checkup of DJ 2) Examine the lymph nodes of his head and neck History Name: Mr DJ Ly Age: 22 Psychosocial History Smoking: nil Alcohol: 1-2 glasses of wine 3 nights a NOTE TO PATIENT: don’t tell student about depression or week and sometimes you have a bit suicide attempt unless specifically asked about it. more. If specifically asked what a “bit However please repeat how desperately you need this more” means, say 2 bottles of wine but job. that’s only happened twice. Been drinking since you started dating Main Concern: your girlfriend 4 years ago. You’re out of money and your girlfriend is about to Recreational Drugs: nil leave you for a guy named Vu. You REALLY need Occupation: Unemployed so you really this job. You’ve been depressed and have tried need this job! taking your life twice in the past by trying to drink Home: Lives with girlfriend who is a plain too much alcohol. clothes model and looks down on you for Keep emphasizing how desperately you need this having no job job. Sexual History: nil - never had sex. Presenting Complaint Travel History: nil You have no presenting complaint Feels unsupported emotionally and If asked “Why have you come to see me?”, explain financially that you need to get this checkout chick job at Diet: normal Coles, so you have to get a general check up done. Depression History (only say if specifically If asked open question about what’s wrong, just asked) say you feel fully healthy (e.g. “Have you noticed Only admit to feeling depressed, if any changes to your health recently?” “Nope, I feel specifically asked if you’ve been feeling fine”) “sad or depressed” Student should begin a systems review and start For the last 4 years, you’ve been feeling asking you associated symptoms. Deny all of them, sad, feeling guilty, you’ve lost interest in except trouble concentrating if specifically asked. your hobbies and have trouble Just say a little bit of trouble concentrating but concentrating you’ve had that for ages. Suicide History (only say if specifically asked) Past Medical History You believe life isn’t worth going on Had the flu a week ago but you think you’re all with/world would be better off without better now you No surgical history Have thought about taking your own life Only when specifically asked if you’ve been to You would do it by drinking yourself to hospital before, say you have twice for drinking a death. little bit too much. You have access to a lot of wine at home Medications and Allergies Have tried taking your own life twice by Nil prescription medications. drinking yourself to death with alcohol Taking multivitamins for general health. and that’s why you’ve been to hospital Allergic to penicillin; causes generalized rash twice Family History If asked how can they can help you, say: Mum has Hypertension, Diabetes type 1 and by passing you on this checkup Hypercholesterolaemia. Case 2 - For Assessor Question for Candidate DJ is applying for a job at coles but must go through a check-up first. 1) Perform a checkup of DJ 2) Examine the lymph nodes of his head and neck History Name: Mr DJ Ly Age: 22 NOTE TO PATIENT: don’t tell student about depression or suicide attempt unless specifically asked about it. However please repeat how desperately you need this job. INTRODUCTORY QUESTIONS Introduction Informed consent Ask if patient is comfortable (sitting, want to close curtains, etc.) Main Concern: Pt out of money and girlfriend is about to leave him for a guy named Vu. Pt REALLY needs this job. Has been depressed and has tried taking his life twice in the past by trying to drink too much alcohol. Presenting Complaint Asks last time patient felt fully well Performs full system Review Neuro o Headache or pain anywhere? o Changes in vision or hearing? o Changes in taste or smell? o Weakness, numbness or clumsiness? o Blackouts, fits, faints dizziness? o Vomiting or drowsy or nausea? o Memory or concentration? o Bladder or bowel problems? Cardiac o Chest pain or discomfort? o Pain in legs or anywhere else? o Ever aware of your own heart thumping? o Cold sweats? o Swelling in ankles? o Trouble breathing? Respiratory o Trouble breathing? o Wheeze or cough? o Chest discomfort or any pain elsewhere? o Fever, chills, sore muscles or joints? o Runny or blocked nose? o Trouble speaking or swallowing? Gastro o Any weight loss or changes to eating habits? o Vomiting, fever, fatigue? o Trouble swallowing or reflux? o Pain or bloating? o Changes to bowel habits? o Changes to urinary habits? o Discharges or itchiness from genitals? Musculoskeletal o Any swelling or pain? o Any joint locking up or giving way suddenly? o Any trouble moving? Past Medical History Had the flu a week ago. Now recovered. Must specifically ask about past surgeries or procedures: No surgical history Specifically ask if been to hospital before. Pt says twice for drinking a little bit too much. Points for asking how much pt drank Medications and Allergies Nil prescription medications. Taking multivitamins for general health (must remember to ask about over-thecounter medications and why