Basic Nursing:Foundations of Skills and Concepts Chapter 21
advertisement
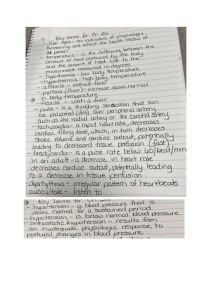
Basic Nursing:Foundations of Skills & Concepts Chapter 21 INFECTION CONTROL ASEPSIS Flora Microorganisms that occur or have adapted to live in a specific environment. Two types: Resident (always present). Transient (episodic). Pathogens Microorganisms that cause disease. These include: Bacteria. Fungi. Viruses. Protozoa. Rickettsia. Virulence The frequency with which a pathogen causes disease. Factors Affecting Virulence Strength of pathogen to adhere to healthy cells. Ability of pathogen to damage cells or interfere with the body’s normal regulating systems. Ability of pathogen to evade attack of white blood cells. Bacteria Small, one-celled microorganisms that lack a true nucleus or mechanism to provide metabolism. Only small percent of bacteria are pathogenic. Common bacterial infections include diarrhea, pneumonia, gonorrhea, meningitis, impetigo, and urinary tract infections. Viruses Organisms that live only inside cells. They cannot get nourishment or reproduce outside cells. Common viral infections include influenza, measles, common cold, chickenpox, hepatitis B, genital herpes, and HIV. Fungi Grow in single cells, as in yeast, or in colonies, as in molds. Most are not pathogenic and make up many of the body’s normal flora. Fungi can cause infections of the hair, skin, nails, and mucous membranes. Protozoa Single-celled parasitic organisms with the ability to move. Common protozoan infections include malaria, gastroenteritis, and vaginal infections. Rickettsia Intracellular parasites that need to be in living cells to reproduce. Spread through fleas, ticks, mites, and lice. Common rickettsia infections include typhus, Rocky Mountain spotted fever, and Lyme disease. Infection An invasion and multiplication of pathogenic microorganisms that occurs in body tissue and results in cellular injury. Chain of Infection Infectious agent Susceptible Host Reservoir Or Source Portal of Entry to Host Mode of Transmission Portal of Exit from Reservoir or Source Agent An entity capable of causing disease. These may be: Biological (bacteria, viruses, fungi, protozoa, Rickettsia). Chemical (pesticides, food additives, medications, industrial chemicals). Physical (environmental factors, like heat, light, noise, radiation, and machinery). Reservoir A place where the agent can survive. The most common reservoirs are: Humans. Animals. Environment. Fomites (objects contaminated with an infectious agent, e.g. bed pans, urinals, linens, instruments, dressings, etc.). Portal of Exit The route by which an infectious agent leaves the reservoir to be transferred to a susceptible host. Includes: Sputum from respiratory tract. Semen, vaginal secretions, or urine, from the genitourinary tract. Saliva and feces, from the gastrointestinal tract. Blood. Draining wounds. Tears. Modes of Transmission The process that bridges the gap between the portal of exit of the infectious agent from the reservoir or source and the portal of entry of the susceptible “new” host.Includes: Contact transmission (direct contact with infected person, indirect contact through fomite, or close contact with contaminated secretions). Airborne transmission. Vehicle transmission (through contaminated substances such as water, milk, drugs, or blood). Vectorborne transmission (through fleas, ticks, lice, and other animals). Host A simple or complex organism that can be affected by an agent. A susceptible host lacks resistance to an agent and is vulnerable to disease. A compromised host has impaired defense mechanisms and is susceptible to infection. Factors Affecting Susceptibility to Infection Age. Concurrent diseases. Stress. Immunization and vaccination status. Occupation. Nutritional Status. Heredity. Lifestyle. Breaking the Chain of Infection Between Agent and Resevoir Cleansing. Disinfection. Sterilizing. Cleansing The removal of soil or organic material from instruments and equipment. Four steps: Rinsing the object under cold water. Applying detergent and scrubbing object. Rinsing the object under warm water. Drying the object prior to sterilization or disinfection. Disinfection The elimination of pathogens, except spores, from inanimate objects. Disinfectants are chemical solutions used to clean inanimate objects. Germicides are chemicals that can be applied to both animate (living) and inanimate objects for the purpose of eliminating pathogens. Sterilization The total elimination of all microorganisms including spores. Instruments used for invasive procedures must be sterilized. Moist heat or steam, radiation, chemicals, and ethylene oxide gas used for sterilization. Autoclaving sterilization, using moist heat, is used in most hospital settings. Breaking the Chain of Infection Between Reservoir and Portal Proper Hygiene. Clean Dressings. Clean Linen. Clean Equipment. Breaking the Chain of Infection Between Portal of Exit and Mode of Transmission Clean dressings on all injuries. Clients should be encouraged to cover the mouth and nose when sneezing or coughing, as should the nurse. Gloves must be worn whenever necessary. Proper disposal of contaminated items. Breaking the Chain of Infection Between Mode of Transmission and Portal of Entry Nurses wearing barrier protection (gloves, masks, gowns, goggles). Proper handwashing. Proper disposal of contaminated equipment and linens. Breaking the Chain of Infection Between Portal of Entry and Host Maintaining skin integrity. Using sterile technique for client contacts. Avoiding needle sticks. Proper disposal of sharps. Breaking the Chain of Infection Between Host and Agent Proper nutrition. Exercise. Immunization. Normal Defense Mechanisms A host’s immune system serves as a normal defense mechanism against the transmission of infectious agents. Immune system recognizes presence of antigens, foreign proteins that cause the formation of an antibody. Nonspecific Immune Defense Skin and normal flora. Mucous membranes. Sneezing, coughing, and tearing reflexes. Elimination and acidic environment. Inflammation. Inflammation A nonspecific cellular response to tissue injury. Characteristics include: Redness (erythema). Heat. Pain. Swelling (edema). Loss of function. Pus (purulent exudate). Specific Immune Defense This is an immune defense mounted specifically against an invading antigen. Skin and normal flora. Mucous membranes. Sneezing, coughing, and tearing reflexes. Elimination and acidic environment. Inflammation. Stages of Infection Incubation (the time interval between entry of an infectious agent into host and onset of symptoms). Prodromal (from onset of nonspecific symptoms to specific symptoms of illness). Illness (period of specific signs and symptoms of infection). Convalescence (from disappearance of acute symptoms until client returns to previous state of health). Nosocomial Infections An infection acquired in a hospital or other health care facility that was not present or incubating at the time of the client’s admission. Also referred to as hospital-acquired infections. Asepsis The absence of microorganisms. Two types of asepsis: Medical (those practices used to reduce the number, growth, and spread of microorganisms). Surgical (practices that eliminate all microorganisms and spores from an object or area). Medical Asepsis Handwashing is the first line of defense against infection and is the single most important practice in preventing the spread of disease. Surgical Asepsis Techniques Surgical handwashing. Sterile field and equipment. Donning surgical attire. Donning sterile gloves. Gowning and closed gloving. Disposal of infectious materials.