they are taking it) Allergic to penicillin – generalized rash. MUST ask what type of allergic reaction they get! Family History Mum has Hypertension, Diabetes type 1 and Hypercholesterolaemia. Psychosocial History Suicide History (don’t give student hints to do Does some sort of a disclaimer e.g. “These this. Only tell them to do this, if they want to are just some questions we ask everyone start the examination) to get a better picture of what’s going on” Do you ever feel sad or depressed? Smoking: nil Do you ever feel like life isn’t worth going on with? Alcohol: 1-2 glasses of wine 3 nights a week and sometimes has a bit more. Have you ever thought about taking your own life? Must specifically ask what a “bit more” How would you take your own life? means: pt says 2 bottles of wine but that’s only happened twice. Do you have the resources/means to do Been drinking since dating girlfriend 4 that? years ago. Have you ever attempted to take your Recreational Drugs: nil life? Occupation: Unemployed Is there anything I can do for you at the moment? Home: Lives with girlfriend who is a plain clothes model and looks down on DJ for having no job Sexual History: nil - never had sex. Travel History: nil Must ask about feeling supported emotional AND THEN ask about feeling supported financially: Feels unsupported emotionally and financially Diet: normal Depression History (don’t give student hints to do this. Only tell them to do this, if they want to start the examination) Have you been feeling sad or even depressed? How long for? (more than 2 weeks is suspicious) Do you find you wake very early in the morning? Has your appetite been poor recently? Have you lost weight recently? How do you feel about the future? Have you had trouble concentrating on things? Have you had guilty thoughts? Have you lost interest in things you usually enjoy? Question for Candidate 1. How do the head and neck lymph nodes drain? Which drains most of the region? Detail its drainage. (Bloody $5 to the kid who can smash all this out without any help.) 2. What forms Waldeyer’s Ring? 3. Name the muscles that form the Palatine Arches? What are they innervated by? Answers 1. Occipital and post-auricular drain to superficial cervical then deep cervical. Everything else (i.e. pre-auricular, submandibular and submental) drain directly into deep cervical. All the lymph nodes eventually drain into the deep cervical lymph nodes. These nodes then drain into the left and right jugular trunks. The right jugular trunk then joins the thoracic duct. The thoracic duct then has the left subclavian trunk also join it; the left bronchiomediastinal trunk sometimes also joins it. The right jugular trunk then joins the right lymphatic duct. The right subclavian trunk also then joins the right lymphatic duct; the right bronchiomediastinal may also join. The right lymphatic duct and thoracic duct both empty in the junction of their respective internal jugular vein and subclavian veins, forming the brachiocephalic vein. Left and right brachiocephalic veins join to form the superior vena cava and empties into the right atrium. 2. Pharangeal tonsils, Palantine tonsils, Tubal tonsils and Lingual tonsils 3. Anterior one is known as the palatoglossal arch, which is formed by the palatoglossus. The posterior one is known as the palatopharyngeal arch and is formed by the Palatopharyngeus. Both muscles are innervated by the Vagus Nerve. Between these two arches is the palatine tonsil. Examination of the Oral cavity and Cervical Lymph Nodes Throat Examination General Inspection o Observe the: Lips, buccal mucosa, gums, palate and teeth - note any signs of inflammation such as erythema or swelling. Inspect the tongue in mouth and then poked out and then touched to roof of mouth (to inspect floor or tongue). o Ask patient to say "Ahh" and inspect oropharynx and uvula. Use a tongue depressor, if necessary, to obtain a better view of the pharynx. It is important that the depressor does not cause the patient to gag. o Inspect tonsils: size, shape, colour, discharge. Palpation o Full oral cavity examination should include palpation of the tongue for lumps (wearing gloves) as well as palpation of the salivary glands and cervical lymph nodes. The tonsils are part of the lymphatic system and should be examined when conducting a systematic examination of the lymphatic system. The examination of the oral cavity includes more than looking at the tonsils but the focus here is on examining the tonsils. Lymph Node Examination Position and Exposure o Patient should be sitting upright, both sides of neck are examined at same time. o Neck must be fully exposed including supraclavicular fossa - ideally shirts should be removed (bra for women can be left on but straps should be moved). General Inspection o Observe for: Swelling Asymmetry Scars o Ask about any tenderness present before proceeding with palpation. Palpation (see images below) o Use alcohol rub and warm hands. o A total of 8 lymph node regions should be palpated here: Submental Posterior to the inferior edge of the mental protuberance of the mandible and between the anterior bellies of both digastric muscle Submandibular Inferior to the body of the mandible Pre-auricular Just anterior to the tragus Post-auricular (mastoid) on the mastoid insertion of the Sternocleidomastoid muscle and inferior to the Auricularis posterior. Post-auricular node Occipital Near the insertion of the trapezius to the skull Resting on the insertion of the Semispinalis capitis (if you want to sound like a precise pro) Posterior Cervical triangle Formed by clavicle, trapezius (ant.) and sternocleidomastoid (post.) Palpate down to scalene node behind scalene insertion at clavicle. Anterior Cervical triangle (deep & superficial Cervical Lymph nodes) Formed by mandible, SCM (ant.) and the midline. Palpation here is for both superficial and deep anterior cervical chain nodes - deep nodes difficult to feel even when enlarged as they are deep to SCM, closely located to and around the neurovascular bundles. Supraclavicular fossae Ask patient to shrug their shoulders and feel behind the clavicle. Case 3 - For Candidate Mr. Clark is concerned about the recent changes in his urinary habits. 1) Take a full medical history and address his concerns. 2) Perform an abdominal examination. Case 3 - For Patient/Assessor Question for Candidate Mr. Clark is concerned about the recent changes in his urinary habits. 1) Take a full medical history and address his concerns. 2) Perform an abdominal examination. History Name: Mr. Maxwell Clark Age: 32 Occupation: Taxi Driver Medications and Allergies Regular medication for diabetes and but No allergies or non-prescription drugs. Presenting Complaint Burning sensation when peeing - began 3 days ago. Burning has become more and more painful since then. Since yesterday, you have also been experiencing some pain "low down on my bell" (suprapubic). When prompted you have also been experiencing: o That you need to pull over in your taxi while working to pee more often (frequency). o Been getting up a night more often to pee, never used to. o You don't get any warning, and just suddenly feel like you need to go. Awkward when you have a customer in your taxi. No fever, renal angle pain, or other urethral discharge. Travel History Nil Sexual history Married and committed to monogamous relationship. No engagement with sex workers, IVDU etc. Confident that wife is clean as a whistle too. Don't use contraception or condoms - wife is pregnant. Family History Brother with prostate cancer Father died of IHD in his 50s Mother died of ovarian cancer. Past Medical History Previously had 2 UTIs - only needed antibiotics once. The other time, you just drank a lot of water and it went away. Type II Diabetes Mellitus Both are managed well by regular medication that you can’t remember Psychosocial History Live with wife in a small one-bedroom apartment on third floor of a building. Alcohol - 2 beers a day usually, sometimes a few more on weekends (since 18 if pushed). Smoked 5 cigarettes a day in youth (from 18 to 25 if pushed). Nil recreational drugs. Taxi driver - work 10 shifts a week, long periods of time with no sleep and no break (not even to go to the toilet, "simply gotta tough it out"). No children, but wife is currently pregnant still in first trimester. Main Concern Your main concern is that your illness will prevent you from working the long hours you have been currently. This concerns you because you are already "on the ropes" financially and can't afford to stop working. Examination of the Abdomen Position and Exposure o Ask patient if he/she is comfortable to lie flat, with head on pillow, arms resting by sides → assists in relaxation of abdominal muscles. o Expose the abdomen from lower chest to pubic symphysis, inguinal ligament and iliac crest. Legs should be covered. General Inspection o Wasting (malignancy, alcoholic cirrhosis), pallor and jaundice (skin and scleral icterus →HCC damage or biliary obstruction causing hyperbilirubinaemia). o Make an obvious attempt to look around the immediate environment for any salient features (oxygen bottles, walkers etc). o Other symptoms: leukonychia (hypoalbuminaemia), clubbing, palmar erythema, bruising, scratch marks (pruritus), spider naevi, gynecomastia →chronic liver disease. o E.g. "On general inspection there does not appear to be any wasting, pallor..." Inspection of Abdomen o Look from above: Localised Swelling (enlargement of abdominal or pelvic organ, hernia) General Distension (fat, fluid (ascites), flatus (gaseous distension from bowel obstruction), faeces, 'filthy' tumour) Scars (laparascopic, nephrectomy, transplanted kidney or other). Other: caput Medusae, striae. o Look from abdominal level Repeat from abdominal level and ask patient to take slow deep breaths through their mouth and watch for asymmetrical movement indicating presence of a mass. o E.g. "On closer inspection of the abdomen there does not appear to be..." Systemic Palpation of Abdomen o Wash and warm hands first o Examine from the patient’s right side when possible. o Ask the patient if any part of their abdomen is painful and examine this part last. o Systematic light palpation of the abdominal quadrants for tenderness Ask the patient if anywhere is tender when you press it. Look at the patient's face to look for any response rather than at your hand. MCP movements only and forefinger lateral surface for organs and masses. o Systematic deep palpation of the abdominal quadrants for: Masses and/or enlarged organs (spleno, hepato, organo) Palpation and Percussion of Liver Palpation o o o o Begin in right lower quadrant/iliac fossa with hand parallel to right costal margin and lateral to lateral margin of rectus abdominis. Ask patient to breathe deeply and adjust hand during expiration to be ready during next inspiration. (Not too much pressure or lifting movement from liver is missed). Move up ~2cm if liver is not palpated and repeat until costal margin is reached. If liver is palpated, move along edge to xiphisternum until no longer palpable. o If not palpated, repeat process more laterally to detect Reidel's lobe. This is an extended, tongue-like right lobe of the liver. Percussion o Hand orientation and starting position same as palpation. Percuss softly in MCL. o Confirm sound change from resonant to dull with patient deep respiration. o Note of location of liver edge. o o o Percuss upper border beginning in 3rd IC space and percuss firmly down MCL. Confirm sound change with patient respiration. Measure liver span in MCL A normal liver span is 8-12cm (>13cm is abnormal) Palpation and Percussion of Spleen Palpation o o o o Left hand posterolaterally over left lower ribs and right hand beginning in below umbilicus in midlineTO and orientated obliquely towards axilla. Ask patient to breathe deeply and adjust hand during expiration to be ready during next inspiration. Hand moves upwards and laterally towards left hand. If spleen not palpated, patient rolls onto their right (towards examiner) and place left arm across upper chest if required - palpate again under costal margin. Spleen usually needs to be enlarged 1.5-2 times normal size to be palpated. Percussion Percussion for lower spleen pole in Traub's space (9th ICS anterior to anterior axillary line) → this should be resonant normally. Palpation of Kidneys o With patient still rolled over, place right hand in left renal angle (made by 12th rib and lateral margin of vertebral column). o Return patient to supine so they are resting on your right hand o Left hand placed anteriorly lining up with right hand (below costal margin and lateral to rectus abdominis). o As patient inspires deeply, flex at MCP of posterior hand and push in with top hand. o Repeat on other side with hands swapped. General Percussion o Performed to determine whether abdominal distension is due to gas or fluid (ascites). Ensure the patient is lying flat. o Percuss for flank dullness starting from midline and moving laterally to the left flank. Fingers should be parallel to rectus abdominis. o Dullness should not be detected until lateral abdominal wall. o If detected before lateral abdominal wall → test for shifting dullness. Note where dullness was detected early and roll patient onto right side. Wait 30 seconds Percuss at original point of dullness which should be resonant to confirm shifting dullness. Percuss further laterally to confirm shifting dullness and percuss medially to determine extent of shifting dullness. The absence of flank dullness is reliable sign for excluding ascites and hence not necessary to test for shifting dullness if there is no flank dullness. In contrast, flank dullness alone is not reliable enough to conclude ascites and therefore must test of shifting dullness. Auscultation o Warm the diaphragm of the stethoscope before auscultating. o Listen for bowel sounds: Due to peristalsis and can be heard anywhere in abdomen. Place stethoscope diaphragm below umbilicus and listen for at least 30 seconds before concluding that bowel sounds are absent. Report as absent or present. o Listen for arterial (aortic) bruits: Stethoscope diaphragm in midline 1cm above umbilicus to listen to AA. o Listen for renal bruits: 2.5cm lateral to site listened to for aortic bruit on either side. Viva Questions Given this man's history are there any other aspects of examination you would like to perform? o Urinalysis (then ask: what results will you be looking for? Leukocytes, nitrates, red blood cells, etc.) o Midstream urine (then what?) then send to lab for culture, staining and microscopy Can you describe the surface anatomy markings of the liver? o Liver upper border - horizontal line across 5th ribs o Liver lower border - oblique line from lowest point of right costal margin across to the left 5th rib in the midclavicular line. What is the normal liver span? o 8-12 cm in the MCL (>13 is considered hepatomegaly) Where do the kidneys normally lie? o Located retroperionteally o Lie in renal angle made from 12th rib and lateral margin of vertebral column o Kidneys extend from T12 to L2 with the right kidney slightly lower than the left kidney.